The American Journal of Sports Medicine
advertisement

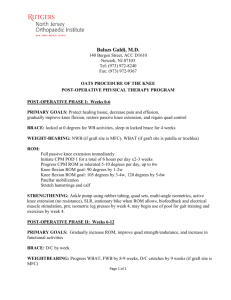
The American Journal of Sports Medicine http://ajs.sagepub.com/ Loss of Normal Knee Motion After Anterior Cruciate Ligament Reconstruction Is Associated With Radiographic Arthritic Changes After Surgery K. Donald Shelbourne, Scott E. Urch, Tinker Gray and Heather Freeman Am J Sports Med 2012 40: 108 originally published online October 11, 2011 DOI: 10.1177/0363546511423639 The online version of this article can be found at: http://ajs.sagepub.com/content/40/1/108 Published by: http://www.sagepublications.com On behalf of: American Orthopaedic Society for Sports Medicine Additional services and information for The American Journal of Sports Medicine can be found at: Email Alerts: http://ajs.sagepub.com/cgi/alerts Subscriptions: http://ajs.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav >> Version of Record - Jan 3, 2012 OnlineFirst Version of Record - Oct 11, 2011 What is This? Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 1, 2012 Loss of Normal Knee Motion After Anterior Cruciate Ligament Reconstruction Is Associated With Radiographic Arthritic Changes After Surgery K. Donald Shelbourne,*y MD, Scott E. Urch,y MD, Tinker Gray,y MA, and Heather Freeman,y PT, DHS Investigation performed at Shelbourne Knee Center, Indianapolis, Indiana Background: Meniscectomy and articular cartilage damage have been found to increase the prevalence of osteoarthritis after anterior cruciate ligament reconstruction, but the effect of knee range of motion has not been extensively studied. Hypothesis: The prevalence of osteoarthritis as observed on radiographs would be higher in patients who had abnormal knee range of motion compared with patients with normal knee motion, even when grouped for like meniscal or articular cartilage lesions. Study Design: Cohort study; Level of evidence, 3. Methods: We prospectively followed patients at a minimum of 5 years after surgery. The constant goal of rehabilitation was to obtain full knee range of motion as quickly as possible after surgery and maintain it in the long term. Range of motion and radiographs were evaluated at the time of initial return to full activities (early follow-up) and final follow-up according to International Knee Documentation Committee (IKDC) objective criteria. A patient was considered to have normal range of motion if extension was within 2° of the opposite knee including hyperextension and knee flexion was within 5°. Radiograph findings were rated as abnormal if any signs of joint space narrowing, sclerosis, or osteophytes were present. Results: Follow-up was obtained for 780 patients at a mean of 10.5 6 4.2 years after surgery. Of these, 539 had either normal or abnormal motion at both early and final follow-up. In 479 patients who had normal extension and flexion at both early and final follow-up, 188 (39%) had radiographic evidence of osteoarthritis versus 32 of 60 (53%) patients who had less than normal extension or flexion at early and final follow-up (P = .036). In subgroups of patients with like meniscal status, the prevalence of normal radiograph findings was significantly higher in patients with normal motion at final follow-up versus patients with motion deficits. Multivariate logistic regression analysis of categorical variables showed that abnormal knee flexion at early follow-up, abnormal knee extension at final follow-up, abnormal knee flexion at final follow-up, partial medial meniscectomy, and articular cartilage damage were significant factors related to the presence of osteoarthritis on radiographs. Abnormal knee extension at early follow-up showed a trend toward statistical significance (P = .0544). Logistic regression showed the odds of having osteoarthritis were 2 times more for patients with abnormal range of motion at final follow-up; these odds were similar for those with partial medial meniscectomy and articular cartilage damage. Conclusion: The prevalence of osteoarthritis on radiographs in the long term after anterior cruciate ligament reconstruction is lower in patients who achieve and maintain normal knee motion, regardless of the status of the meniscus. Keywords: anterior cruciate ligament; range of motion; meniscus; radiographs; long-term results tomy and articular cartilage damage.z A few studies have examined the association between loss of knee range of motion (ROM) and arthritic changes on radiographs. Roe et al21 stated that flexion contractures were associated with early osteoarthritic changes at a mean of 7 years after ACL reconstruction. Salmon et al23 found that loss of knee extension at 13 years after surgery and lateral or medial meniscectomy at the time of ACL reconstruction were related to