Gait & Posture 29 (2009) 123–128
Contents lists available at ScienceDirect
Gait & Posture
journal homepage: www.elsevier.com/locate/gaitpost
Recording scapular motion using an acromion marker cluster
Carolien van Andel a,b,*, Kim van Hutten b, Marielle Eversdijk b, DirkJan Veeger b,c, Jaap Harlaar a,b
a
Department of Rehabilitation Medicine, Research Institute MOVE, VU University Medical Center, Amsterdam, The Netherlands
Research Institute MOVE, Faculty of Human Movement Sciences, Vrije Universiteit, Amsterdam, The Netherlands
c
Man Machine Systems, Delft University of Technology, The Netherlands
b
A R T I C L E I N F O
A B S T R A C T
Article history:
Received 9 July 2007
Received in revised form 3 July 2008
Accepted 23 July 2008
Disorders of the shoulder complex can be accompanied by changes in the movement pattern of the
scapula. However, scapular motion is difficult to measure. A possible non-invasive method for dynamic
three-dimensional kinematic measurement of the human scapula is the use of a marker cluster placed on
the flat part of the acromion. A small light-weight acromion marker cluster (AMC) is presented in this
study. In order to assess validity, kinematics obtained with the AMC were compared to simultaneous
scapula locator (SL) recordings in a series of postures. The test/retest variability of replacement of the
AMC, was also assessed. Measurement errors appeared to be sensitive for the plane of movement, the
degree of humerus elevation, and replacement of the AMC. The AMC generally under-estimated scapula
motion, compared to the SL. Some significant differences were found between the two methods, although
the absolute differences were small (maximum mean difference 8.48 in extreme position). In humerus
forward flexion and abduction the maximum mean differences were 68 or lower. In conclusion, the AMC
is a valid method of measuring scapular movement during arm elevation that could be used in shoulder
pathologies. Placement and planes of movement should be carefully considered and elevation of the
humerus should not exceed 1008.
ß 2008 Elsevier B.V. All rights reserved.
Keywords:
3D kinematics
Scapula
Acromion
Dynamic
Validation
1. Introduction
Scapular movement is an essential component in arm elevation.
The position of the scapula serves as an adaptive base of support for
the humerus. Abnormal scapular kinematics are believed to
contribute to shoulder pain and pathology, i.e. frozen shoulder
[1], impingement [2], glenohumeral instability [3] and in joint
replacement results [4]. Knowledge of the contribution of scapula
motion to the humero-thoracic motion may benefit certain aspects
of current clinical practice, such as physical examination,
reconstructive surgery and rehabilitation programs. A recent
study demonstrated the importance of recognizing the presence
of scapular hypoplasia, elevation and rotation deformity before
deciding on a treatment plan for persistent internal rotation due to
internal rotation contracture in patients with obstetric brachial
plexus injury [5].
When using motion capture technology, it is difficult to track
the movement of the scapula during dynamic shoulder function,
* Corresponding author at: VU University Medical Center, Department of
Rehabilitation Medicine, P.O. Box 7057, 1007 MB Amsterdam, The Netherlands.
Tel.: +31 20 4440756; fax: +31 20 4440787.
E-mail address: cj.vanandel@vumc.nl (C. van Andel).
0966-6362/$ – see front matter ß 2008 Elsevier B.V. All rights reserved.
doi:10.1016/j.gaitpost.2008.07.012
because of its broad, flat shape, substantial soft-tissue covering,
and significant skin motion over it. Several methods have been
developed for accurate registration of scapular movement. The
insertion of bone pins into the scapula of living subjects, combined
with a motion capture system, such as an electromagnetic one is
obviously the most accurate [6,7]. Despite its high accuracy, such
an invasive method is not feasible in clinical practice unless very
important decisions depend on it. For diagnostic or evaluation
research a number of non-invasive possibilities, based on
electromagnetic or optical tracking devices, have been developed
to measure scapular movements. These possibilities are detailed in
Table 1.
