Research Report
advertisement

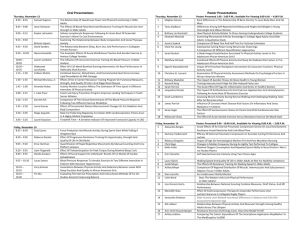
Research Report Effect of Aerobic Training on Walking Capacity and Maximal Exercise Tolerance in Patients With Multiple Sclerosis: A Randomized Crossover Controlled Study Anais Rampello, Marco Franceschini, Massimo Piepoli, Roberto Antenucci, Gabriella Lenti, Dario Olivieri, Alfredo Chetta Background and Purpose Physical deconditioning is involved in the impaired exercise tolerance of patients with multiple sclerosis (MS), but data on the effects of aerobic training (AT) in this population are scanty. The purpose of this study was to compare the effects of an 8-week AT program on exercise capacity—in terms of walking capacity and maximum exercise tolerance, as well as its effects on fatigue and health-related quality of life—as compared with neurological rehabilitation (NR) in subjects with MS. Subjects and Methods Nineteen subjects (14 female, 5 male; mean age [X⫾SD]⫽41⫾8 years) with mild to moderate disability secondary to MS participated in a randomized crossover controlled study. Eleven subjects (8 female, 3 male; mean age [X⫾SD]⫽44⫾6 years) completed the study. Results After AT, but not NR, the subjects’ walking distances and speeds during a self-paced walk were significantly improved, as were their maximum work rate, peak oxygen uptake, and oxygen pulse during cardiopulmonary exercise tests. The increases in peak oxygen uptake and maximum work rate, but not in walking capacity, were significantly higher after AT, as compared with after NR. Additionally, the subjects who were most disabled tended to benefit more from AT. There were no differences between AT and NR in effects on fatigue, and the results showed that AT may have partially affected health-related quality of life. Discussion and Conclusion The results suggest that AT is more effective than NR in improving maximum exercise tolerance and walking capacity in people with mild to moderate disability secondary to MS. A Rampello, MD, is Registrar, Department of Geriatrics and Rehabilitation, Unit of Rehabilitation, University Hospital of Parma, Parma, Italy. M Franceschini, MD, is Consultant, Department of Geriatrics and Rehabilitation, Unit of Rehabilitation, University Hospital of Parma. M Piepoli, MD, is Consultant, Heart Failure Unit, Department of Cardiology, G da Saliceto Hospital, Piacenza, Italy. R Antenucci, MD, is Registrar, Unit of Rehabilitation, G da Saliceto Hospital. G Lenti, MD, is Consultant, Unit of Rehabilitation, G da Saliceto Hospital. D Olivieri, MD, is Full Professor, Department of Clinical Sciences, Section of Respiratory Diseases, University of Parma, Parma, Italy. A Chetta, MD, is Associate Professor, Department of Clinical Sciences, Section of Respiratory Diseases, University of Parma, Viale G Rasori, 10 – 43100, Parma, Italy. Address all correspondence to Dr Chetta at: chetta@unipr.it. [Rampello A, Franceschini M, Piepoli M, et al. Effect of aerobic training on walking capacity and maximal exercise tolerance in patients with multiple sclerosis: a randomized crossover controlled study. Phys Ther. 2007;87:545– 555.] © 2007 American Physical Therapy Association Post a Rapid Response or find The Bottom Line: www.ptjournal.org May 2007 Volume 87 Number 5 Physical Therapy f 545 Aerobic Training in Patients With Multiple Sclerosis M ultiple sclerosis (MS) is a chronic demyelinating disease of the central nervous system characterized by disturbances in nerve conduction and manifested by various clinical features. People with MS often complain of poor exercise tolerance and exertion fatigue that limit their daily living activities.1,2 Peripheral factors3–5 as well as central factors2,6 – 8 may be involved in the pathogenesis of the reduced exercise tolerance and fatigue in people with MS. An abnormally high energy cost of walking has been suggested as an important contributing factor in leg fatigue during treadmill exercise.3 Respiratory muscle dysfunction also has been related to the reduction in exercise tolerance in people with MS.4 A recent study by Chetta et al5 showed that subjects with MS who were mildly disabled had reduced limb endurance and an impaired cardiorespiratory response to self-paced walking that might have been related to deconditioning, cardiovascular autonomic dysfunction, and altered breathing control. Deconditioning may play a key role in the impaired exercise tolerance of people with MS. In order to minimize fatigue, people with MS limit their physical activity.1,2 This limited physical activity, in turn, can lead to deconditioning and disuse that further worsens limb weakness and fatigue.9 Furthermore, fatigue and limitation of physical activity may reduce the ability to participate in daily social and family activities.9 positively affect both maximum exercise capacity12 and daily physical activities.13 In both the study by Petajan et al12 and the study by Romberg et al,13 however, the effect of aerobic exercise was compared with that of no treatment. In addition, in the study by Romberg et al,13 aerobic exercise consisted of aquatic training, which was not tailored to meet the specific exercise capabilities of the subjects. Only one study14 previously examined the effects of aerobic training (AT) on maximum exercise capacity, as compared with a physical therapy program. The analysis was restricted to within-group comparisons, and the results showed a significant increase in the anaerobic threshold but no changes in maximum aerobic capacity. Therefore, the purpose of this randomized crossover controlled study was to assess the effects of an 8-week AT program on exercise capacity— in terms of walking capacity and maximum exercise tolerance, as well as its effects on fatigue and healthrelated quality of life—as compared with a neurological rehabilitation (NR) protocol in subjects with mild to moderate disability secondary to MS. We considered both the AT program and the NR protocol as 2 effective rehabilitative interventions for people with MS. Accordingly, we