a higher incidence of OA at follow-up. In a minimum 10-year follow-up study of 502 patients, Shelbourne and Gray27 found that patients who had less than normal ROM were about Several studies have established that major risk factors for the development of osteoarthritis (OA) after anterior cruciate ligament (ACL) reconstruction are meniscec*Address correspondence to K. Donald Shelbourne, MD, Shelbourne Knee Center, 1815 North Capitol Avenue, Indianapolis, IN 46202 (e-mail: tgray@aclmd.com). y Shelbourne Knee Center, Indianapolis, Indiana. Presented at the 37th annual meeting of the AOSSM, San Diego, California, July 2011. The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. The American Journal of Sports Medicine, Vol. 40, No. 1 DOI: 10.1177/0363546511423639 Ó 2012 The Author(s) z References 1, 5-8, 10, 13, 15, 17, 20, 21, 23, 25, 27, 28. 108 Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 1, 2012 Vol. 40, No. 1, 2012 ROM Loss and OA After ACL Reconstruction 2.5 times as likely to have abnormal radiograph findings as patients with normal ROM. Rehabilitation programs with ACL reconstruction have evolved through the years from restricting ROM after surgery for a determined amount of time to more current times when unrestricted ROM immediately after surgery is allowed and encouraged. Regardless of the rehabilitation plan for achieving full knee ROM, deficits in ROM compared with the opposite knee still exist in many patients after ACL reconstruction. The purpose of this study was to determine how knee ROM deficits would correlate with the prevalence of arthritic changes observed on radiographs after ACL reconstruction. We hypothesized that the prevalence of OA as observed on radiographs would be higher in a group of patients who had loss of normal knee ROM than in patients with normal knee ROM, even when grouped for like meniscal or articular cartilage abnormality. 109 Figure 1 To measure knee hyperextension, the heel of the foot is placed on a bolster so the knee can fall into hyperextension, if it is present. Knee range of motion is measured with a goniometer. MATERIALS AND METHODS Between 1987 and 2004, 3243 patients were prospectively enrolled in a long-term outcome study after ACL reconstruction with an autogenous patellar tendon graft. All patients gave informed consent to participate in the study, and the study was approved by the institutional review board. Patients were evaluated at regular intervals after surgery to include 2, 5, 10, and 20 years after surgery. Patients were excluded from this analysis if they had bilateral ACL injuries (n = 749), had arthritic changes on radiographs before surgery (n = 419), were deceased (n = 91), or had a subsequent ACL graft tear after surgery (n = 175). Of 1809 patients who met the criteria for the study, 780 patients had a minimum of 5 years of objective and subjective follow-up after surgery and are the focus of this study. At the time of surgery, an arthroscopic procedure was performed to evaluate and treat, if needed, any meniscal injuries or articular cartilage damage. The articular cartilage was graded for the femur and tibia in the medial and lateral compartments and for the patella according to the Outerbridge scale.19 Rehabilitation after surgery emphasized obtaining full knee ROM as soon as possible after surgery, and this program has been described previously.26,30 Knee ROM was evaluated with the patient lying supine and was measured with a goniometer as described by Norkin and White.16 The patient’s heel was elevated on a bolster to allow the knee to go into hyperextension if present (Figure 1). Knee flexion was measured by having the patient bend the knee to slide the heel toward the buttocks as far as possible. According to International Knee Documentation Committee (IKDC) criteria, normal knee extension is considered within 2° of the opposite normal knee, and normal flexion is considered to be within 5° of the opposite normal knee. Although IKDC criteria use 4 grades of normal, nearly normal, abnormal, and severely abnormal, we categorized knee extension and flexion as ‘‘abnormal’’ for any grade less than normal. Patients were also assigned an IKDC overall ROM rating, in which normal ROM was defined as the patient having both normal extension and flexion; abnormal was defined as the patient having less than normal extension or flexion. For this study, IKDC categories for ROM were evaluated at 2 time frames. The first time was when the patient was released to return to activities (early follow-up), and this time varied between patients depending on when they reached their rehabilitation goals. The mean time of this observation was 6.2 6 2.1 months after surgery. The second time when ROM data were evaluated was at