From all the available options to track scapular motion, the
acromial method enables dynamic 3D measurement of scapula
kinematics. A clinically feasible method requires unconstrained
measurement to minimize load and pain for the patient and to
allow for natural (including compensatory) movements, especially
for (young) children. This method can be included in motion
capture protocols, e.g. to evaluate the pre-operative and postoperative status of patients with upper extremity pathologies,
especially when dynamic functional movements need to be
studied. When upper extremity kinematic data are collected with
an optoelectronic system by camera detection of active LED
markers, no standard marker cluster is available. A special
C. van Andel et al. / Gait & Posture 29 (2009) 123–128
124
Table 1
Methods for measurement of scapular movement
Method
Proposed by
Remark
Scapulohumeral regression
Scapula locator
[8,9]
[10–12]
Skin-mounted acromion tracker
Skin deformation, measured with markers
Digital fluoroscopy
[6,13]
[14]
[15,16]
Unsuitable for shoulder pathology
Acceptable method for clinical measurements, although there is always a small error because
exact replacement is impossible [5,10,12]. Requires static measurement positions
Valid up to 1208 humerus elevation, enables dynamic measurements
Requires minimal soft tissue coverage and muscle volume over the scapula. Preliminary results
Subjects exposed to radiation. So far, scapular motions only measured in one plane
acromion tracker was therefore developed, based on a cluster with
three markers. This acromion marker cluster (AMC) is different to
the ones used in other studies [6,13] due to its specifically designed
light-weight titanium frame (4 g) and small size of the base
(15 mm diameter) that can be accurately placed on the flat part of
the acromion.
Before applying the AMC, its accuracy would require evaluation, as part of the overall upper extremity 3D movement
evaluation using optoelectronic measurements. Generalization
from earlier evaluations would not be warranted since the AMC
design in this study was very light weight, compared to
electromagnetic trackers in previous studies [6,13]. Moreover,
the use of this type of AMC should encourage users of these
systems to include scapular kinematics in upper extremity
evaluation, which is not yet a common procedure [17]. The
existing literature is inconclusive concerning the under and overestimation of scapular movement by an acromion sensor. Meskers
et al. [13] found a general under-estimation of their acromial
method compared to scapula locator (SL) recordings with a
maximum rotation error of approximately 98. Karduna et al. [6]
found a maximal root mean square error of 11.48 for the acromial
method and reported an over-estimation for external rotation.
Therefore, we decided to study the accuracy of this AMC using the
SL method to serve as reference [11]. It was hypothesized that no
systematic error would be found between the results of the two
methods, at least up to 1208 humerus elevation. Since replacement of the acromion tracker was found to be a source of
variability [13], an assessment of the test/retest reliability of the
AMC was also included in our study.
2. Materials and methods
2.1. Subjects
Thirteen healthy subjects (six male and seven female), between 22 and 33 years
of age, were recruited for this study. Two different measurement protocols were
performed: a validation protocol and a reliability one. Four subjects performed both
protocols, seven subjects performed a validation protocol only, and two subjects
performed a reliability protocol only. Accordingly, there were eleven validation
measurements and six reliability measurements. The right shoulder of all subjects
was tested. Approval was obtained from the ethical committee of the Faculty of
Human Movement Science of the VU University in Amsterdam, and all subjects
provided informed consent.
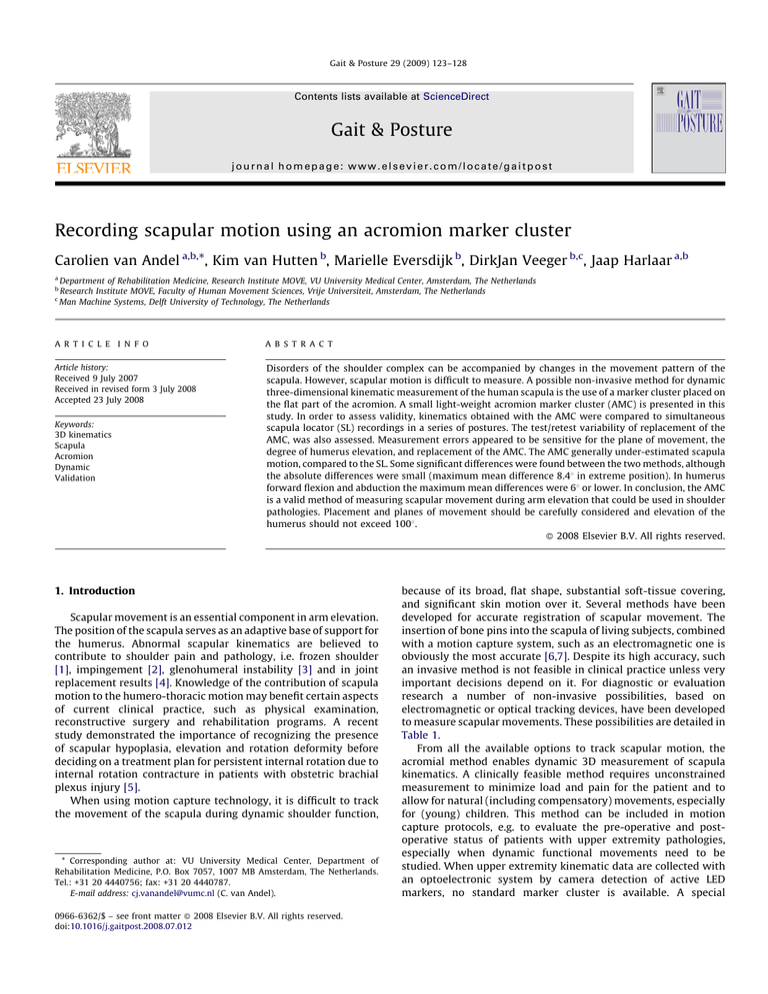
2.2. Instrumentation
3D kinematic data were collected by means of an Optotrak (Northern Digital Inc.,