hypothesized that the 2 rehabilitation protocols could have similar effects on the functional status of subjects with MS. Method One of the primary aims of rehabilitation in people with MS is to maintain and improve functional independence. Review studies10,11 suggest that exercise therapy may be beneficial for patients with MS in terms of physical fitness, activities of daily living, and outcomes related to mood. In particular, aerobic exercise seems to be a promising rehabilitative tool for patients with MS because it could 546 f Physical Therapy Volume 87 Subjects and Design The subjects were screened from a waiting list for a rehabilitation program in the MS outpatient clinics at Parma University Hospital and Piacenza Hospital between January and May 2005. The inclusion criteria were: a diagnosis of MS according to the criteria of Poser et al,15 a score of 6 or less on the Expanded Disability Status Scale (EDSS)16 because indi- Number 5 viduals with an EDSS score greater than 6 need constant use of a bilateral aid while walking, and age between 20 and 55 years. Subjects were excluded if they had a relapse 4 weeks before the study; had a history of cardiac, pulmonary, orthopedic, metabolic, or other medical conditions precluding participation; were currently receiving steroid therapy or had been treated with steroids within 2 months prior to the study; or had engaged in a regular exercise program within 2 months before the study. After screening, the subjects were randomly assigned, according to a computer-generated randomization list, and stratified by sex, age, and EDSS score to receive either an AT or NR 8-week parallel crossover intervention. To avoid any interference between the 2 interventions, all subjects waited 8 weeks before initiating the second intervention. During the 8-week washout period, the subjects were instructed to stop exercising. Clinical assessments, lung function and respiratory muscle strength (force-generating capacity) testing, 6-minute walk tests (6MWTs), and cardiopulmonary exercise tests (CPETs) were administered by the same examiner both prior to and after each 8-week treatment without knowledge of the subject’s group assignment. Out of 40 eligible subjects, 21 subjects were excluded because they did not meet the inclusion criteria or they declined to be enrolled (Fig. 1). Accordingly, we studied 19 subjects with MS (14 female, 5 male). The subjects’ ages ranged from 22 to 51 years, and their disease duration ranged from 1 to 15 years. None of the subjects reported any history of cardiac or pulmonary disease, and all subjects had normal physical examinations of the chest, chest radiographs, and resting electrocardiograms. At the time of the study, 10 subjects were being treated with inMay 2007 Aerobic Training in Patients With Multiple Sclerosis Eligible subjects (n=40) Excluded (n=21) Not meeting inclusion criteria (n=17) Refused to participate (n=4) Enrollment Randomization Allocated to aerobic training group (n=8) Received allocated intervention (n=8) Allocation Allocated to neurological rehabilitation group (n=11) Received allocated intervention (n=11) Follow-up Completed aerobic training (n=8) Completed neurological rehabilitation (n=11) Dropouts (n=2) MS relapses (n=1) Did not adhere to protocol (n=1) Allocated to aerobic training group (n=9) Received allocated intervention (n=9) Dropouts (n=2) MS relapses (n=1) Did not adhere to protocol (n=1) Allocated to neurological rehabilitation group (n=6) Allocation Received allocated intervention (n=6) Dropouts (n=3) MS relapses (n=1) Did not adhere to protocol (n=2) Completed aerobic training (n=6) Analyzed (n=6) Dropouts (n=1) MS relapses (n=1) Completed neurological rehabilitation (n=5) Follow-up Analysis Analyzed (n=5) Figure 1. Flow chart of the randomized crossover controlled study. MS⫽multiple sclerosis. terferon beta, 4 with mitoxantrone, and 1 with glatiramer acetate. All subjects gave informed consent to participate in the study. Clinical Assessment The subjects’ neurological impairment and degree of disability were assessed with the EDSS, which provides a score ranging from 0, indicating normal neurological findings, to 10, indicating death from MS. This scale is a reliable and valid measure of impairment and disability in people with MS.17 The EDSS score was assigned without knowledge of the May 2007 subjects’ pulmonary function and exercise capacity test results. The subjects’ perceived effect of fatigue was assessed with the Modified Fatigue Impact Scale (MFIS),18 which has been validated in people with MS.19,20 The MFIS is a structured, self-report, 21-item questionnaire that provides an assessment of the effects of fatigue in terms of physical, cognitive, and psychosocial functions. Scores on the MFIS range from 0 to 84, and all items are scaled so that higher scores indicate a greater effect of fatigue on a person’s activities. Fatigue is defined as a selfreported lack of physical or mental energy that is perceived by the individual to interfere with usual and desired activities.19 The disease-specific Multiple Sclerosis Quality of Life–54 questionnaire (MSQOL-54) was used to assess health-related quality of life.21,22 The 54 items are divided into 12 multipleitem scales and 2 single-item scales. The MSQOL-54 item results are transformed linearly to scores of 0 to 100, and final scale scores are created by averaging the scores of items within Volume 87 Number 5 Physical Therapy f 547 Aerobic Training in Patients With Multiple Sclerosis the scales. A higher score in each scale indicates a better health-related quality of life. Physical health composite (PHC) and mental health composite (MHC) scores were calculated as a weighted sum of selected scale scores. The reliability and validity of the MSQOL-54 scores have been confirmed in subjects with MS.23 Lung Function, Respiratory Muscle Strength, and Exercise Capacity Assessment Pulmonary function was measured with a flow-sensing spirometer (Vmax 22)* and a body plethysmograph (Vmax 6200)* connected