the latest follow-up visit at greater than 5 years after surgery (final follow-up). Ligament stability was evaluated with a KT-1000 arthrometer, and the manual maximum difference between knees was measured. Radiographs obtained included bilateral knee views to include a 45° posteroanterior weightbearing view,22 Merchant view,14 and lateral view. Radiographs were graded according to criteria described by the IKDC.2 A grade of normal (A) means that there was no evidence of arthritic changes in the joint. A grade of nearly normal (B) indicates the presence of small osteophytes, slight sclerosis, flattening of the femoral condyles, and/or narrowing of the joint space that is just detectable. A grade of abnormal (C) indicates similar arthritic changes but also includes joint space narrowing up to 50% of the joint space. A grade of severely abnormal (D) indicated arthritic changes and includes joint space narrowing greater than 50%. Although the specific IKDC radiographic grade was recorded at the time of evaluation, we used only 2 categories of normal or abnormal in our analysis. If the knee was graded less than ‘‘A’’ in any compartment, it received a grade of abnormal for this analysis. Data Analysis Descriptive statistics were obtained. Multivariate logistic regression was performed on categorical variables, and univariate logistic regression was performed on continuous variables to determine their relationship to the presence of Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 1, 2012 110 Shelbourne et al The American Journal of Sports Medicine TABLE 1 Multivariate Logistic Regression Analysis of Categorical Variables Related to Radiographic Osteoarthritis at Follow-up Variable Early extension, abnormala Early flexion, abnormala Final follow-up extension, abnormal Final follow-up flexion, abnormal Medial meniscus removed Lateral meniscus removed Articular cartilage, abnormal Coefficient Standard Error P Value Odds Ratio 95% Confidence Interval .1077 .4616 .4913 .6268 .6339 .1858 .7423 .1513 .1788 .2246 .1796 .1472 .1768 .1722 .0544 .0098 .0287 .041 .0012 .294 \.01 1.1 1.6 1.9 1.8 1.8 1.1 2.1 0.83-1.5 1.1-2.3 1.3-2.9 1.3-2.6 1.4-2.5 0.85-1.7 1.5-2.9 a Early follow-up time when the patient was released to return to full activities. OA on radiographs at final follow-up. The x2 test was used to determine whether there was a statistically significant difference in the number of patients who had abnormal radiographic ratings based on whether they had an IKDC overall ROM rating of abnormal or normal ROM at both follow-up times. Further subanalysis was performed based on the status of the medial and lateral meniscus at the time of surgery or at the time of a subsequent arthroscopic procedure after ACL reconstruction, with the 4 categories being both menisci intact, partial medial meniscectomy, partial lateral meniscectomy, or partial medial and lateral meniscectomy. Subanalysis based on the status of the articular cartilage was performed by using 2 categories of normal (grade 2 or less in all compartments) or abnormal (grade 3 or 4 in any compartment). Statistical significance was set at P \ .05. The data were analyzed using Base SAS, SAS Access, and SAS Stat statistical software (SAS Institute, Cary, North Carolina). RESULTS The mean age for patients at the time of surgery was 25.4 6 9.2 years. The mean time for latest follow-up evaluation was 10.5 6 4.5 years (range, 5-21.2 years). The mean KT-1000 arthrometer manual maximum difference between knees was 1.9 6 1.3 mm, with 91% of patients with 3 mm, 8% with 4 to 5 mm, and 1% with .5 mm. At final follow-up, the IKDC rating for knee extension was ‘‘A’’ for 89% of patients, ‘‘B’’ for 10%, and ‘‘C’’ for 1%. The IKDC rating for knee flexion was ‘‘A’’ for 79% of patients, ‘‘B’’ for 16%, ‘‘C’’ for 3%, and ‘‘D’’ for 2%. The percentage of patients who had both normal knee extension and flexion was 68% at final follow-up. Ninety-two percent of patients had some degree of hyperextension (range, 1°14°), with the average being 5°. Thirty-three patients (4.2%) did not obtain at least 0° (neutral) knee extension. The IKDC category for overall ROM remained the same for 69% of patients from early follow-up to final follow-up (479 remained as normal, and 60 remained as abnormal). The overall IKDC ROM category changed from normal to abnormal in 13% (102 patients) and from abnormal to normal in 18% (139 patients). In 479 patients who had both normal extension and flexion from early to final follow-up, 188 (39%) had radiographic evidence of OA versus 32 of 60 (53%) patients who had less than normal extension or flexion throughout follow-up (P = .036). Multivariate logistic regression analysis of categorical variables showed that abnormal knee flexion at early