Canada) system with 3 camera-sensors. This system is accurate up to 0.1 mm, and
the data were sampled at 50 Hz. Five clusters of markers were used to track the
thorax, scapula, scapula locator, upper arm and forearm and all clusters consisted of
three markers, except for the forearm cluster which consisted of six markers. The
thorax cluster was attached to the sternum with double-sided adhesive tape. The
upper arm cluster was attached to a cuff and strapped to the lateral arm just below
the insertion of the deltoid. A forearm cuff with six equally distributed markers was
strapped just proximally to the ulnar and radial styloids. Scapular movements were
recorded using two methods: (1) the AMC attached to the flat part of the acromion
with adhesive tape (Fig. 1), and (2) an SL. The SL is a fixture with an attached sensor,
holding three pins which can be adjusted to fit the landmarks on the scapula prior to
measurement. During the measurement, the investigator keeps the SL in close
contact with the bony landmarks of the scapula, slipping over the skin. The SL pins
were positioned on the acromial angle (AA), the root of the scapular spine (trigonum
spinae (TS)) and the inferior angle (AI) of the scapula.
To link the position of the marker cluster to local anatomical coordinate systems,
a standard pointer device was used to digitize 15 bony landmarks according to the
ISB standardization proposal for the upper extremity [18]. The proximal landmark
of the humerus, the glenohumeral rotation center, was estimated from scapular
Fig. 1. Positions of the SL with a cluster of three markers (A) and the acromion marker cluster that was placed on the flat part of the acromion (B).
C. van Andel et al. / Gait & Posture 29 (2009) 123–128
125
SL. Subsequently, the AMC was removed and then repositioned by the second
observer. This was followed by anatomical calibration. Again both observers
measured scapular movement with the SL. The order of examination by the first and
second observer was randomized.
2.4.1. Data analysis
BodyMech (www.bodymech.nl), a Matlab1 based open source package for 3D
kinematic analysis, was used and adapted to calculate joint kinematics from recorded
3D marker positions. In this study, motion of the scapula in relation to the thorax was
calculated for both methods (AMC and SL), with rotation order protraction/retraction
(Y), external/internal rotation (X) and anterior/posterior rotation (Z) [18].
For each posture, a generalized linear model analysis of variance (GLM-ANOVA)
with repeated measures (SPSS1 12.0.1) was performed to establish the difference
between the SL and the AMC recordings. Independent variables were method (SL
and AMC) and angle.
Reliability was assessed according to the Generalizability Theory, which is based
on analysis of variance (ANOVA) [19]. The components of variance that were
estimated with this analysis included the inter-subject variance, the variance
related to replacement and the error variance. Variance related to replacement and
error variance were used to calculate the standard error of measurement (S.E.M. = H
(replacement + error)).
3. Results
Fig. 2. The experimental set-up: a chair on which a semicircular pipe is fixed to
standardize arm positions.
bony landmarks by means of regression analysis [20]. From the combination of local
coordinate systems constructed from these anatomical landmarks and marker
cluster motions, it was possible to calculate global and relative orientations of
segment coordinate systems and subsequently the approximated joint rotations
(segment rotations) [18].
During the experiment, subjects were seated on a chair, with a semicircular
adjustable pipe fixed on it, in order to standardize the positions of the arm during
forward flexion and abduction (Fig. 2). Subjects were asked to point their index
finger once to the marks on the pipe. Measurements were performed by two
observers. Both were experienced human movement scientists and paramedical
specialists, and therefore had extensive experience with human anatomy and
palpation of anatomical landmarks.
