N [ research
advertisement

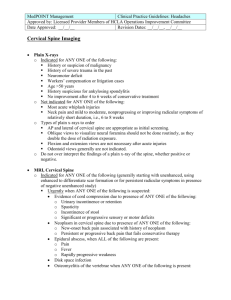
[ ] research report EMILIO J. PUENTEDURA, PT, DPT1 • MERRILL R. LANDERS, PT, DPT2 • JOSHUA A. CLELAND, PT, PhD3 PAUL MINTKEN, PT, DPT4 • PETER HUIJBREGTS, PT, DPT5 • CESAR FERNANDEZ-DE-LAS-PEÑAS, PT, DO, PhD6 Thoracic Spine Thrust Manipulation Versus Cervical Spine Thrust Manipulation in Patients With Acute Neck Pain: A Randomized Clinical Trial TTSTUDY DESIGN: Randomized clinical trial. TTOBJECTIVE: To determine if patients who met the clinical prediction rule (CPR) criteria for the success of thoracic spine thrust joint manipulation (TJM) for the treatment of neck pain would have a different outcome if they were treated with a cervical spine TJM. TTBACKGROUND: A CPR had been proposed to identify patients with neck pain who would likely respond favorably to thoracic spine TJM. Research on validation of that CPR had not been completed when this trial was initiated. In our clinical experience, though many patients with neck pain responded favorably to thoracic spine TJM, they often reported that their symptomatic cervical spine area had not been adequately addressed. TTMETHODS: Twenty-four consecutive patients, who presented to physical therapy with a primary complaint of neck pain and met 4 out of 6 of the CPR criteria for thoracic TJM, were randomly assigned to 1 of 2 treatment groups. The thoracic group received thoracic TJM and a cervical rangeof-motion (ROM) exercise for the first 2 sessions, followed by a standardized exercise program for an additional 3 sessions. The cervical group received cervical TJM and the same cervical ROM exercise for the first 2 sessions, and the same exercise program given to the thoracic group for the next 3 sessions. Outcome measures collected at 1 week, 4 weeks, and 6 months from start of treatment included the Neck Disability Index, numeric pain rating scale, and Fear-Avoidance Beliefs Questionnaire. TTRESULTS: Patients who received cervical TJM demonstrated greater improvements in Neck Disability Index (P.001) and numeric pain rating scale (P.003) scores at all follow-up times. There was also a statistically significant improvement in the Fear-Avoidance Beliefs Questionnaire physical activity subscale score at all follow-up times for the cervical group (P.004). The number needed to treat to avoid an unsuccessful overall outcome was 1.8 at 1 week, 1.6 at 4 weeks, and 1.6 at 6 months. TTCONCLUSION: Patients with neck pain who met 4 of 6 of the CPR criteria for successful treatment of neck pain with a thoracic spine TJM demonstrated a more favorable response when the TJM was directed to the cervical spine rather than the thoracic spine. Patients receiving cervical TJM also demonstrated fewer transient side-effects. TTLEVEL OF EVIDENCE: Therapy, level 1b. J Orthop Sports Phys Ther 2011;41(4):208-220, Epub 18 February 2011. doi:10.2519/jospt.2011.3640 TTKEY WORDS: clinical prediction rule, manual therapy, mobilization, prognosis N eck pain is a common complaint within the general population, and one that over 50% of individuals report having experienced at some point in their lives. 3,4 While 12-month prevalence rates for neck pain SUPPLEMENTAL VIDEO ONLINE are estimated to be between 30% and 50%, disabling neck pain is less common, with estimated 12-month prevalence rates of 2% to 11%.22 Individuals with significant neck pain often have considerable disability, resulting in substantial economic hardship. Neck pain is most often managed conservatively and frequently by referral to physical therapy.27 Physical therapists commonly approach the clinical management of patients with neck pain by incorporating manual therapy interventions directed to the cervical spine. These manual therapy techniques include passive joint mobili- Assistant Professor, Department of Physical Therapy, School of Allied Health Sciences, University of Nevada Las Vegas, Las Vegas, NV. 2Associate Professor, Department of Physical Therapy, School of Allied Health Sciences, University of Nevada Las Vegas, Las Vegas, NV. 3Professor, Department of Physical Therapy, Franklin Pierce University, Concord, NH. 4Assistant Professor, Department of Physical Therapy, School of Medicine, University of Colorado, Aurora, CO. 5In memoriam, Assistant Professor, University of St Augustine for Health Sciences, St Augustine, Florida; Clinical Consultant, Shelbourne Physiotherapy Clinic, Victoria, British Columbia, Canada. 6Professor, Department of Physical Therapy, Occupational Therapy, Rehabilitation and Physical Medicine, Universidad Rey Juan Carlos, Alcorcón, Madrid, Spain. This clinical trial received full board approval from The University of Nevada Las Vegas, Office for the Protection of Human Research Subjects. Address correspondence to Dr Emilio J. Puentedura, Assistant Professor, University of Nevada Las Vegas, School of Allied Health Sciences, Department of Physical Therapy, 4505 Maryland Parkway, Box 453029, Las Vegas, NV, 89154-3029. E-mail: louie.puentedura@unlv.edu 1 208 | april 2011 | volume 41 | number 4 | journal of orthopaedic & sports physical therapy 41-04 Puentedura.indd 208 3/16/2011 12:57:01 PM zation (nonthrust techniques) and thrust joint manipulation (TJM). Although there is solid evidence to support manual therapy directed at the cervical spine in patients with neck pain,5-7,10,23,30 physical therapists may be reluctant to apply TJM to the cervical spine because of perceived risks associated with thrust techniques applied to this region.1,8,17,28 Recent research has shown that TJM directed to the thoracic spine provides a therapeutic benefit to some patients with neck pain13 and has been suggested as an appropriate strategy to minimize the risks associated with manipulation of the cervical spine. Despite this, cervical spine TJM continues to be provided to patients with neck pain30 and is recommended in patients with cervicogenic headache.7 In their derivation study, Cleland et al12 developed a clinical prediction rule (CPR) to identify a subgroup of patients with neck pain who were more likely to benefit from thoracic spine TJM. In that study, the researchers treated all patients with thoracic spine TJM and a general range-of-motion (ROM) exercise and using a logistic regression model, identified the common characteristics (prognostic variables) of patients who met the criteria for treatment success. These prognostic variables were used to define the CPR; however, more recent evidence has questioned its validity.15 A regional interdependence approach to the treatment of patients with neck pain is gaining support both clinically and in published research reports.2,39,41,42,45 While treatment of the thoracic spine in these patients has demonstrated benefits and involves arguably less risk, it may not completely address the symptoms and mobility impairments with which these patients present. It has been our experience that adding cervical manipulation to a comprehensive management approach improves clinical outcomes. The purpose of this randomized clinical trial was to determine the differences in outcome using cervical spine TJM compared to thoracic spine TJM to treat patients with neck pain who met the criteria for the CPR. METHODS Participants C onsecutive patients with a primary complaint of neck pain, who presented to physical therapy between December 2008 and April 2010, were screened for