follow-up, abnormal knee extension at final follow-up, abnormal knee flexion at final follow-up, partial medial meniscectomy, and articular cartilage damage were significant factors correlating with the presence of OA on radiographs (Table 1). Abnormal knee extension at early follow-up showed a trend toward statistical significance (P = .0544). The multivariate logistic regression analysis showed that ROM loss at final follow-up, partial medial meniscectomy, and articular cartilage damage each had about 2 times the odds of having OA. Univariate logistic regression analysis showed that older age at time of surgery (P \ .1) and longer follow-up time (P \ .01) were statistically significant factors correlating with OA on radiographs. In patients who had both menisci intact, the radiograph results were rated as normal in all joint compartments in 88% of patients versus 63% in patients who had both a medial and lateral meniscectomy (see the Appendix, available in the online version of this article at http:// ajs.sagepub.com/supplemental/). The percentage of patients with normal radiograph results was 69% in patients with normal knee extension at final follow-up and 70% in patients with normal knee flexion at final follow-up, which was statistically significantly higher than patients who had abnormal extension or flexion at final follow-up (P \ .001) (Figure 2). Overall, the percentage of patients who had normal radiograph results was 71% in patients with both normal extension and flexion (normal ROM) at final follow-up and 55% for patients who had any deficit in ROM at final follow-up (P \ .001). The percentage of patients who had normal radiograph results was statistically significantly higher for patients with normal ROM at final follow-up within each meniscus tear group (Figure 3). In the group of patients with normal articular cartilage at the time of surgery (n = 611), normal radiograph findings were found for 328 of 427 (77%) patients with normal ROM at final follow-up versus 114 of 184 (62%) patients with abnormal ROM (P \ .001). In patients with abnormal articular cartilage at the time of surgery (n = 169), normal radiograph results were found for 48 of 100 (48%) patients Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 1, 2012 Vol. 40, No. 1, 2012 100 90 80 70 60 50 40 30 20 10 0 % ROM Loss and OA After ACL Reconstruction Extension 69 Flexion 70 57 50 50 43 42 Normal Nearly Normal Abnormal Severely Abnormal Extension and Flexion Rating Figure 2 The number of patients with no evidence of osteoarthritis (normal radiographic rating) was statistically significantly higher in patients with normal extension and normal flexion versus those with less than normal range of motion ratings. (There were no patients who had a knee extension rating of severely abnormal.) 100 90 80 70 60 50 40 30 20 10 0 % Normal ROM* 77 74 67 Abnormal ROM* 56 56 41 38 24 Intact Medial Meniscectomy Lateral Medial and Lateral Meniscectomy Meniscectomy Meniscus Group Figure 3 There was a statistically significant difference in the number of patients with normal radiograph findings versus abnormal radiograph findings within each meniscus group: intact menisci (P = .01), medial meniscectomy (P = .035), lateral meniscectomy (P \ .01), and both medial and lateral meniscectomy (P = .021). ROM, range of motion. if they had normal ROM at final follow-up versus 25 of 69 (36%) patients with abnormal ROM (P = .12). DISCUSSION The results of this study showed that, when the factors of the meniscus status or articular cartilage damage are equalized, loss of normal knee ROM at final follow-up was associated with a higher prevalence of OA on radiographs in the long term. In patients with partial meniscectomy and/or articular cartilage damage, the loss of ROM was associated with a further increase in prevalence of OA. Furthermore, patients with loss of knee ROM of .5° of extension or .15° of flexion at final follow-up (IKDC ROM rating of abnormal or severely abnormal) had the highest prevalence of radiographic evidence of OA, as illustrated in Figure 2. The radiographic rating scale used in this study was the IKDC criteria. The IKDC scale is similar to the Kellgren 111 and Lawrence (K&L) classification system for grading radiographs.9 The IKDC classification of ‘‘B’’ is similar to K&L grade 2. The IKDC grade ‘‘C’’ is similar to K&L grade 3, and IKDC grade ‘‘D’’ is similar to K&L grade 4. Of studies evaluating posteroanterior weightbearing radiographs at 5 years or more after surgery and using the criteria for OA as either the IKDC radiographic grade of B, C, or D or the K&L grade of 2 or higher, the prevalence of OA in the long term after ACL reconstruction ranges from 18% to 80%.