2.3. Measurement procedures
2.3.1. Validation protocol
To validate the AMC the following postures were studied:
(1) Humerus forward flexion from 08 to 1208 with the elbow in full extension.
(2) Humerus abduction from 08 to 1208 with the elbow in full extension.
(3) Humerus rotation from 608 internal to 908 external, in 908 abduction and the
elbow in 908 flexion.
The subjects moved their arm through the desired arc in steps of 308. The interval
from 908 to 1208 of humerus elevation (postures 1 and 2) was measured in steps of
108, because it was expected that the maximum valid measurement of the position
of the scapula with the AMC would be approximately 1208 humerus elevation
[6,13]. These three postures were measured in random order. The AMC and the SL
measured scapular motion simultaneously (Fig. 1) and each position was measured
for 0.5 s. One successful measurement of each posture was required.
2.4. Reliability protocol
To assess the inter-trial variability of the AMC, six subjects performed a
reliability protocol. For this protocol the following positions were measured:
(1) Anatomical posture.
(2) 908 and 1208 humerus forward flexion with the elbow in full extension.
(3) 908 and 1208 humerus abduction with the elbow in full extension.
The first observer positioned the AMC for anatomical calibration, after which
both observers measured scapular movements for the different positions using the
Despite the standardization by means of semicircular pipes,
arm elevation resulted in variable humerus positions due to
variable elbow flexions, wrist flexions and thorax rotations. Also
fatigue during the course of the session, may have been of
influence. This resulted in a certain amount of variability in the
scapula positions. Moreover, the calculated thoracohumeral
elevation rarely exceeded 1108. The results of a recent study
[21] showed that the mean maximum humeral elevation appearing in a set of functional tasks is approximately 1008, therefore we
accepted the fact that 1208 of elevation was not reached by the
subjects. Scapula positions as a function of humerus elevation in
the validation protocol were approximated by a second order
polynomial, in order to compare subjects at equal and re-sampled
humerus elevation angles of 208, 408, 608, 808 and 1008.
3.1. Validation protocol
The mean recordings of the SL and the AMC over all subjects and
the error between the two methods were calculated for each of the
postures. Fig. 3 presents the graphs of these calculated values for the
postures forward flexion (Fig. 3a), abduction (Fig. 3b) and internal/
external rotation (Fig. 3c). The differences and interaction effects
between the two methods for each posture are shown in Table 2.
In general, there was no significant difference between the two
methods, except for external rotation during abduction. Overall,
the recordings of the AMC showed a larger standard deviation than
the recordings of the SL, and the standard deviation increased with
humeral elevation (Fig. 3a and b). Although the error graphs show
that the mean difference did not exceed 8.48, the error bars indicate
that some individual subject differences reached extreme values of
approximately 258. Further investigation showed that these
extreme values occurred during abduction above 908 and in the
extremes of internal/external rotation. In these particular cases the
scapular movements indicated by the AMC were remarkably lower
than those indicated by the SL. Mostly, the AMC under-estimated
the scapular movements, compared to the SL, except for
protraction and external rotation during forward flexion and
spinal tilt at 908 external rotation.
3.2. Reliability protocol
The results of the reliability assessment for the AMC are shown
in Table 3. Overall, ICC values for protraction and external rotation
were found to be acceptable to good. For spinal tilt the ICC values
126
C. van Andel et al. / Gait & Posture 29 (2009) 123–128
Fig. 3. The results of the validation protocol in (a) humerus forward flexion, (b) humerus abduction and (c) internal and external rotation at 908 humerus abduction. The upper
graphs show the mean recordings over all subjects by the SL (blue line, chequered) and the AMC (pink line, squares) with their standard deviation and the lower graphs show
the mean difference (error) between both methods with standard deviations (below), all for each of the three scapular movements (protraction, external rotation and spinal
tilt). The mean difference was calculated by subtracting the mean recordings of the SL cluster from the mean recordings of the AMC (For interpretation of the references to
color in this figure legend, the reader is referred to the web version of the article).
were low. A maximal S.E.M. of 8.48 was found in spinal tilt at 1208
humeral forward flexion. The amount of measurement error had a
maximal value of 8.48, which is equal to the mean maximal error
found in the validation study.