eligibility. To be eligible to participate, patients had to be between 18 and 60 years of age, have a primary report of neck pain with or without unilateral upper extremity symptoms, and have a baseline Neck Disability Index (NDI) score of 10/50 points or greater. Additional inclusion and exclusion criteria for this trial were based on those used by Cleland et al12 in their CPR derivation study. Finally, patients had to satisfy at least 4 out of the following 6 criteria: symptom duration less than 30 days, no symptoms distal to the shoulder, no aggravation of symptoms by looking up, Fear-Avoidance Beliefs Questionnaire Physical Activity (FABQPA) subscale score of less than 12, decreased upper thoracic spine kyphosis (T3-T5), and cervical extension range of motion (ROM) less than 30°. Exclusion criteria included any serious pathology (such as neoplasm), a diagnosis of cervical spinal stenosis (as identified in the patients’ medical intake form) or bilateral upper extremity symptoms, evidence of central nervous system involvement, 2 or more positive neurologic signs consistent with nerve root compression (changes in sensation, myotomal weakness, or decreased deep tendon reflexes), pending legal action regarding their neck pain, a history of whiplash injury within 6 weeks of the examination, or any history of cervical spine surgery, rheumatoid arthritis, osteoporosis, osteopenia, or ankylosing spondylitis. The study was approved by the University of Nevada Las Vegas Biomedical Institutional Review Board. All individuals provided informed consent prior to their participation. INTERVENTIONS Examination P rior to randomization, all patients underwent a standardized history and physical examination. Demographic information collected included age, sex, mechanism of injury (if any), location and nature of symptoms, and the number of days since onset of symptoms. The historical examination included follow-up questions regarding aggravating and relieving factors, 24hour behavior of presenting symptoms, and any prior history of neck pain. The physical examination followed the same protocol as that described by Cleland et al,12 beginning with a neurological screen,18 followed by postural assessment.29 Cervical ROM was measured and symptom response assessed, followed by assessments of muscle length and strength. The amount of motion and symptom response were recorded for segmental passive intervertebral mobility testing18 of the cervical spine and passive accessory intervertebral mobility testing32 of the cervical and thoracic spine (C2-T9). The physical examination was then concluded with a number of special tests typically performed in the examination of patients with neck pain, including Spurling’s test,38 the neck distraction test,44 and the median neurodynamic test (MNT). 35 Patients were also screened for any signs of vertebrobasilar insufficiency (VBI), such as nystagmus, gait disturbances, and Horner’s syndrome, as well as screening for upper cervical spine ligamentous laxity through the Sharp-Purser test, alar ligament stress test, and transverse ligament tests.11 Patients who had a positive finding on any of these final screening tests were excluded from the study. Outcome Measures All patients completed several commonly used instruments to assess pain and perceived disability. The Neck Disability Index (NDI) is the most widely used condition-specific disability scale for patients journal of orthopaedic & sports physical therapy | volume 41 | number 4 | april 2011 | 209 41-04 Puentedura.indd 209 3/16/2011 12:57:02 PM [ with neck pain,15 and consists of 10 items addressing different aspects of function, each scored from 0 to 5, with a maximum possible score of 50 points.40 The NDI has been reported to be a reliable and valid outcome measure for patients with neck pain.21,36,40,46 In a recent systematic review of the literature, MacDermid et al31 concluded that the minimal detectable change (MDC) for the NDI is 5 points out of 50, whereas 7 points out of 50 was recommended for the minimal clinically important difference (MCID). To measure pain intensity, we used an 11-point numeric pain rating scale (NPRS),25,26,34 ranging from 0 (“no pain”) to 10 (“worst imaginable pain”). Patients were asked to rate their current level of pain, and their worst and least amount of pain in the preceding 24 hours, and the 3 ratings were averaged to represent the patient’s level of pain. The MDC and MCID for the NPRS have been reported as 2.1 and 1.3 points, respectively.14 The Fear-Avoidance Beliefs Questionnaire (FABQ) is a 16-item questionnaire designed to quantify fear and avoidance beliefs in patients with low back pain.43,47 The FABQ has 2 subscales: a 4-item scale to measure fear-avoidance beliefs about physical activity (FABQ-PA) and a 7-item scale to measure fear-avoidance beliefs about work (FABQ-W). Each item of the FABQ-PA and FABQ-W is scored from 0 to 6, with possible scores on the FABQ-PA raging from 0 to 24 and on the FABQ-W from 0 to 42, and higher scores representing increased fear-avoidance beliefs. As in previous studies, the FABQ was modified by replacing the word “back” with the word “neck.”12,15 Currently, there are few published estimates for the MDC and MCID of the FABQ. Grotle et al20 reported an MDC of 12 points for the physical activity subscale (FABQPA) and 9 points for the work subscale (FABQ-W); however, these were for the Norwegian version. Finally, starting at the second treatment session and at each follow-up period, patients completed the 15-point global rating of change (GROC) scale research report ] FIGURE 2. Supine upper thoracic on midthoracic spine thrust manipulation in cervicothoracic flexion used in this study. The therapist used his manipulative hand to stabilize the inferior vertebra of the motion segment targeted and used his body to push down through the patient’s arms, to perform a high-velocity, low-amplitude thrust. FIGURE 1. Seated thoracic spine distraction thrust manipulation used in this study. The therapist placed his upper chest at the level of the patient’s middle thoracic spine and grasped the patient’s elbows. A high-velocity distraction thrust was performed in an upward direction. described by Jaeschke et al.24 The scale ranges from –7 (“a very great deal worse”) to 0 (“about the same”) to +7 (“a very great deal better”). It has been reported that scores of +4 and +5 are indicative of moderate changes in patient-perceived status and scores of +6 and +7 indicate large changes in patient status.24 As in studies that have developed and attempted to validate the CPR,12,15 patients who rated their perceived recovery on the GROC as “a very great deal better,” “a great deal better,” or “quite a bit better” (a score of +5 or greater) at any followup treatment session were considered to have experienced dramatic improvements. The MCID for the GROC has been reported as a 3-point change from baseline.24 Randomization One of 3 physical therapists recruited patients who met the eligibility criteria and collected all baseline demographics and self-report variables. The 3 physical therapists, who were blinded to group allocation, collected all outcome measures during the trial. Patients were randomly allocated to 1 of the 2 treatment groups by drawing index cards showing the group assignment from sealed, opaque envelopes. A researcher with over 30 years of clinical experience in TJM and blinded to the outcome measures performed all of the treatment interventions. It was not possible to blind the patients and the treating researcher to treatment allocation because of the nature of the interventions. Patients and the treating researcher were instructed not to reveal treatment allocation to the clinicians who were collecting the outcome measures. Treatment Procedures Once all examination procedures were complete, patients were randomly assigned to 1 of 2 groups: (1) patients who received thoracic TJM and an exercise program (thoracic group) or (2) patients who received cervical TJM and an exercise program (cervical group). The exercise program was standardized for both groups and is described in detail in the APPENDIX. Both groups attended physical therapy sessions 3 times during the first week and 2 times during the second week, for a total of 5 sessions over a 2-week period. 