§ The major factors found to be related to a higher prevalence of OA in these studies were meniscectomy, time from injury to surgery, and articular cartilage damage. The wide range for the prevalence of radiographic OA between studies could be because of different follow-up times, the patients’ ages at the time of surgery, and the number of patients who underwent meniscectomy or who had existing OA before undergoing ACL reconstruction. The results of our study show that having a ROM deficit is a major factor associated with a higher prevalence of OA after ACL reconstruction. However, knee ROM in other studies is not always consistently evaluated or reported with regard to whether the measurement is compared to the noninvolved knee or whether knee hyperextension is included in the evaluation. Unless investigators specifically state how the patient was positioned and how ROM was measured, it is unknown whether knee hyperextension was included in the comparison between knees. Subtle differences for critically measuring passive knee hyperextension can be observed when the heels are placed on a bolster with the patient lying supine on the examination table. Another technique for observing differences in knee hyperextension is looking for heel height differences with the patient lying prone with his or her lower legs off the end of the examination table.24 However, patients with extension deficits are typically more uncomfortable in this position, and it is common for them to tilt their pelvis, which can affect the measurement. Another way to feel a difference in extension kinesthetically is to passively extend the patient’s knee by holding the thigh in place with one hand and using the other hand to hold the ball of the foot to lift the heel off the examination table (Figure 4). The average degree of hyperextension in normal knees is 6° in women and 5° in men, and 95% of people have some degree of hyperextension in their knees.4 The results in our study showed that 92% of patients had some degree of hyperextension, with the average being 5°. If passive hyperextension is not included as part of a regular physical examination, the subtle difference of 3° to 5° between knees (IKDC grade ‘‘B’’) may not be observed. Questions that are difficult to answer are did the ROM deficit contribute to OA or did the development of OA cause a ROM deficit? Salmon et al,23 in a study that evaluated patients at 5, 7, and 13 years after ACL reconstruction, found an increase in the percentage of patients who had a loss of normal knee extension from 2% at 5 years postoperatively to 44% at 13 years postoperatively. Similarly, the percentage of patients who had a loss of normal knee flexion increased § References 1, 11, 17, 18, 20, 23, 27, 28. Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 1, 2012 112 Shelbourne et al The American Journal of Sports Medicine Figure 4 To feel a difference in extension kinesthetically, the examiner passively extends the patient’s knee by holding the thigh in place with one hand and using the other hand to hold the ball of the foot to lift the heel off the examination table. from 6% at 5 years to 21% at 13 years after surgery. They also found a progression of OA with greater time after surgery, and a regression analysis determined that the loss of knee extension was a factor related to OA.23 Conversely, we found that very few patients (13%) lost knee ROM from the time they were released to activities to the time of final follow-up, and there were more patients (18%) who had ROM deficits early that improved to the normal category at follow-up. The prevalence of OA in this current study was statistically significantly higher (53%) for patients who had an overall IKDC ROM grade of abnormal at both early and final follow-up compared with patients who maintained an overall IKDC ROM grade as normal (39%). This finding leads us to believe that ROM deficits that a patient has early after surgery and continues to have with time may contribute to OA in the long term. The multivariate logistic regression analysis showed that abnormal knee extension at final follow-up and abnormal knee flexion at both early and final follow-up were equally as significant as having a partial medial meniscectomy, with patients having almost 2 times the odds of having OA. The most important factor in the regression model was damaged articular cartilage with 2.1 times the odds of developing OA. While each of these factors is important, rehabilitation to achieve normal knee ROM may be easier to achieve than controlling the status of the meniscus or articular cartilage. Most rehabilitation programs today with ACL reconstruction ‘‘allow’’ full ROM immediately after surgery. However, there is a difference between allowing full ROM and emphasizing that full ROM