4. Discussion
In general, scapular movements recorded by the AMC are
similar to recordings made with the SL. During the internal and
external rotation posture the maximum mean difference did not
exceed 8.48 (found in protraction). During forward flexion and
abduction of the humerus, the maximum mean differences were 68
or lower. These findings are similar to the errors found by Meskers
et al. [13], who reported a maximum mean difference of 68 in
protraction during forward flexion and 98 in external rotation
during abduction. The standard deviations found in this present
study, varying from 3.58 to 9.58, are within the range described by
Karduna et al. [6], who found a root-mean-square error varying
from 1.18 to 11.48. The SL is also prone to error, however, the
anatomical points of the scapula that are used to align the SL, are
the most distal ones. Minor misalignments in placing the SL will,
therefore, not cause much effect. Therefore, given the choice to use
C. van Andel et al. / Gait & Posture 29 (2009) 123–128
127
Fig. 3. (Continued ).
Table 2
Results of the ANOVA for repeated measurements with scapular movement (protraction, external rotation and spinal tilt) as dependent and method (SL and AMC) and angle as
independent variables
Posture
Scapular movement
Mean (S.D.) (8)
SL
AMC
Method (significance)
Method* angle (significance)
1. Humerus forward flexion
Protraction
External rotation
Spinal tilt
34.6 (9.6)
23.2 (5.0)
1.4 (3.8)
38.8 (12.3)
24.9 (5.6)
3.2 (7.7)
0.028*
0.121
0.286
0.105
0.163
0.107
2. Humerus abduction
Protraction
External rotation
Spinal tilt
26.6 (7.7)
30.6 (7.6)
1.8 (6.3)
23.5 (12)
28.0 (7.3)
0.3 (9.7)
0.237
0.021*
0.312
0.679
0.080
0.292
3. Humerus internal/external rotation
Protraction
External rotation
Spinal tilt
27.1 (7.0)
34.7 (7.7)
2.0 (5.8)
21.9 (13.1)
31.2 (8.5)
1.1 (9.3)
0.064
0.090
0.244
0.03*
0.524
0.006**
*
**
Significant at p < 0.05.
Significant at p < 0.01.
a non-invasive reference method, the SL is considered the best
possible solution. An invasive method like 3D RSA would, however,
yield the highest accurate golden standard [22].
General under-estimation of scapular movements recorded by
the AMC compared to the SL, was also found by Meskers et al. [13]
but is partly in contradiction with Karduna et al. [6]. Individual
anatomical characteristics such as muscle mass and subcutaneous
tissue may represent a possible explanation for this underestimation. Especially above 908 of humerus elevation the deltoid
muscle contraction causes alternation in the shape of soft tissues.
Another factor could be skin to bone displacement. Both muscle
bulging and skin to bone displacement lead to a loss of contact
between the AMC and the acromion. This can result in an underestimation of scapular movement by the AMC, because skin and
muscle limit the movements of the AMC while the scapula
continues moving during elevation. These anatomical characteristics, unique to each individual, may also explain the large error
observed in some individuals during abduction, particularly above
908 humerus elevation. In addition to general under-estimation,
the AMC over-estimated two scapular movements, compared to
the SL: protraction and external rotation during forward flexion of
the humerus. Karduna et al. [6] also reported an over-estimation
during external rotation. During forward flexion the deltoid muscle
displaces only the anterior-lateral part of the AMC, while the
posterior part still contacts the acromion well. This results in a
larger external rotation by the AMC, more than the scapula actually
moves. Likewise, protraction may be influenced by the contracting
deltoid muscle.
As the deformity caused by the deltoid appears to be an
important factor affecting accuracy of the AMC in registering
scapular movements, placement of the AMC is a critical issue. The
large contribution of variance related to repositioning of the AMC
for all postures during protraction demonstrated the dependence
of protraction on AMC positioning. For the other two scapular
movements the variance caused by repositioning of the AMC was
negligible. Meskers et al. [13] also reported an effect of
repositioning of the AMC on the recorded scapular movement.
They stated that the acromial method of scapular recordings is only
precise when the recordings are compared without repositioning
the receiver. However, this is not possible in clinical practice.
C. van Andel et al. / Gait & Posture 29 (2009) 123–128
128
Table 3
Results of the AMC reliability measurements
Scapular movement Postures
Conflict of interest
Mean recordings (8) ICC S.E.M.
The authors declare that they have no competing interests.