to a computer for data analysis. Baseline total lung capacity (TLC), forced expiratory volume in 1 second (FEV1), vital capacity (VC), and FEV1/VC ratio were recorded. All of these variables are expressed as a percentage of the predicted value.24 The best out of 3 results was used in subsequent calculations. Maximum inspiratory pressure and maximum expiratory pressure were performed against a valve, which could be closed by turning a tap.25 Maximum inspiratory pressure and maximum expiratory pressure were measured (in centimeters of water) from TLC and residual volume (RV), respectively. The highest out of 5 recorded pressures maintained for 1 second were used for analysis. Walking capacity was assessed with the 6MWT, according to a standard protocol.26 The 6MWT is a symptomlimited exercise test, so subjects were allowed to stop if necessary, although they were instructed to resume walking as soon as possible. All subjects performed two 6MWTs, the second test performed the same as the first test, following a rest of at least 60 minutes. The walking distance was recorded in meters and * SensorMedics Corp, 22705 Savi Ranch Pwy, Yorba Linda, CA 92667-4609. 548 f Physical Therapy Volume 87 expressed as a percentage of the predicted value, which accounted for age, sex, and height.27 Additionally, the walking speed (in meters per minute) was calculated. Oxygen uptake (V̇O2, in milliliters per kilogram per minute) was continuously monitored with a portable lightweight system (VmaxST)* from 5 minutes before the walk until test completion, as well as 5 minutes after completion or until the return to the baseline level. The V̇O2 and the cost of walking during the walk (expressed as mL O2䡠kg⫺1䡠m⫺1)3 were considered for analysis. Results from only the second walk were used for analysis to allow for any learning effect.26,28 Each subject performed a physiciansupervised, standard, progressively increasing work rate CPET to maximum tolerance on an electromagnetically braked cycle ergometer. Gas exchange measurements (Vmax 229)* were taken for 3 minutes at rest, for 3 minutes of unloaded cycling at 60 rpm followed by a progressively increasing work rate exercise of 5 to 20 W䡠min⫺1 to maximum tolerance, and for 2 minutes of recovery. Pulse oximetry, heart rate (HR), 12-lead electrocardiogram, and cuff blood pressure were monitored and recorded. Minute ventilation, V̇O2, and carbon dioxide production (V̇CO2) were computer-calculated breath by breath, interpolated second by second, and averaged over 10-second intervals. The maximum work rate (in watts), the V̇O2 at the peak of the exercise (in milliliters per minute and as a percentage of the predicted value),29 and the V̇O2/HR at the peak of the exercise (in milliliters divided by beats per minute and as a percentage of the predicted value)29 were considered for analysis. Rehabilitation Program The AT program partially followed the protocol proposed by Petajan Number 5 et al.12 Briefly, the subjects participated in 3 training sessions per week on a leg cycle ergometer for 8 weeks. Each training session consisted of a 5-minute warm-up at 30% of maximum work rate, then 30 minutes at 60% of maximum work rate, which was followed by a 5-minute cool-down. Subjects then performed stretching exercises of their lower limbs and trunk muscles for 15 minutes. Workloads were calculated from the work rate obtained during the CPET and were progressively increased every week up to 80% of maximum work rate. Heart rate, blood pressure, pulse oximetry, and the subjects’ perceived exertion, as assessed with a visual analog scale, were monitored during exercise. During the NR program, subjects underwent 3 sessions per week for 8 weeks. Each session lasted 60 minutes and consisted of exercises aimed at improving respiratorypostural and respiratory-motor synergies and of stretching exercises. These exercises consisted of active movements of the trunk and upper limbs in a standing, sitting, or kneeling position, such as flexion and rotation movements of the trunk; gait exercises, including tandem gait or ambulation exercises combining advancement of one lower limb with raising of the opposite upper limb; and exercises for stretching the lower limbs and trunk muscles. During each exercise, much emphasis was placed on breathing, as the subjects were asked to inspire during active movements and to expire during relaxation. The exercises were grouped in 4 parts, separated by 3-minute pauses, and were all proposed with the same temporal sequence. Trained physical therapists instructed the subjects individually on both AT and NR programs and supervised each exercise program session. Before and immediately after each May 2007 Aerobic Training in Patients With Multiple Sclerosis Table 1. Characteristics of the 19 Subjects With Multiple Sclerosis Enrolled in the Study, of the 11 Subjects Who Completed the Study, and of the 8 Subjects Who Withdrew From the Studya Variable All Subjects (nⴝ19) Subjects Who Completed Study (nⴝ11) Subjects Who Withdrew From Study (nⴝ8) Pb Age (y) 41⫾8 44⫾6 37⫾10 .21 Sex (female/male) 14/5 8/3 6/2 .99 BMI (kg/m2) 22⫾3 23⫾3 21⫾3 .54 8⫾5 6⫾4 10⫾6 .34 8/3 7/1 .74 3.5 (1–4) 3.25 (1.5–6) .96 Disease duration (y) Using disease-modifying drugs (yes/no) EDSS score (0–10) FEV1/VC (% of predicted value) 15/4 3.5 (1–6) 82⫾8 82⫾8 83⫾8 .99 FEV1 (% of predicted value) 103⫾13 105⫾13 100⫾13 .69 TLC (% of predicted value) 111⫾8 112⫾11 112⫾14 PImax (cm H2O) 83⫾35 75⫾42 95⫾16 .46 .94 PEmax (cm H2O) 93⫾36 91⫾37 96⫾36 .94 a Values expressed as mean⫾SD, except for Expanded Disability Status Scale (EDSS) scores, which are expressed as median (range). BMI⫽body mass index, FEV1⫽forced expiratory volume in 1 second, VC⫽vital capacity, TLC⫽total lung capacity, PImax⫽maximum inspiratory pressure, PEmax⫽maximum expiratory pressure. b P values assessed by chi-square test (sex, using disease-modifying drugs), analysis of variance (age, BMI, disease duration, FEV1/VC, FEV1, TLC, PImax, PEmax), and Kruskal-Wallis test (EDSS score). exercise