needs to be obtained to achieve the optimal outcome after surgery. The senior author has used the ‘‘accelerated’’ rehabilitation program30 after ACL reconstruction since 1987; however, the program was meant to accelerate the return of ROM and strength, and the quicker return to sports was a direct result of patients achieving those 2 specific rehabilitation goals. Regardless of the time restriction surgeons decide is appropriate for their patients to return to activities, the goal of achieving full knee ROM, to include hyperextension, can be a common goal for all because patients who achieve full ROM and maintain it through time may have less OA in the long term. Throughout the years of the study, the methods used to achieve full knee ROM were refined. We believe that there were 2 main factors that helped patients achieve full ROM after surgery: (1) delaying surgery after an acute injury so patients could perform rehabilitation exercises to obtain full ROM before surgery and (2) limiting the development of a hemarthrosis after surgery. The protocol to limit a hemarthrosis and pain after surgery has been described26,29 and includes adequate pain control with intravenous ketorolac and cold/compression with elevation of the knee. An advantage to limiting a hemarthrosis is that hemarthrosis can cause a quadriceps muscle shutdown, which further complicates obtaining terminal knee extension and achieving good leg control. The goal of limiting an intra-articular hemarthrosis or effusion was central to the progression of rehabilitation during the first year after surgery. If a patient experienced increased swelling with increased exercises or activities, he or she was told to reduce the level of activity to eliminate the swelling and to make sure full knee ROM was maintained. Surgical procedures are being done with the intent to prevent or minimize the development of OA after ACL reconstruction, and the major surgical efforts being performed include double-bundle ACL reconstruction, meniscal transplant, and articular cartilage repair or restoration.3,12,31 Given the results of this current study showing that even a 3° to 5° extension loss or 5° flexion loss can be associated with the prevalence of OA in the long term, the results of these other surgical procedures to reduce OA should also include a critical evaluation of knee ROM as a factor for success or failure from surgery. A limitation of this study is that we had 5-year objective follow-up on 43% of patients. While, ideally, we would like to achieve long-term follow-up on all patients, this goal is difficult to achieve in clinical practice. However, a previous study28 of our patient population showed that the subjective results of patients who could not return for long-term objective evaluation were not statistically significantly different than the patients who did return. Therefore, we believe the results of this study show a representative sample of our total patient population. CONCLUSION The data in this study show that the prevalence of OA on radiographs in the long term after ACL reconstruction is lower in patients who achieve and maintain normal knee ROM after ACL reconstruction, regardless of the status of the meniscus. Proper perioperative rehabilitation to achieve normal knee ROM may reduce the effect of partial meniscectomy for developing OA after surgery. ACKNOWLEDGMENT We thank Kanitha Phalakornkule, MS, for her statistical analysis of the data. Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 1, 2012 Vol. 40, No. 1, 2012 ROM Loss and OA After ACL Reconstruction REFERENCES 1. Ait Si Selmi T, Fithian D, Neyret P. The evolution of osteoarthritis in 103 patients with ACL reconstruction at 17 years follow-up. Knee. 2006;13:353-358. 2. American Orthopaedic Society for Sports Medicine. 2000 International Knee Documentation Committee Knee Evaluation Form. Available from: http://www.sportsmed.org/research/docs/IKDC%202000-Revised%20Subjective%20Scoring.doc. Accessed September 25, 2008. 3. Cole BJ, Carter TR, Rodeo SA. Allograft meniscal transplantation: background, techniques and results. Instr Course Lect. 2003;52:383-396. 4. DeCarlo MS, Sell KE. Normative data for range of motion and singleleg hop in high school athletes. J Sport Rehabilitation. 1997;6:246-255. 5. Hertel P, Behrend H, Cierpinski T, Musahl B, Widjaja G. ACL reconstruction using bone-patellar tendon-bone press-fit fixation: 10-year clinical results. Knee Surg Sports Traumatol Arthrosc. 2005;13:248-255. 6. Ichiba A, Kishimoto I. Effects of articular cartilage and meniscus injuries at the time of surgery on osteoarthritic changes after anterior cruciate ligament reconstruction in patients over 40 years old. Arch Orthop Trauma Surg. 2009;129:409-415. 