210 | april 2011 | volume 41 | number 4 | journal of orthopaedic & sports physical therapy 41-04 Puentedura.indd 210 3/16/2011 12:57:04 PM FIGURE 3. Supine middle to lower thoracic spine thrust manipulation used in this study. The therapist used his manipulative hand to stabilize the inferior vertebra of the motion segment targeted and used his body to push down through the patient’s arms to perform a high-velocity, low-amplitude thrust. Thoracic TJM Group During the first 2 sessions, patients in the thoracic group received thoracic TJM and a cervical ROM exercise. The cervical ROM exercise was the 3-finger exercise for cervical rotation, as originally described by Richard Erhard16 (APPENDIX), which was performed in the clinic as well as at home. All patients in this group received 3 different thoracic spine TJM techniques that were identical to those used in the CPR derivation study.12 A maximum of 2 attempts for each TJM technique was allowed, regardless of having achieved joint cavitation. According to the model for describing thrust manipulations recently proposed by Mintken et al,33 the following techniques were used: 1. A high-velocity, midrange, distraction force to the midthoracic spine on the lower thoracic spine in a sitting position. The therapist placed his upper chest at the level of the patient’s middle thoracic spine and grasped the patient’s elbows. A high-velocity distraction thrust was performed in an upward direction (FIGURE 1 and ONLINE VIDEO). 2. A high-velocity, end range, anteriorposterior force applied through the elbows to the upper thoracic spine on the midthoracic spine in cervicothoracic flexion. This technique was performed with the patient po- FIGURE 4. Cervical spine thrust manipulation used in this study. The therapist used his manipulative hand to localize the motion segment targeted and used both hands to perform a high-velocity, lowamplitude thrust into rotation, which was directed up towards the patient’s contralateral eye. sitioned supine. The therapist used his manipulating hand to stabilize the inferior vertebra of the motion segment targeted and his body to push down through the patient’s arms, to perform a high-velocity, low-amplitude thrust (FIGURE 2 and ONLINE VIDEO). 3. A high-velocity, end range, anteriorposterior force applied through the elbows to the middle thoracic spine on the lower thoracic spine in cervicothoracic flexion. This technique was performed with the patient positioned supine. The therapist used his manipulating hand to stabilize the inferior vertebra of the motion segment targeted and his body to push down through the patient’s arms, to perform a high-velocity, low-amplitude thrust (FIGURE 3 and ONLINE VIDEO). During the last 3 therapy sessions, patients did not receive further TJM and, instead, performed a standardized therapeutic exercise program. Patients continued performing the 3-finger cervical rotation exercise and also commenced a new set of exercises, as described below and illustrated in the APPENDIX. All exercises were performed in a comfortable, seated position, for 3 sets of 10 repetitions each, in the clinic. Patients were instructed to perform these exercises 3 to 4 times per day, within pain tolerance, each day during participation in the study. These exercises were as follows: 1. Three-finger exercise for cervical rotation16 2. Bilateral shoulder shrugs and scapular retractions (against gravity only) 3. Bilateral shoulder horizontal adduction and abduction, with hands clasped behind the head 4. Upper cervical flexion and extension, with hands clasped behind the head and elbows held together (keeping elbows stationary and moving the head into forearms) 5. Lower cervical flexion and extension, with hands clasped behind the head and elbows held together (keeping upper cervical spine stationary and moving elbows up towards ceiling and into lap) 6. Thera-Band rows, with moderateresistance elastic band (green) 7. Lateral pull-downs, with moderateresistance theraband (green) Cervical TJM Group During the first 2 sessions, patients in the cervical group received cervical TJM and performed the same 3-finger cervical ROM exercise as the thoracic group (APPENDIX). All patients in the cervical group received the same cervical spine TJM technique applied to both sides of the neck. The treating therapist, based on pain localization and detection of perceived joint hypomobility, used his clinical discretion to choose the most appropriate or symptomatic cervical motion segments and attempted to localize the TJM to those levels. A maximum of 2 attempts for each side of the cervical spine was allowed, regardless of having achieved joint cavitation. Using the model for describing thrust manipulations recently proposed by Mintken et al33 to, in this example, target the C4-5 level on the left, we used a high-velocity, midrange, right rotational force to the left articular pillar of C4, on the left articular pillar of C5, in supine, with right rotation journal of orthopaedic & sports physical therapy | volume 41 | number 4 | april 2011 | 211 41-04 Puentedura.indd 211 3/16/2011 12:57:06 PM [ TABLE 1 research report Baseline Demographic and Self-Report Variables for All Patients in Both Treatment Groups* Variable Thoracic Group (n = 10) Cervical Group (n = 14) P Value Age (y) 33.1 5.8 34.1 7.0 .723† 6 (60%) 10 (71%) .673‡ 18.8 9.3 11.7 7.0 .044† 5 (50%) 9 (64%) .760§ Cervical extension ROM (°) 21.5 6.4 26.8 7.1 .067† FABQ-PA (0-24) 8.0 4.0 9.7 4.1 .316† FABQ-W (0-42) 3.4 2.6 5.2 2.8 .121† Sex (female) Symptom duration (d) Pain location (unilateral) Abbreviations: FABQ-PA, Fear-Avoidance Beliefs Questionnaire physical activity subscale; FABQ-W, Fear-Avoidance Beliefs Questionnaire work subscale; ROM, range of motion. *Values are mean SD and n (%). † Independent t test. ‡ Fisher exact test. § Pearson chi-square. and left sidebending. This technique was performed with the patient positioned supine. The therapist used his manipulating hand to localize the targeted C4-5 motion segment and both hands to perform a high-velocity, low-amplitude thrust, directed up towards the patient’s contralateral eye (FIGURE 4 and ONLINE VIDEO).19 During the last 3 therapy sessions, patients in the cervical group performed the same standardized therapeutic exercise program as that described previously for the thoracic group. Follow-up All patients completed the GROC and NPRS prior to the start of each subsequent treatment