program session, subjects rated the magnitude of their perceived breathlessness and fatigue on a visual analog scale. Data Analysis We considered 2 outcome measures. The primary outcome measure was the effect of the rehabilitation programs on exercise capacity. The secondary outcome measure was the effect of the rehabilitation programs on fatigue and health-related quality of life. Values are presented as mean⫾ standard deviation, unless otherwise specified. Between-group differences for all enrolled subjects, the subjects who completed the study, and the subjects who did not complete the study were examined using the chisquare test, the analysis of variance, and the Kruskal-Wallis test, when appropriate. In order to analyze the between-group and within-group inMay 2007 terventions, the analysis of variance for repeated measures and the Newman-Keuls multiple comparison test were used for analysis of variables with Gaussian distribution, and the Friedman test was used for analysis of nonparametric variables. A P value ⱕ.05 was taken as significant. The clinical effect of the interventions on the primary outcomes was assessed by the effect size statistic, calculated as the mean change found in a variable divided by the standard deviation of that variable.30 We used the criteria of Cohen31 to interpret the effect size, where a value of 0.2 is considered a small effect, a value of 0.5 is considered a moderate effect, and a value of 0.8 is considered a large effect. Results Fourteen of the 19 subjects recruited for the investigation completed the AT program, and 16 subjects com- pleted the NR program. Only 11 subjects, however, were able to complete the overall crossover controlled parallel study and were considered for analysis. Four subjects did not adhere to the study protocol and dropped out of the trial. In 2 of those subjects, the exercise program sessions induced a perception of breathlessness and fatigue, which persisted up to the beginning of the following session, thereby precluding the continuation of the rehabilitation program. The other 2 subjects withdrew from the rehabilitation program because they felt it was too stressful. Four subjects had a relapse of MS (2 subjects during the AT program and 2 subjects during the NR program) and were unable to complete the study (Fig. 1). Personal details and pulmonary function test results of the 19 subjects enrolled in the study, of the 11 subjects who completed the study, and of the 8 subjects who did not complete the study are reported in Table 1. No between-group differ- Volume 87 Number 5 Physical Therapy f 549 Aerobic Training in Patients With Multiple Sclerosis Table 2. Preintervention and Postintervention Values for Lung Function, Respiratory Muscle Strength, 6-Minute Walk Tests, and Cardiopulmonary Exercise Tests in Subjects With Multiple Sclerosisa Variable Aerobic Training Group Preintervention FEV1/VC (% of predicted value) Postintervention Neurological Rehabilitation Group b P Preintervention Postintervention Pb Pc Pd 84⫾6 83⫾8 .74 82⫾8 84⫾7 .54 .51 .75 FEV1 (% of predicted value) 110⫾11 108⫾10 .66 105⫾13 109⫾11 .44 .34 .82 TLC (% of predicted value) 117⫾14 116⫾13 .86 113⫾14 115⫾14 .74 .51 .86 PImax (cm H2O) 78⫾45 80⫾42 .91 75⫾42 77⫾41 .91 .87 .86 PEmax (cm H2O) 88⫾38 90⫾35 .89 91⫾37 92⫾38 .95 .85 .89 308⫾98 332⫾108 .02 298⫾114 308⫾110 .17 .59 .18 Walking distance (% of predicted value) 55⫾17 59⫾19 .02 53⫾20 55⫾20 .22 .67 .25 Walking speed (m/min) 51⫾16 55⫾18 .02 50⫾19 51⫾18 .14 .60 .23 Cost of walking (mL O2䡠kg⫺1䡠m⫺1) 0.20⫾0.07 0.20⫾0.07 .13 0.23⫾0.1 0.22⫾0.09 .41 .42 .13 Peak V̇O2 (mL/min/kg) 17.1⫾7.0 20.0⫾6.6 .01 16.8⫾6.5 16.9⫾6.1 .88 .66 .02 Peak V̇O2 (% of predicted value) 58⫾18 68⫾18 .01 57⫾17 57⫾18 .88 .89 .02 Maximum work rate (W) 82⫾43 103⫾48 .01 79⫾45 82⫾42 .47 .53 .02 Peak V̇O2/HR (mL/bpm) 7.8⫾3.0 8.7⫾3.2 .04 7.8⫾2.9 8.1⫾3.5 .57 .96 .40 Peak V̇O2/HR (% of predicted value) 75⫾19 84⫾17 .04 76⫾21 78⫾25 .67 .87 .49 Walking distance (m) a Values expressed as mean⫾SD. FEV1⫽forced expiratory volume in 1 second, VC⫽vital capacity, TLC⫽total lung capacity, PImax⫽maximum inspiratory pressure, PEmax⫽maximum expiratory pressure, V̇O2⫽oxygen uptake, HR⫽heart rate. P values assessed by means of analysis of variance for repeated measures and Newman-Keuls multiple comparison test. b Preintervention vs postintervention. c Preintervention vs preintervention. d Postintervention vs postintervention. ences were found. In addition, when baseline condition measurements of the 2 interventions were considered, no difference was found (Tabs. 2, 3, and 4). Disease Progression and Exercise Adherence No change over time was found in neurological status, as measured with the EDSS (P⫽1.0). All subjects who completed the study adhered very well to both the AT program and the NR program. Of 264 exercise sessions 550 f Physical Therapy Volume 87 prescribed for either the AT program or the NR program, 230 and 238 exercise sessions, respectively, were completed, with an average adherence rate of 87%⫾8% and of 90%⫾6%, respectively. No exercise-related injuries were reported. Primary and Secondary Outcomes Lung function and respiratory muscle strength were not changed by participation in the AT program or the NR program (Tab. 2). All subjects Number 5 were able to complete a 6MWT without stopping. Due to technical problems, we recorded only preintervention and postintervention values for the 6MWT in 8 out of 11 subjects. Within-group analysis showed that subjects had significant improvements in walking distance (P⫽.02) and walking speed (P⫽.02) after the AT program, but not after the NR program. Cost of walking also did not change after completion of the AT program or the NR program (Tab. 2). When interventions were May 2007 Aerobic Training in Patients With Multiple Sclerosis Table 3. Preintervention and Postintervention Modified Fatigue Impact Scale (MFIS) Scores in Subjects With Muliple Sclerosisa Variable Aerobic Training Group Neurological Rehabilitation Group Preintervention Postintervention P