7. Jarvela T, Nyyssonen M, Kannus P, Paakkala T, Jarvinen M. Bonepatellar tendon-bone reconstruction of the anterior cruciate ligament: a long-term comparison of early and late repair. Int Orthop. 1999;23:227-231. 8. Jomha NM, Borton DC, Clingeleffer AJ, Pinczewski LA. Long-term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res. 1999;358:188-193. 9. Kellgren JH, Lawrence JS. Radiological assessment of osteoarthrosis. Ann Rheum Dis. 1957;16(4):494-502. 10. Kocher MS, Steadman JR, Briggs K, Zurakowski D, Sterett WI, Hawkins R. Determinants of patient satisfaction with outcome after anterior cruciate ligament reconstructions. J Bone Joint Surg Am. 2002;84:1560-1572. 11. Lebel B, Hulet C, Galaud B, Burdin G, Locker B, Vielpeau C. Arthroscopic reconstruction of the anterior cruciate ligament using bonepatellar tendon-bone autograft. Am J Sports Med. 2008;36:1275-1282. 12. Levy AS, Meier SW. Approach to cartilage injury in the anterior cruciate ligament-deficient knee. Orthop Clin North Am. 2003;34(1):149-167. 13. Liden M, Ejerhed L, Sernert N, Laxdal G, Kartus J. Patellar tendon or semitendinosus tendon autografts for anterior cruciate ligament reconstruction: a prospective, randomized study with a 7-year follow-up. Am J Sports Med. 2007;35:740-748. 14. Merchant AC. Patellofemoral malalignment and instabilities. In: Ewing JW, ed. Articular Cartilage and Knee Joint Function: Basic Science and Arthroscopy. New York: Raven Press; 1990:79-91. 15. Neuman P, Englund M, Kostogiannis I, Friden T, Roos H, Dahlberg LE. Prevalence of tibiofemoral osteoarthritis 15 years after nonoperative treatment of anterior cruciate ligament injury: a prospective cohort study. Am J Sports Med. 2008;36:1717-1725. 16. Norkin CC, White DJ. Measurement of Joint Motion: A Guide to Goniometry. 3rd ed. Philadelphia: FA Davis Co; 2003. 113 17. Øiestad BE, Holm I, Aune AK, et al. Knee function and prevalence of knee osteoarthritis after anterior cruciate ligament reconstruction: a prospective study with 10-15 years of follow-up. Am J Sports Med. 2010;38:2201-2210. 18. Øiestad BE, Holm I, Engebretsen L, Risberg MA. The association between radiographic knee osteoarthritis and knee symptoms, function, and quality of life 10-15 years after anterior cruciate ligament reconstruction. Br J Sports Med. 2011;45(7):583-588. 19. Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br. 1961;43:752-757. 20. Pinczewski LA, Lyman J, Salmon LJ, Russell VJ, Roe J, Linklater J. A 10-year comparison of anterior cruciate ligament reconstructions with hamstring tendon and patellar tendon autograft: a controlled, prospective trial. Am J Sports Med. 2007;35:564-574. 21. Roe J, Pinczewski LA, Russell VJ, Salmon LJ, Kawamata T, Chew M. A 7-year follow-up of patellar tendon and hamstring tendon grafts for arthroscopic anterior cruciate ligament reconstruction: differences and similarities. Am J Sports Med. 2005;33:1337-1345. 22. Rosenberg TD, Paulos LE, Parker RD, Coward DB, Scott SM. The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg Am. 1988;70:1479-1483. 23. Salmon LJ, Russell VJ, Refshauge K, et al. Long-term outcome of endoscopic anterior cruciate ligament reconstruction with patellar tendon autograft: minimum 13-year review. Am J Sports Med. 2006;34:721-732. 24. Schlegel TF, Boublik M, Hawkins RF, Steadman JR. Reliability of heel height measurement for documenting knee extension deficits. Am J Sports Med. 2002;30:479-482. 25. Segawa H, Omori G, Koga Y. Long-term results of non-operative treatment of anterior cruciate ligament injury. Knee. 2001;8:5-11. 26. Shelbourne KD, Gray T. Anterior cruciate ligament reconstruction with autogenous patellar tendon graft followed by accelerated rehabilitation: a two- to nine-year followup. Am J Sports Med. 1997;25:786-795. 27. Shelbourne KD, Gray T. Minimum 10-year results after anterior cruciate ligament reconstruction: how the loss of normal knee motion compounds other factors related to the development of osteoarthritis after surgery. Am J Sports Med. 2009;37:471-480. 28. Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery: five- to fifteen-year evaluations. Am J Sports Med. 2000;28:446-452. 29. Shelbourne KD, Liotta FJ, Goodloe SL. Preemptive pain management program for anterior cruciate ligament reconstruction. Am J Knee Surg. 1998;11:116-119. 30. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. Am J Sports Med. 1990;18:292-299. 31. Stergiou N, Ristanis S, Moraiti C, Georgoulis AD. Tibial rotation in anterior cruciate ligament (ACL)-deficient and ACL-reconstructed knees: a theoretical proposition for the development of osteoarthritis. Sports Med. 2007;37(7):601-613. For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav Downloaded from ajs.sagepub.com at UNIV OF DELAWARE LIB on May 1, 2012