session. Patients were also asked for the presence of any posttreatment side effects (increased neck pain, headache, dizziness, etc) after treatment sessions 1 and 2, which included the TJM interventions. Formal follow-up assessments were performed at 1 week (prior to treatment on the fourth visit), 4 weeks, and 6 months. At each follow-up assessment, patients completed the NDI, NPRS, GROC, and FABQ. Data Analysis Key baseline demographic variables and scores on the self-report measures were compared between groups, using inde- pendent t tests for continuous data and chi-square tests of independence for categorical data (TABLE 1). The primary aim (effects of treatment on disability and pain) was examined with a 2-way repeated-measures analysis of variance (ANOVA), with treatment group (thoracic thrust versus cervical thrust manipulation) as the between-subjects variable and time (baseline and follow-up periods) as the within-subjects variable. Separate ANOVAs were performed with disability (NDI) and pain (NPRS) as the dependent variable. For each ANOVA, the hypothesis of interest was the 2-way (group-by-time) interaction. Interactions were analyzed by using simple main effects for the between-group differences at each measurement point, with a Bonferroni-corrected alpha of .0125 (4 independent-samples t tests). In addition, GROC data for the cervical and thoracic groups were compared using a Wilcoxon rank sum test for each of the following time points: posttreatment 1, 1 week, 4 weeks, and 6 months. Data were analyzed using 2 different approaches. First, an intention-to-treat (ITT) analysis was performed for all patients originally randomized in the trial. Missing data points for dropouts were imputed using the lastobservation-carried-forward method. We also analyzed only the data of those who ] completed the trial, which is referred to as the per-protocol analysis. Data analysis was performed using PASW Statistics 18 (IBM, Somers, NY). To determine absolute risk reduction (ARR) and number needed to treat (NNT), an outcome was deemed an overall success if all of the following occurred: NDI score improvement met or exceeded MDC and MCID (7 scale points out of 50), NPRS score improvement met or exceeded MDC and MCID (2.1 scale points), and GROC score was at least a +5. If a patient did not meet all 3 of the aforementioned criteria, the outcome was deemed unsuccessful. In addition, ARR and NNT were calculated for patients who at the 6-month time point required further treatment and continued medication use for their neck pain following the study intervention. The need for further treatment and/or medication was also defined as an unsuccessful outcome. RESULTS N inety-six consecutive patients with a primary complaint of neck pain were screened for possible eligibility. The reasons for ineligibility can be found in FIGURE 5, the flow diagram of patient recruitment and retention. Of the 96 patients screened, 24 patients (mean SD age, 33.7 6.4 years; range, 26-48 years; 67% female) satisfied the eligibility criteria and agreed to participate in the study. Ten patients were randomly assigned to receive thoracic TJM and exercise, and 14 patients were randomly assigned to receive cervical TJM and exercise. The baseline demographic and self-report variables for both treatment groups are shown in TABLE 1. Four patients in the cervical TJM group did not complete all 5 treatment sessions, citing complete relief (full recovery) of their symptoms. Of these 4 patients, 2 completed the GROC and NPRS at the start of the second session but did not want to continue treatment. The other 2 patients completed the GROC and NPRS at the start of third session but also declined 212 | april 2011 | volume 41 | number 4 | journal of orthopaedic & sports physical therapy 41-04 Puentedura.indd 212 3/16/2011 12:57:07 PM further treatment and follow-up. For all 4 of these patients, we did not obtain NDI or FABQ beyond baseline scores. Patients screened for eligibility (n = 96) Not eligible (n = 72): • Did not meet CPR (n = 56) • Whiplash (n = 8) • Red flags (n = 5) • Prior surgery (n = 2) • Cervical stenosis (n = 1) Neck Disability In the ITT analysis, there was a significant group-by-time interaction on the NDI (F3,66 = 7.241; P = .011; ηp2 = .248; Greenhouse-Geisser correction secondary to a violation of sphericity, P<.001) (FIGURE 6). Using a Bonferroni-corrected alpha (.0125), we found no differences between the cervical and thoracic manipulation groups at baseline (P = .482), 1 week (P = .028), and 4 weeks (P = .021); however, there was a significant difference at 6 months (P = .004) (TABLE 2). In the ITT analysis, 10 out of 14 patients in the cervical group demonstrated improved scores that met or exceeded the MDC and MCID for the NDI from baseline to 4 weeks and from baseline to 6 months; for the thoracic group, 1 patient improved to meet or exceed the MDC and MCID at both time points. In the per-protocol analysis there was also a significant group-by-time interaction on the NDI (F3,54 = 40.260; P<.001; ηp2 = .691; Greenhouse-Geisser correction secondary to a violation of sphericity, P<.001). At baseline, there was no difference between the 2 groups (P = .482). However, at all follow-up points the cervical group had significantly lower NDI scores than the thoracic group (P.001). Neck Pain The ITT analysis showed a significant group-by-time interaction on the NPRS (F3,66 = 15.506; P<.001; ηp2 = .413; Greenhouse-Geisser correction secondary to a violation of sphericity, P<.001). Using a Bonferroni-corrected alpha of .0125, we found no significant differences between the cervical and thoracic manipulation groups at baseline (P = .213); however, we did find significant differences between the 2 groups at 1 week (P = .003), 4 weeks (P<.001), and 6 months (P<.001) (FIGURE 7). The ITT analysis showed that 12 out of 14 patients in the cervical manipulation group had improved scores that Randomized (n = 24) Thoracic spine TJM (n = 10) Cervical spine TJM (n = 14) 1-wk follow-up (n = 10) 1-wk follow-up (n = 10) 4-wk follow-up (n = 10) 4-wk follow-up (n = 10) 6-mo follow-up (n = 10) 6-mo follow-up (n = 10) Did not want to continue, “felt 100%” (n = 4) FIGURE 5. Flow diagram of patient recruitment and retention. Abbreviations: CPR, clinical prediction rule; TJM, thrust joint manipulation. met or exceeded the MDC and MCID for the NPRS at both the 4-week and 6-month points. In the thoracic manipulation group, 4 (at 4 weeks) and 2 (at 6 months) out of 10 patients had improved scores that met or exceeded the MDC and MCID. The results of the per-protocol analysis were identical to those of the ITT analysis. TABLE 2 shows the disability and pain scores for both groups at each follow-up period. Fear-Avoidance Beliefs The ITT analysis also showed a significant group-by-time interaction for the FABQ-PA (F3,66 = 4.271; P = .045; ηp2 = .163; Greenhouse-Geisser correction secondary to a violation of sphericity, P<.001). There were no differences between the cervical and thoracic groups prior to treatment (P = .316). Nor were there differences at the 1-week (P = .082), 4-week (P = .242), and 6-month (P = .037) measurement points (TABLE 2). The per-protocol analysis provided results that were different. A significant groupby-time interaction was observed (F3,54 = 17.503; P<.001; ηp2 = .493; GreenhouseGeisser correction secondary