Preintervention Postintervention Pb Pc Pd Total MFIS score 36 (3–57) 29 (4–56) .66 30 (6–52) 26 (3–67) .64 .94 .86 Physical subscale 17 (3–27) 14 (4–23) .39 19 (6–33) 13 (3–26) .55 .79 .89 Cognitive subscale 11 (0–34) 8 (0–36) .84 11 (0–31) 10 (0–40) .97 .00 .71 3 (0–6) 3 (0–7) .89 4 (0–6) 2 (0–6) .57 .69 .92 Psychosocial subscale b a Values are expressed as median (range). P values assessed by means of Friedman test. Preintervention vs postintervention. Preintervention vs preintervention. d Postintervention vs postintervention. b c analyzed between groups, no difference was found. The effect size for walking distance and maximum work rate was small (0.2) in the AT program and negligible (0.09) in the NR program. After the AT program, subjects showed a significant increase in peak V̇O2 (P⫽.01), maximum work rate (P⫽.01), and peak V̇O2/HR at CPET (P⫽.04) when preintervention and postintervention values were compared. Moreover, after the AT program, 82% of the subjects had a percent increase in change of maximum work rate greater than 10% of the baseline value. After the NR program, subjects showed no significant increase in any CPET values (Tab. 2, Fig. 2). When interventions were analyzed between groups, peak V̇O2 and maximum work rate after the AT program were significantly increased compared with the corresponding values after the NR program (P⫽.025 and P⫽.02). The effect size for peak V̇O2 and maximum work rate was moderate in the AT program (0.6 and 0.5, respectively) and negligible in the NR program (0.02 and 0.07, respectively). The MFIS and MSQOL-54 scores before and after AT and NR intervenMay 2007 tions are shown in Tables 3 and 4. After the AT program, the subjects showed a significant increase in 3 MSQOL-54 scale scores (emotional well-being, energy, and health distress). After the NR program, the subjects had significant improvements in health distress and mental health composite scores and a significant reduction in emotional wellbeing scores. Discussion Our study showed that, in subjects with mild to moderate disability secondary to MS, maximum exercise tolerance improved after completion of the 8-week AT and NT programs, as compared with baseline conditions. The change in walking capacity was significant after the AT program when compared with baseline conditions, but not after the NR program. Despite the effect of the AT program on physical performance, this rehabilitative approach did not differ from the NR intervention in terms of the perceived effect of fatigue and only partially affected the subjects’ health-related quality of life. Walking capacity can be assessed simply and reliably with the selfpaced 6MWT, which can be consid- ered to be a measure of limb endurance and reflects the submaximal functional exercise level of daily physical activities.26 Restricted walking prevents people with MS from participating in family and social activities and is a major determinant of overall impairment in people with MS who are ambulatory.32 Moreover, the walking distance covered during the 6MWT was found to be inversely related to the EDSS scores.5 In the present study, we found that the walking capacity of patients with MS who were mildly to moderately disabled was substantially reduced, as expressed as a percentage of the predicted value, and was significantly increased after the AT program but not after the NR program. Furthermore, the change in walking capacity induced by AT did not significantly differ from the change induced by NR. Previous studies, different in length and kind of exercise and in outcomes, showed discordant results of the effects of AT on walking capacity in subjects with MS. Rodgers et al,33 in an uncontrolled study, found minimal effects on gait abnormalities (ie, decreased walking speed and cadence) after 6 months of AT. In contrast, Romberg et al13 showed that a Volume 87 Number 5 Physical Therapy f 551 Aerobic Training in Patients With Multiple Sclerosis Table 4. Preintervention and Postintervention Multiple Sclerosis Quality of Life–54 Questionnaire (MSQOL-54) Scores in Subjects With Multiple Sclerosisa Variable Aerobic Training Group Preintervention Postintervention Neurological Rehabilitation Group b P Preintervention Postintervention Pb Pc Pd Physical function 68 (35–95) 60 (25–95) .59 70 (25–95) 55 (20–95) .92 .72 .84 Role limitations– physical 25 (0–100) 75 (0–100) .69 50 (0–100) 75 (0–100) .71 .72 .97 Role limitations– emotional 100 (0–100) 100 (0–100) .66 100 (0–100) 100 (0–100) .87 1.00 .76 Pain 63 (23–100) 63 (32–100) .59 68 (30–100) 77 (38–100) .79 .77 .41 Emotional wellbeing 52 (4–84) 56 (28–84) .02 56 (4–76) 52 (28–76) .04 .59 .62 Energy 36 (8–64) 44 (32–64) .04 44 (24–56) 40 (20–72) .86 .67 .14 Health perception 40 (10–70) 35 (10–75) .84 45 (5–70) 35 (15–65) .76 .92 .92 Social function 67 (33–100) 75 (50–100) .45 75 (8–92) 83 (38–100) .81 .74 .49 Cognitive function 70 (0–100) 75 (10–100) .69 70 (5–100) 80 (25–100) .77 1.00 1.00 Health distress 60 (40–95) 75 (60–95) .03 65 (15–90) 75 (55–100) .03 .83 .74 Sexual function 100 (42–100) 100 (33–100) 1.00 100 (50–100) 100 (33–100) .61 .84 .76 Sexual satisfaction 75 (50–75) 75 (50–75) .66 75 (75–100) 75 (0–100) .87 .97 .92 Change in health 50 (25–75) 50 (25–50) .96 50 (25–75) 75 (50–75) .66 .97 .68 Overall quality of life 36 (5–77) 28 (10–82) 1.00 28 (20–73) 36 (20–82) .36 .59 .19 Physical health composite 50 (39–82) 59 (44–81) .65 53 (43–81) 57 (41–81) .33 .55 1.00 Mental health composite 60 (10–86) 66 (24–90) .41 63 (18–85) 66 (32–87) .03 .51 .89 a Values are expressed as median (range). P values assessed by means of Friedman test. Preintervention vs postintervention. c Preintervention vs preintervention. d Postintervention vs postintervention. b 6-month AT program, including aquatic exercises, induced an increase in walking speed compared with no therapy. Recently, in an uncontrolled study, Kileff and Ashburn34 found that 24 biweekly sessions of 30 minutes of cycling on a stationary bicycle improved walking distance. In that study, the mean improvement in 6MWT walking distance was 32 m. In the present study, we found that the AT program induced a significant change in maximum aerobic capacity and work rate both over the study 552 f Physical Therapy Volume 87 time and as compared with the NR program. Moreover, if we consider that a 10% increase in work rate on the cycle ergometer is indicative of an improvement in fitness, as suggested by Schapiro and colleagues,35 we found that this outcome was achieved by most subjects undergoing AT. Our findings are consistent with those of Petajan et al,12 who found a significant change in maximum aerobic capacity and work load in subjects who undertook AT compared with no therapy. Interestingly, we found a 20% increase in aerobic capacity, which is comparable to Number 5 that found by Petajan et al,12 despite a different duration of training (8 versus 15 weeks) and mode of aerobic exercise (leg cycle ergometer versus combined arm and leg cycle ergometer). By contrast, Mostert and Kesselring14 did not find any change in maximum aerobic capacity in subjects with MS after a 4-week period of AT, despite findings of significant increases in V̇O2, anaerobic threshold, and maximum work rate. The shortness of the training period and the different degree of disability may explain the discrepancy between May 2007 Aerobic Training in Patients With Multiple Sclerosis showed that the peak oxygen pulse increased after the AT program, but not after the NR program. To our knowledge, no data concerning the effect of rehabilitation programs on oxygen pulse have been available until now, except for the study by Mostert and Kesselring,14 which demonstrated significant change in oxygen pulse measured at anaerobic threshold in subjects with MS who participated in an AT program. Figure 2. Mean and standard deviation of peak oxygen uptake (V̇O2) as percentage of predicted value (upper panel), of maximum work rate in watts (middle panel), and of walking distance as percentage of predicted value (lower panel) in 11 subjects with multiple sclerosis before and after aerobic training (AT) or neurological rehabilitation (NR). P values assessed by means of analysis of variance for repeated measures and Newman-Keuls multiple comparison test. *P⬍.05 vs all measurements; § P⬍.05 vs baseline measurement. these results and those of Petajan et al12 and our study. In people with MS, the peak oxygen pulse during maximal incremental exercise on a cycle ergometer may be reduced when compared with subjects who are healthy.36 This finding suggests that people with MS may have reduced cardiovascular fitness, which, in turn, may be related to deconditioning. In this study, we May 2007 Our results showed that both AT and NR intervention led to no significant change in the subjects’ MFIS scores. The poor influence of physical exercise on perception of fatigue may be related to the multidimensional origin of fatigue, because central factors,2,6 – 8 in addition to peripheral mechanisms,3–5 are known to play a key role in the pathogenesis of this symptom. Furthermore, the MFIS may not be sensitive enough to detect changes in fatigue over time, and the duration of the rehabilitative program was too short to determine significant changes. Previous studies have shown discordant results on the effect of AT on fatigue. Some studies failed to demonstrate a significant effect of AT on fatigue, when comparing exercise training versus no exercise therapy12 or “conventional” physical therapy.14 In contrast, Surakka et al37 found that 6 months of aerobic and strength exercises reduced motor fatigue in women, but not in men. In this study, we showed that AT only partly affected the health perception of the subjects, particularly by significantly inducing increases in emotional well-being, energy, and health distress scores. In contrast, the NR program had a contradictory effect because it improved health distress and mental health composite scores while reducing emotional well-being. The mechanism of action of these changes is not completely clear and may not relate directly to the AT program or the NR program. Both intervention programs facilitate the patient’s socialization, which, in itself, may have contributed to some of the beneficial effects. Moreover, it has been demonstrated that exercise may enhance psychological wellbeing via a strong placebo effect.38 We found a high rate of participant loss in this study. Among our subjects, a 26% dropout rate was observed, which was higher than dropout rates reported in previous studies.13,14 Variations in the type and duration of the programs can explain the different adherence rates of the subjects with MS. Our rehabilitative protocol was an outpatient program that lasted 6 months, the study by Mostert and Kesselring14 used a 4-week inpatient program, and the study by Romberg et al13 used a combined 3-week inpatient program and a 23-week home-based rehabilitation program. However, our findings, together with previous findings, could imply that people with MS may have limited tolerance for traditional exercise training, and other rehabilitative strategies, such as pacing and energy conservation techniques, should be considered to improve their functional status. We are aware of the numerous limitations of our study. First, a large number of subjects did not complete the study, and we are aware that a type II error may have occurred in our analysis of results. Moreover, the participant loss prevented a full intention-to-treat analysis being carried out. However, as far as we know, our study is the first randomized controlled study comparing 2 different rehabilitation interventions in patients with MS, which was conducted in a crossover way. In addition, we did not find any betweengroup (all subjects versus subjects who completed the study versus subjects who withdrew from the study) difference in baseline conditions. Volume 87 Number 5 Physical Therapy f 553 Aerobic Training in Patients With Multiple Sclerosis This finding could likely minimize the bias