to a violation of sphericity, P<.001). Again, there was no difference between the cervical and thoracic groups prior to treatment (P = .316). There were, however, statistically significant differences at each of the subsequent measurement points, all favoring the cervical group (P.004) (FIGURE 8). Global Rating of Change After 1 treatment, the median (range) GROC for the patients in the cervical manipulation group (+6 [+4 to +7]) was significantly better than that of the tho- journal of orthopaedic & sports physical therapy | volume 41 | number 4 | april 2011 | 213 41-04 Puentedura.indd 213 3/16/2011 12:57:08 PM racic manipulation group (+2 [0 to +4]) (W = 56.00, z = –4.083, P<.001). After 1 week, the median (range) GROC for the patients in the thoracic manipulation group (+4 [+1 to +6]) was higher but still significantly lower than that of the patients in the cervical manipulation group (+7 [+7 to +7]) (W = 55.00, z = –4.595, P<.001). The GROC of the patients in the cervical manipulation group continued to be significantly higher than that of the thoracic manipulation group at both the 4-week (W = 55.00, z = –4.620, P<.001) and 6-month (W = 55.00, z = –4.588, P<.001) measurement points. All patients in the cervical manipulation group reported a GROC of +7 at 4 weeks and 6 months; however, in the thoracic manipulation group the medians (ranges) for the GROC were still lower at 4 weeks (+4 [+1 to +6]) and 6 months (+3 [+1 to +5]). research report ] 16 14 P = .482 P = .028 12 P = .004 P = .021 10 NDI (0-50) [ 8 6 4 2 0 Baseline 1 wk 4 wk Thoracic 6 mo Cervical FIGURE 6. Mean Neck Disability Index (NDI) score, with 95% CI for the intention-to-treat analysis over the course of the trial for the cervical and thoracic manipulation groups. NNT Analysis Treatment Side Effects The ARR ratio for an unsuccessful outcome (those not meeting all 3 of the success criteria at the end of treatment) from baseline to week 1, when taking into account the 4 patients who were lost to follow-up, was 57.1% (95% CI: 29.2%, 85.1%). The associated NNT was found to be 1.8 (95% CI: 1.2, 3.4) in favor of the cervical thrust manipulation group. The ARR ratio for an unsuccessful outcome (those who did not meet all 3 of the success criteria at the end of the trial) at 4 weeks, when taking into account the 4 patients who were lost to follow-up, was 61.4% (95% CI: 31.3%, 91.5%). The associated NNT was 1.6 (95% CI: 1.1, 3.2) in favor of the cervical manipulation group as well. The ARR and NNT for the outcome at 6 months were the same as those at 4 weeks. The ARR ratio for an unsuccessful outcome at 6 months (those needing medication or further treatment after the trial), taking into account the 4 patients lost to follow-up, was 50.0% (95% CI: 15.5%, 84.5%). The NNT to avoid this unsuccessful outcome was 2.0 (95% CI: 1.2, 6.5). See TABLE 3 for overall treatment outcomes for the cervical and thoracic manipulation groups. Patients reported no adverse events during the treatment period, nor were any identified during the 6-month follow-up. We defined an adverse event as sequelae medium- to long-term in duration, with moderate to severe symptoms that were serious, distressing, and unacceptable to the patient and required further treatment.9 Some patients did report minor side effects, which were defined as short term, mild in nature, nonserious, transient, and were reversible consequences of the treatment, such as an increase in neck pain, headache, and fatigue.37 These posttreatment side effects were reported to disappear within 24 to 48 hours. In the per-protocol analysis, which had no data for posttreatment side effects of the 4 patients who dropped out of the study, only 1 patient in the cervical group (7%) reported a minor posttreatment side effect (increased neck pain) after the first treatment, and none reported side effects after the second treatment. Conversely, 8 patients in the thoracic group (80%) reported minor posttreatment side effects after the first treatment, and 7 patients in the thoracic group (70%) reported minor side effects after the second treatment. These minor posttreatment symptoms were reported as increased neck pain, fatigue, headache, or upper back pain that resolved within 24 hours of onset. DISCUSSION T he results of this study show that patients with mechanical neck pain who fit the CPR for thoracic spine thrust manipulation may demonstrate better overall outcomes with TJM directed to the cervical spine as opposed to the thoracic spine. Patients in the cervical group, compared to the thoracic group, showed significantly greater improvements on all of the outcome measures. In addition, patients in the cervical TJM group experienced fewer transient posttreatment side effects. Ten out of 14 patients in the cervical group achieved improvements in the NDI that met or exceeded the MDC and MCID from baseline to 4 weeks and from baseline to 6 months, whereas only 1 patient in the thoracic group met or exceeded the MDC and MCID at these follow-up points. The cervical group also experienced more rapid and greater pain relief than the thoracic group. Twelve of the 14 214 | april 2011 | volume 41 | number 4 | journal of orthopaedic & sports physical therapy 41-04 Puentedura.indd 214 3/16/2011 12:57:10 PM 6 P = .213 5 NPRS (0-10) 4 3 P = .003 P<.001 P<.001 2 1 0 –1 Baseline 1 wk 4 wk Thoracic 6 mo Cervical FIGURE 7. Mean numeric pain rating scale (NPRS) score, with 95% CI for the intention-to-treat analysis over the course of the trial for the cervical and thoracic manipulation groups. 12 P = .316 10 P<.004 FABQ-PA (0-24) 8 P<.004 6 P<.004 4 2 0 Baseline 1 wk 4 wk Thoracic 6 mo Cervical FIGURE 8. Mean Fear-Avoidance Beliefs Questionnaire physical activity subscale (FABQ-PA) score with 95% CI for the per-protocol analysis over the course of the trial for the cervical and thoracic manipulation groups. patients in the cervical group achieved improvements in the NPRS that met or exceeded the MDC and MCID, and all the patients in the cervical group achieved GROC equal to or greater than +5 within 1 week. In contrast, only 3 of the 10 patients in the thoracic group achieved improvement in the NPRS that met or exceeded the MDC and MCID, and only 2 out of 10 reported a GROC score equal to or greater than +5 within 1 week. The majority of patients in the cervical group, compared to only 1 thoracic patient in the thoracic group, met the criteria for overall success at both the 4-week and 6-month follow-ups. The NNT of 1.8 in favor of the cervical group over the thoracic group suggests that only 2 patients with neck pain would need to be treated with cervical TJM to prevent an unsuccessful outcome at 1 week. Similarly, an NNT of 1.6 in favor of the cervical group at 4 weeks and 6 months suggests that only 2 patients with neck pain would need to be treated with cervical TJM to prevent an unsuccessful outcome at those time points. Only 1 patient in the cervical group reported a need for further treatment and medication at the 6-month followup, whereas, in the thoracic group, 8 patients required further treatment and 7 required continued medications. The NNT to avoid the need for further treatment and medication was 2.0 in favor of cervical manipulation, so that only 2 patients with neck pain would need to be treated with cervical TJM to prevent the need for further treatment and medication for 1 patient at 6 months. While the sample size in our study was small, we feel that it was sufficient to produce meaningful statistics. Furthermore, the 4 patients lost during the study were actually those demonstrating the best and most immediate response. Thus, our results might have underestimated the true differences. Thoracic spine manipulation has been shown to be advantageous for patients with neck pain,13 and a CPR had been derived12 to identify those patients who would most likely benefit from such treatment. This CPR was recently examined for validity in a randomized clinical trial,15 the results of which did not support the CPR’s validity. However, the authors did demonstrate that patients journal of orthopaedic & sports physical therapy | volume 41 | number 4 | april 2011 | 215 41-04 Puentedura.indd 215 3/16/2011 12:57:11 PM [ ] research report Outcomes From the Intention-to-Treat Analysis for Both Groups at Each Follow-up Period* TABLE 2 Outcome/Group Baseline 1 wk 4 wk 6 mo NDI (0-50) Thoracic 12.6 1.9 (10.9, 14.3) 10.9 2.0 (9.0, 12.8) 9.1 3.7 (6.0, 12.2) 9.9 3.9 (6.6, 13.2) Cervical 13.4 2.9 (11.9, 14.8) 8.3 3.4 (6.7, 9.9) 4.2 5.4 (1.6, 6.8) 3.7 5.7 (0.9, 6.5) NPRS (0-10) Thoracic 3.6 1.4 (2.4, 4.9) 2.1 1.6 (1.5, 2.8) 1.9 1.0 (1.5, 2.3) 2.3 1.1 (1.9, 2.8) Cervical 4.6 2.2 (3.6, 5.7) 0.1 0.2 (–0.5, 0.7) 0.1 0.1 (–0.3, 0.4) 0.1 0.1 (–0.3, 0.4) FABQ-PA (0-24) Thoracic 8.0 4.0 (5.4, 10.6) 5.5 3.6 (3.3, 7.7) 4.0 2.7 (1.9, 6.1) 5.2 3.0 (3.0, 7.4) Cervical 9.7 4.1 (7.5, 12.0) 2.9 3.3 (1.0, 4.8) 2.4 3.4 (0.7, 4.2) 2.1 3.5 (0.3, 4.0) Abbreviations: FABQ-PA, Fear-Avoidance Beliefs Questionnaire physical activity subscale; NDI, Neck Disability Index; NPRS, numeric pain rating scale. *Values are mean SD (95% CI). TABLE 3 Overall Treatment Outcomes From the Intention-to-Treat Analyses for the Cervical and Thoracic Manipulation Groups Outcome Baseline to 1 wk Baseline to 4 wk Baseline to 6 mo Cervical TJM NDI, met or exceeded MDC and MCID 8/14 10/14 10/14 NPRS, met or exceeded MDC and MCID 12/14 12/14 12/14 GROC, at least +5 14/14 14/14 14/14 Overall success (met all 3 above criteria) 8/14 10/14 10/14 ... ... Treatment, 1/10*; medication, 1/10* Unsuccessful outcome, need for further treatment or medication Thoracic TJM NDI, met or exceeded MDC and MCID 0/10 1/10 1/10 NPRS, met or exceeded MDC and MCID 3/10 4/10 2/10 GROC, at least +5 2/10 2/10 2/10 Overall success (met all 3 above criteria) 0/10 1/10 1/10 ... ... Treatment, 8/10; medication, 7/10 Unsuccessful outcome (need for further treatment or medication) Abbreviations: GROC, global rating of change scale; MCID, minimal clinically important difference; MDC, minimal detectable change; NDI, Neck Disability Index; NPRS, numeric pain rating scale; TJM, thrust joint manipulation. *No data about need for further treatment or medication were available for the 4 patients who dropped from the study. with mechanical neck pain who received thoracic spine TJM and exercise, compared to patients who received exercise only, exhibited significantly greater improvements in pain and disability. These results suggest that the CPR did not help to identify patients with mechanical neck pain who would demonstrate greater improvements when provided with thoracic spine TJM in addition to exercise. They did, however, show that patients with mechanical neck pain (and no contraindications for TJM), who were given a combination of thoracic spine TJM and exercise, had statistically and clinically significant greater improvements in pain and disability compared to those who received exercise alone. One limitation suggested by the authors of this study was that different exercise approaches might have resulted in different outcomes. In the recent CPR validation study,15 patients who were positive on the CPR and received thoracic manipulation had a baseline mean NDI of 14.0/50, which improved to 6.3/50 at 1 week, 4.1/50 at 4 weeks, and 3.2/50 at 6 months. Patients in the thoracic group of our study had a comparable mean NDI score at baseline (12.6/50) but did not show as much improvement over time (10.9/50 at 1 week, 9.1/50 at 4 weeks, and 9.9/50 at 6 months). A comparison of changes in NPRS measures between the thoracic manipulation groups in the 2 studies revealed a similar trend: patients in the CPR validation study15 had a NPRS score of 4.3 at baseline, 1.9 at 1 week, 1.6 at 4 weeks, and 1.5 at 6 months; patients in the current study started with a lower mean NPRS score at baseline (3.6) and did not appear to improve as much over time, with mean scores of 2.1 at 1 week, 1.9 at 4 weeks, and 2.3 at 6 months. The inconsistencies in outcomes between 216 | april 2011 | volume 41 | number 4 | journal of orthopaedic & sports physical therapy 41-04 Puentedura.indd 216 3/16/2011 12:57:12 PM these studies might be explained by their different exercise programs. Patients in the validation study15 participated in a more extensive program, which included manual stretching by the physical therapist, whereas the current study limited its exercise program to those exercises described in the APPENDIX. It is also important to note that the patients in the current study presented with acute neck pain. Mean duration of symptoms for all patients was 14.7 days, and the duration of symptoms for those in the cervical group (11.7 days) was shorter (P = .044) than that of the thoracic group (18.8 days). This is a limitation associated with the randomization in the study and may account for some of the differences observed in outcomes between groups. The shorter the duration of the patients’ symptoms in this study contrasts with that of the patients in the CPR derivation and validation studies.12,15 In the CPR derivation study,12 mean duration of symptoms was 80 days for all patients, 54.6 days for those who experienced a successful outcome, and 109.6 days for the nonsuccessful outcome group. In the CPR validation study,15 the mean duration of symptoms was 63.5 days for all patients, regardless of their status on the CPR, 53.0 days for those patients who were classified as positive on the CPR (the manipulation group), and 47.6 days for the exercise-only group. It is possible that a shorter duration of symptoms may be associated with better outcomes of manual therapy to the cervical spine. In a recent study, Leaver et al30 compared cervical spine TJM with nonthrust mobilization techniques in patients with recent-onset neck pain. The authors tracked days to recovery from neck pain, defined as the first of 7 consecutive days on which the patient reported less than 1 on a 0-to-10 NPRS. While they found no difference in recovery rates, less than 60% of patients in both the manipulation and mobilization groups actually achieved recovery.30 They also found no better outcomes between the groups in terms of pain, disability, function, global perceived effect, or health-related quality of life.30 The mean SD duration of symptoms for all patients in that study was 19.4 20.0 days,30 indicating that not all patients had a symptom duration of less than 30 days. Also, the baseline characteristics of these patients showed that 63.2% reported a previous episode of neck pain and a majority had concomitant symptoms such as upper limb pain (79.1%), headache (64.3%), and upper back pain (63.2%).30 These findings suggest that very few of the patients in that study would have met the inclusion criteria for our