due to the effect of attrition on the study sample.39 Second, it is well known that there is a learning effect when maximal or submaximal exercise testing, such as the 6MWT and the CPET, are performed. Thus, we cannot exclude the possibility that the positive results of our study might have been due, in part, to the expected variability in these measures. However, our subjects performed the 6MWT twice on the study day to minimize the learning effect of this exercise test because performance usually reaches a plateau after 2 tests are done within a week.26 Moreover, in the assessment of maximum exercise capacity, we followed the same method as that applied in previous clinical trials in which subjects performed the CPET only once.12-14 Third, we arbitrarily choose an 8-week washout period between the 2 interventions. However, previous studies of subjects with MS showed beneficial effects on disability and health-related quality of life after rehabilitation, which lasted for 6 weeks40 to 9 weeks.41 Moreover, in our study, we can exclude a carryover effect between interventions because no significant difference was found in baseline measurements of the 2 interventions. Lastly, we are aware that we compared the AT program with the NR program by using specific outcomes for the AT program. We, therefore, cannot exclude the possibility that the NR program could be superior to the AT program with regard to nonaerobic outcomes (eg, flexibility, balance) that were not measured in this study. Conclusions The findings demonstrated that 8 weeks of AT may be more effective than NR in improving maximum ex554 f Physical Therapy Volume 87 ercise tolerance and walking capacity in patients with MS and mild to moderate disability, leading to some positive effects on health-related quality of life. Our study supports the view that AT may be beneficial for patients with MS who are not experiencing an exacerbation of symptoms. However, the high rate of participant loss that occurred in our study also indicates that exercise programs may harm patients with MS. Further studies are needed to determine whether a more graded AT program can improve the adherence of patients with MS. Dr Rampello, Dr Franceschini, and Dr Chetta provided concept/idea/research design. Dr Rampello and Dr Chetta provided writing and data analysis. Dr Rampello and Dr Piepoli provided data collection. Dr Franceschini, Dr Olivieri, and Dr Chetta provided project management. Dr Franceschini and Dr Olivieri provided fund procurement. Dr Rampello, Dr Antenucci, and Dr Lenti provided subjects. Dr Piepoli, Dr Olivieri, and Dr Chetta provided consultation (including review of manuscript before submission). The study protocol was approved by the ethics committees of University Hospital of Parma and of G da Saliceto Hospital. This article was received March 15, 2006, and was accepted January 9, 2007. DOI: 10.2522/ptj.20060085 References 1 Freal JF, Kraft GH, Coryell JK. Symptomatic fatigue in MS. Arch Phys Med Rehabil. 1984;65:135–138. 2 Comi G, Leocani L, Rossi P, Colombo B. Physiopathology and treatment of fatigue in multiple sclerosis. J Neurol. 2001;248: 174 –179. 3 Olgiati R, Jacquet J, Di Prampero PE. Energy cost of walking and exertional dyspnea in multiple sclerosis. Am Rev Respir Dis. 1986;134:1005–1010. 4 Foglio K, Clini E, Facchetti D, et al. Respiratory muscle function and exercise capacity in multiple sclerosis. Eur Respir J. 1994;7:23–28. 5 Chetta A, Rampello A, Marangio E, et al. Cardiorespiratory response to walk in multiple sclerosis patients. Respir Med. 2004; 98:522–529. 6 Sandroni P, Walzer C, Starr A. Fatigue in patients with multiple sclerosis: motor pathway conduction and event-related potentials. Arch Neurol. 1992;49:517–524. Number 5 7 Roelcke U, Kappos L, Lechner-Scott J, et al. Reduced glucose metabolism in the frontal cortex and basal ganglion of multiple sclerosis patients with fatigue. Neurology. 1997;48:1566 –1571. 8 Schubert M, Wohlfarth K, Rollnik JD, Dengler R. Walking and fatigue in multiple sclerosis: the role of the corticospinal system. Muscle Nerve. 1998;21:1068 –1070. 9 MacAllister WS, Krupp LB. Multiple sclerosis-related fatigue. Phys Med Rehabil Clin North Am. 2005;16:483–502. 10 White LJ, Dressendorfer RH. Exercise and multiple sclerosis. Sports Med. 2004;34: 1077–1100. 11 Rietberg MB, Brooks D, Uitdehaag BMJ, Kwakkel G. Exercise therapy for multiple sclerosis. Cochrane Database Syst Rev. 2005;(1):CD003980. 12 Petajan JH, Gappmaier E, White AT, et al. Impact of aerobic training on fitness and quality of life in multiple sclerosis. Ann Neurol. 1996;39:432– 441. 13 Romberg A, Virtanen A, Ruutiainen J, et al. Effects of a 6-month exercise program on patients with multiple sclerosis: a randomized study. Neurology. 2004; 63:2034 –2038. 14 Mostert S, Kesselring J. Effects of a shortterm exercise training program on aerobic fitness, fatigue, health perception and activity level of subjects with multiple sclerosis. Mult Scler. 2002;8:161–168. 15 Poser GM, Paty DW, Scheinberg L, et al. New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol. 1983;13:227–231. 16 Kurtzke JF. Rating neurological impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology. 1983;33:1444 –1452. 17 Sharrack B, Hughes RA, Soudain S, Dunn G. The psychometric properties of clinical rating scales used in multiple sclerosis. Brain. 1999;122:141–159. 18 Fisk JD, Pontefract A, Ritvo PG, et al. The impact of fatigue on patients with multiple sclerosis. Can J Neurol Sci. 1994;21:9 –14. 19 Fisk JD, Ritvo PG, Ross L, et al. Measuring the functional impact of fatigue: initial validation of the Fatigue Impact Scale. Clin Infect Dis. 1994;18(suppl 1):S79 –S83. 20 Kos D, Kerckhofs E, Carrea I, et al. Evaluation of the Modified Fatigue Impact Scale in four different European countries. Mult Scler. 2005;11:76 – 80. 21 Vickrey BG, Hays RD, Harooni R, et al. A health-related quality of life measure for multiple sclerosis. Qual Life Res. 1995; 4:187–206. 