current study and, furthermore, 30.8% reported dizziness/ vertigo and 22.5% reported nausea, which would have excluded them from our study. Despite the absence of adverse events related to the cervical manipulation treatment and an equal prevalence of minor side effects such as additional neck pain and headache for both the manipulation and mobilization groups, the authors suggested that practitioners and their patients reevaluate the use of manipulation for recent-onset neck pain. 30 The short duration of symptoms in our study sample might have been due to our choosing a cutoff point of 4 out of 6 predictor variables for a positive status on the thoracic TJM CPR. The CPR validation study15 used 3 out of 6 predictors to determine status on the rule, based on the derivation study’s12 finding of a wide CI for the positive likelihood ratio (LR) associated with positive findings on 4 out of 6 tests (95% CI: 2.28, 70.8). By choosing the more stringent cutoff, our study sample was limited to patients with a symptom duration of less than 30 days, as prospective patients who did not meet this particular criterion invariably had difficulty meeting at least 3 out of the remaining 5 predictor variables. All patients in our study had a symptom duration of equal to or less than 30 days and had no symptoms distal to the shoulder. Study Limitations Several important limitations of this study should be noted, the first of which is its small sample size. Despite screening close to 100 potential patients, we were only able to recruit about 25% into the study because of the stringent inclusion and exclusion criteria used in the CPR derivation study. Considering the study’s small sample size, we chose to be conservative with our statistical analyses and used a Bonferroni correction. Despite this approach, our results demonstrated significant differences between groups on all outcome measures at most of the follow-up points, with the exception of the NDI changes at the 1-week (P = .028) and 4-week (P = .021) follow-ups. Had we not used the Bonferroni correction, these NDI changes would have been significant (P<.05). Unfortunately, we did not examine the outcomes in patients who had neck pain regardless of their status on the rule, which could be an area for future research. Patients in the cervical group had significantly shorter duration of symptoms compared to those in the thoracic group. This occurred despite adequate randomization and may well have been due to our relatively small sample size. Another limitation is that all patients were recruited from 1 of 2 clinics in a city (Las Vegas) within the Western United States, and all interventions were provided by 1 practitioner. Future studies should recruit a larger sample size from more diverse locations and involve a greater number of practitioners to better generalize the results. Also, as with other trials involving manual therapy interventions, it was not possible to blind the practitioner or patients to treatment allocation, as in some placebo-controlled trials. CONCLUSION T his study tested 2 different forms of TJM in a select group of patients with mechanical neck pain who met a previously derived12 and recently questioned CPR.15 We found that patients who were treated with a combination of cervical spine TJM and exercises showed significantly greater journal of orthopaedic & sports physical therapy | volume 41 | number 4 | april 2011 | 217 41-04 Puentedura.indd 217 3/16/2011 12:57:13 PM [ improvement in pain and disability compared to those treated with thoracic spine TJM and exercises. Our results suggest that patients with neck pain of less than 30 days in duration, who meet 4 out of the 6 CPR criteria for thoracic spine TJM, may benefit more from cervical than thoracic spine TJM. t KEY POINTS FINDINGS: Patients who were treated with a combination of cervical spine TJM and exercises showed significantly greater improvement in pain and disability compared to those treated with thoracic spine TJM and exercises. They also experienced fewer transient posttreatment side effects than patients who had thoracic spine manipulation and exercise. IMPLICATION: The CPR for thoracic spine manipulation and exercise in patients with neck pain may actually be helpful in identifying patients who are more likely to benefit from cervical spine manipulation, but this needs to be formally tested. CAUTION: Several factors limiting the generalizability of this study include a small sample size, that all patients had acute neck pain (neck pain for less than 30 days), and that all interventions were provided by 1 physical therapist. ACKNOWLEDGEMENTS: It is with great sadness that we say good-bye to our close friend and colleague Peter Huijbregts, who tragically passed away on November 6, 2010. Peter made many terrific contributions to the profession of physical therapy and has been instrumental in the battle to maintain manipulation within the scope of our practice. Peter had a terrific passion for life and was truly an inspiring individual who will be greatly missed by us and the profession. REFERENCES 1. Adams G, Sim J. A survey of UK manual therapists’ practice of and attitudes towards manipulation and its complications. Physiother Res Int. research report ] 1998;3:206-227. 2. B ialosky JE, Bishop MD, George SZ. Regional interdependence: a musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2008;38:159-160; author reply 160. http://dx.doi.org/10.2519/jospt.2008.0201 3. Borghouts J, Janssen H, Koes B, Muris J, Metsemakers J, Bouter L. The management of chronic neck pain in general practice. A retrospective study. Scand J Prim Health Care. 1999;17:215-220. 4. Borghouts JA, Koes BW, Bouter LM. The clinical course and prognostic factors of nonspecific neck pain: a systematic review. Pain. 1998;77:1-13. 5. Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized clinical trial of exercise and spinal manipulation for patients with chronic neck pain. Spine (Phila Pa 1976). 2001;26:788-797; discussion 798-789. 6. Bronfort G, Haas M, Evans RL, Bouter LM. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. Spine J. 2004;4:335-356. http://dx.doi.org/10.1016/j. spinee.2003.06.002 7. Bronfort G, Nilsson N, Haas M, et al. Noninvasive physical treatments for chronic/ recurrent headache. Cochrane Database Syst Rev. 2004;CD001878. http://dx.doi. org/10.1002/14651858.CD001878.pub2 8. Carlesso LC, Macdermid JC, Santaguida LP. Standardization of adverse event terminology and reporting in orthopaedic physical therapy: application to the cervical spine. J Orthop Sports Phys Ther. 2010;40:455-463. http:// dx.doi.org/10.2519/jospt.2010.3229 9. Carnes D, Mullinger B, Underwood M. Defining adverse events in manual therapies: a modified Delphi consensus study. Man Ther. 15:2-6. http://dx.doi.org/10.1016/j.math.2009.02.003 10. Childs JD, Cleland JA, Elliott JM, et al. Neck pain: Clinical practice guidelines linked to the International Classification of Functioning, Disability, and Health from the Orthopedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38:A1-A34. http://dx.doi.org/10.2519/jospt.2008.0303 11. Childs JD, Flynn TW, Fritz JM, et al. Screening for vertebrobasilar insufficiency in patients with neck pain: manual therapy decision-making in the presence of uncertainty. J Orthop Sports Phys Ther. 2005;35:300-306. http://dx.doi. org/10.2519/jospt.2005.1312 12. Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87:9-23. http://dx.doi.org/10.2522/ ptj.20060155 13. Cleland JA, Childs JD, McRae M, Palmer JA, Stowell T. Immediate effects of thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther. 2005;10:127-135. http:// dx.doi.org/10.1016/j.math.2004.08.005 14. C leland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69-74. http://dx.doi.org/10.1016/j. apmr.2007.08.126 15. Cleland JA, Mintken PE, Carpenter K, et al. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multicenter randomized clinical trial. Phys Ther. 2010;90:1239-1250. http://dx.doi.org/10.2522/ ptj.20100123 16. Erhard R. The Spinal Exercise Handbook: A Home Exercise Manual for a Managed Care Environment. Pittsburgh, PA: Laurel Concepts; 1998. 17. Ernst E. Vascular accidents after neck manipulation: cause or coincidence? Int J Clin Pract. 2010;64:673-677. http://dx.doi. org/10.1111/j.1742-1241.2009.02237.x 18. Flynn TW, Whitman J, Magel J. Orthopaedic Manual Physical Therapy Management of the Cervico-Thoracic Spine and Ribcage. San Antonio, TX: Manipulations, Inc; 2000. 19. Gibbons P, Tehan P. Manipulation of the Spine, Thorax and Pelvis: An Osteopathic Perspective. 3rd ed. Edinburgh, UK: Churchill-Livingstone; 2010. 20. Grotle M, Brox JI, Vollestad NK. Reliability, validity and responsiveness of the fear-avoidance beliefs questionnaire: methodological aspects of the Norwegian version. J Rehabil Med. 2006;38:346-353. http://dx.doi. org/10.1080/16501970600722403 21. Hains F, Waalen J, Mior S. Psychometric properties of the neck disability index. J Manipulative Physiol Ther. 1998;21:75-80. 22. Hogg-Johnson S, van der Velde G, Carroll LJ, et al. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976). 2008;33:S39-51. http://dx.doi. org/10.1097/BRS.0b013e31816454c8 23. Hurwitz EL, Carragee EJ, van der Velde G, et al. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976). 2008;33:S123-152. http://dx.doi.org/10.1097/ BRS.0b013e3181644b1d 24. Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10:407-415. 25. Jensen MP, Miller L, Fisher LD. Assessment of pain during medical procedures: a comparison of three scales. Clin J Pain. 1998;14:343-349. 26. Jensen MP, Turner JA, Romano JM. What is the maximum number of levels needed in pain intensity measurement? Pain. 1994;58:387-392. 27. Jette AM, Delitto A. Physical therapy treatment choices for musculoskeletal impairments. Phys 218 | april 2011 | volume 41 | number 4 | journal of orthopaedic & sports physical therapy 41-04 Puentedura.indd 218 3/16/2011 12:57:14 PM Ther. 1997;77:145-154. 28. J ull G. Use of high and low velocity cervical manipulative therapy procedures by Australian manipulative physiotherapists. Aust J Physiother. 2002;48:189-193. 29. Kendall FP. Muscles: Testing and Function. 4th ed. Baltimore, MD: Lippincott, Williams & Wilkins; 1993. 30. Leaver AM, Maher CG, Herbert RD, et al. A randomized controlled trial comparing manipulation with mobilization for recent onset neck pain. Arch Phys Med Rehabil. 2010;91:1313-1318. http://dx.doi.org/10.1016/j.apmr.2010.06.006 31. MacDermid JC, Walton DM, Avery S, et al. Measurement properties of the neck disability index: a systematic review. J Orthop Sports Phys Ther. 2009;39:400-417. http://dx.doi.org/10.2519/ jospt.2009.2930 32. Maitland G, Hengeveld E, Banks K, English K. Maitland’s Vertebral Manipulation. Oxford, UK: Butterworth-Heinemann; 2000. 33. Mintken PE, DeRosa C, Little T, Smith B. AAOMPT clinical guidelines: a model for standardizing manipulation terminology in physical therapy practice. J Orthop Sports Phys Ther. 2008;38:A1-A6. http://dx.doi.org/10.2519/ jospt.2008.0301 34. Price DD, Bush FM, Long S, Harkins SW. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain. 1994;56:217-226. 35. Puentedura E, Louw A, Mintken PE. Neuro- 36. 37. 38. 39. 40. 41. 42. dynamic interventions for the management of patients with headache. In: Fernandez-delas-Penas C, Arend-Nielsen L, Gerwin R, eds. Tension-Type and Cervicogenic Headache: Pathophysiology, Diagnosis, and Management. Sudbury, MA: Jones and Bartlett; 2010:393-420. Riddle DL, Stratford PW. Use of generic versus region-specific functional status measures on patients with cervical spine disorders. Phys Ther. 1998;78:951-963. Senstad O, Leboeuf-Yde C, Borchgrevink C. Frequency and characteristics of side effects of spinal manipulative therapy. Spine (Phila Pa 1976). 1997;22:435-440; discussion 440-431. Spurling RG, Segerberg LH. Lateral intervertebral disk lesions in the lower cervical region. J Am Med Assoc. 1953;151:354-359. Strunce JB, Walker MJ, Boyles RE, Young BA. The immediate effects of thoracic spine and rib manipulation on subjects with primary complaints of shoulder pain. J Man Manip Ther. 2009;17:230-236. Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409-415. Vicenzino B, Collins D, Benson H, Wright A. An investigation of the interrelationship between manipulative therapy-induced hypoalgesia and sympathoexcitation. J Manipulative Physiol Ther. 1998;21:448-453. Vicenzino B, Collins D, Wright A. The initial effects of a cervical spine manipulative physio- 43. 44. 45. 46. 47. therapy treatment on the pain and dysfunction of lateral epicondylalgia. Pain. 1996;68:69-74. Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157-168. Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine (Phila Pa 1976). 2003;28:52-62. http://dx.doi.org/10.1097/01. BRS.0000038873.01855.50 Wainner RS, Whitman JM, Cleland JA, Flynn TW. Regional interdependence: a musculoskeletal examination model whose time has come. J Orthop Sports Phys Ther. 2007;37:658-660. http:// dx.doi.org/10.2519/jospt.2007.0110 Wheeler AH, Goolkasian P, Baird AC, Darden BV, 2nd. Development of the Neck Pain and Disability Scale. Item analysis, face, and criterion-related validity. Spine (Phila Pa 1976). 1999;24:1290-1294. Williamson E. Fear Avoidance Beliefs Questionnaire (FABQ). Aust J Physiother. 2006;52:149. @ MORE INFORMATION WWW.JOSPT.ORG APPENDIX THE EXERCISE PROGRAM PERFORMED BY BOTH TREATMENT GROUPS DURING THE TRIAL* Following the thrust joint manipulation at each of the first 2 treatment sessions, both groups performed the 3-finger exercise for cervical rotation, as originally described by Richard Erhard.16 For the third through to fifth treatment sessions, both groups performed the therapeutic exercises, as shown below. 1. B ilateral shoulder shrugs and scapular retractions (against gravity only) journal of orthopaedic & sports physical therapy | volume 41 | number 4 | april 2011 | 219 41-04 Puentedura.indd 219 3/16/2011 12:57:15 PM [ research report ] APPENDIX 2. B ilateral shoulder horizontal adduction and abduction with hands clasped behind the head 3. U pper cervical flexion and extension with hands clasped behind the head and elbows held together (keeping elbows stationary and moving the head into forearms) 4. L ower cervical flexion/extension, with hands clasped behind the head and elbows held together (keeping upper cervical spine stationary and moving elbows up towards ceiling and into lap) 5. Thera-Band rows with moderate-resistance elastic band (green) 6. Lateral pull-downs with moderate-resistance elastic band (green) *Images used with permission from International Spine & Pain Institute. 220 | april 2011 | volume 41 | number 4 | journal of orthopaedic & sports physical therapy 41-04 Puentedura.indd 220 3/16/2011 12:57:18 PM