22 Solari A, Filippini G, Mendozzi L, et al. Validation of Italian multiple sclerosis quality of life 54 questionnaire. J Neurol Neurosurg Psychiatry. 1999;67:158 –162. 23 Miller A, Dishon S. Health-related quality of life in multiple sclerosis: psychometric analysis of inventories. Mult Scler. 2005;11:450 – 458. 24 Quanjer PH, Tammeling GJ, Cotes JE, et al. Lung volumes and forced ventilatory flows. Eur Respir J Suppl. 1993;16:5– 40. May 2007 Aerobic Training in Patients With Multiple Sclerosis 25 Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationships to age and sex. Am Rev Respir Dis. 1969;99:696 –702. 26 American Thoracic Society Statement: guidelines for the Six-Minute Walk Test. Am J Respir Crit Care Med. 2002; 166:111–117. 27 Chetta A, Zanini A, Pisi G, et al. Reference values for 6-minute walk test in healthy subjects 20 –50 years old. Respir Med. 2006;100:1573–1578. 28 Knox AJ, Morrison JFJ, Muers MF. Reproducibility of walking test results in chronic obstructive airways disease. Thorax. 1988;43:388 –392. 29 Wasserman K, Hansen JE, Sue DY, et al. Principles of Exercise Testing and Interpretation. 3rd ed. Baltimore, Md: Lippincott Williams & Wilkins; 1999:143–164. 30 Kazis LE, Anderson JJ, Meenan RF. Effect sizes for interpreting changes in health status. Med Care. 1989;27(3 suppl):S178 – S189. Invited Commentary The authors should be congratulated for proposing this study to investigate the relationship between an aerobic cycling program and a functional activity outcome such as the cost of walking. As they point out, it is possible that the physical impairments that occur with the disease also may lead to a more sedentary lifestyle and deconditioning, resulting in further limitations in functional ability. For many years, limited knowledge of the pathophysiology of multiple sclerosis restricted our efforts to select the appropriate intensity of intervention and the prevention of accumulation of functional disability. Studies such as this help us to formulate better hypotheses for future interventions. In summary, the authors found that an 8-week program of cycling on a lower-extremity ergometer with progressive resistance resulted in an increase in walking distance and speed for individuals with mild to moderate impairment related to multiple sclerosis. Improvements also were seen in measures of aerobic capacity. SimMay 2007 31 Cohen J. Statistical Power Analysis for the Behavioral Sciences. London, United Kingdom: Academic Press Ltd; 1977:1–20. 32 Schwid SR, Goodman AD, Mattson DH, et al. The measurement of ambulatory impairment in multiple sclerosis. Neurology. 1997;49:1419 –1424. 33 Rodgers MM, Mulcare JA, King DL, et al. Gait characteristics of individuals with multiple sclerosis before and after a 6-month aerobic training program. J Rehabil Res Dev. 1999;36:183–188. 34 Kileff J, Ashburn A. A pilot study of the effect of aerobic exercise on people with moderate disability multiple sclerosis. Clin Rehabil. 2005;19:165–169. 35 Schapiro RT, Petajan JH, Kosich D, et al. Role of cardiovascular fitness in multiple sclerosis: a pilot study. J Neurol Rehabil. 1988;2:43– 49. 36 Tantucci C, Massucci M, Piperno R, et al. Energy cost of exercise in multiple sclerosis patients with low degree of disability. Mult Scler. 1996;2:161–167. 37 Surakka J, Romberg A, Ruutiainen J, et al. Effects of aerobic and strength exercise on motor fatigue in men and women with multiple sclerosis: a randomized controlled trial. Clin Rehabil. 2004;18: 737–746. 38 Desharnais R, Jobin J, Cote C, et al. Aerobic exercise and the placebo effect: a controlled study. Psychosom Med. 1993; 55:149 –154. 39 Dumville JC, Torgerson DJ, Hewitt CE. Reporting attrition in randomised controlled trials. BMJ. 2006;332:969 –971. 40 Patti F, Ciancio MR, Cacopardo M, et al. Effects of a short outpatient rehabilitation treatment on disability of multiple sclerosis patients: a randomised controlled trial. J Neurol. 2003;250:861– 866. 41 Solari A, Filippini G, Gasco P, et al. Physical rehabilitation has a positive effect on disability in multiple sclerosis patients. Neurology. 1999;52:57– 62. Carol Leiper ilar changes did not occur when the subjects performed a “neurological rehabilitation” exercise program described as emphasizing active movements and gait exercises. I would like to address 2 very different topics related to the study: (1) whether reported improvements represent real change and (2) the importance of continued physical activity for people with physical disability. Measurement of Change The measure of walking distance during the 6-minute walk tests will be used as the example to discuss the first question. The authors report a statistically significant improvement in walking distance of approximately 24 m following the aerobic training but not after the neurological training. However, the comparison between the 2 groups did not indicate the superiority of the aerobic training. How do we explain this discrepancy? One solution is to look at the size of the standard deviations of the measurements. The larger the standard deviation, the less likely the results will be significant unless the mean values are greatly different. The authors have used these variables to calculate the effect size and show us that for these 2 measures it is indeed small. Another way to translate the results into meaningful values for the clinician would be to ask the question, “What is the minimal detectable change (MDC) of the measurements that would indicate a real change, indicating either improvement related to the intervention or, perhaps in a chronic disease, deterioration over time?” Because all measurements have some error associated with them, we would like to know that a reported change exceeded the likelihood of that due to errors of measurement. The MDC is frequently reported as the value of the standard error of measurement (SEM) multiplied by ⫾1.96 (⫾2 standard deviations) and therefore should be outside the range of measurement error. For example, Kennedy and colleagues1 deter- Volume 87 Number 5 Physical Therapy f 555