AMC
Protraction
Anatomical posture
908 humeral abduction
1208 humeral abduction
908 humeral forward flexion
1208 humeral forward flexion
23.4
22.5
22.4
43.1
41.4
0.79 4.3
0.76 6.3
0.73 7.7
0.78 6.1
0.66 8.0
External rotation
Anatomical posture
908 humeral abduction
1208 humeral abduction
908 humeral forward flexion
1208 humeral forward flexion
11.1
28.4
38.1
31.2
37.6
0.84 3.4
0.65 4.2
0.72 3.9
0.84 3.8
0.71 4.1
Spinal tilt
Anatomical posture
908 humeral abduction
1208 humeral abduction
908 humeral forward flexion
1208 humeral forward flexion
3.5
0.1
4.2
2.6
0.1
0.36 7.7
0.30 7.0
0.59 7.3
0.29 6.6
0.29 8.4
Abbreviations: ICC, intraclass correlation coefficient; S.E.M., standard error of
measurement, presented in absolute values.
ICCagreement = variability inter-subject/(variability inter-subject + variability of
replacement + error variability).
Therefore, reducing the error caused by fixation and calibration
after repositioning of the AMC requires further investigation. In
general, external rotation movements are accurately recorded by
the AMC, as shown by the high or acceptable ICC values and
insensitivity to repositioning of the AMC. For all scapular movements, the S.E.M. value lies within the found mean maximal error
of 8.48 in the validation study.
There are, however, some limitations. Increasing the amount of
humerus elevation affected all scapula rotations, and the plane of
movement and repositioning of the AMC affected movements in
protraction. The small range of spinal tilt (approximately 108),
which was close to the maximal mean error of 8.48 found in the
present study, makes recording of this scapular motion by the AMC
questionable. This is also reflected in low ICC values for spinal tilt.
Despite the fact that the hypothesis of an unambiguous
relationship between the results of the SL and the AMC, at least
up to 1208 humerus elevation, could not be entirely confirmed, the
AMC that was investigated in this study was found to be a valid
method to detect abnormalities and differences above 8.48. This is
below the range of abnormal scapular movement found in
pathologies such as stroke (e.g. a diminished protraction of 168,
compared to healthy subjects) reported by Meskers et al. [23] and
impingement syndrome (e.g. a lower posterior tilting of 9.58,
compared to healthy subjects) [24].
In conclusion, we found that the AMC allows dynamic and
unconstrained recording of scapular motion. We recommend the
use of an AMC as part of motion capture protocols evaluating upper
extremity functional movements. Interpretation of results of the
AMC are however not recommended above 1008 elevation, and
only deviations and differences above 8.48 can be concluded. These
values can, however, be considered a clinically meaningful
measure, except for spinal tilt.
Acknowledgements
The authors would like to thank all the volunteers who
participated in this study. We also gratefully acknowledge Nienke
Wolterbeek’s contribution to the measurements.
References
[1] Vermeulen HM, Stokdijk M, Eilers PH, Meskers CG, Rozing PM, Vliet Vlieland
TP. Measurement of three dimensional shoulder movement patterns with an
electromagnetic tracking device in patients with a frozen shoulder. Ann
Rheum Dis 2002;61(2):115–20.
[2] Ludewig PM, Cook TM. Alterations in shoulder kinematics and associated
muscle activity in people with symptoms of shoulder impingement. Phys
Ther 2000;80(3):276–91.
[3] Matias R, Pascoal AG. The unstable shoulder in arm elevation: a three-dimensional and electromyographic study in subjects with glenohumeral instability.
Clin Biomech 2006;21(Suppl. 1):S52–8.
[4] Veeger HE, Magermans DJ, Nagels J, Chadwick EK, van der Helm FC. A
kinematical analysis of the shoulder after arthroplasty during a hair combing
task. Clin Biomech 2006;21(Suppl. 1):S39–44.
[5] Nath RK, Lyons AB, Melcher SE, Paizi M. Surgical correction of the medial
rotation contracture in obstetric brachial plexus palsy. J Bone Joint Surg Br
2007;89(12):1638–44.
[6] Karduna AR, McClure PW, Michener LA, Sennett B. Dynamic measurements of
three-dimensional scapular kinematics: a validation study. J Biomech Eng
2001;123(2):184–90.
[7] McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional
measurement of scapular kinematics during dynamic movements in vivo. J
Shoulder Elbow Surg 2001;10(3):269–77.
[8] Veeger HEJ, Vanderhelm FCT, Rozendal RH. Orientation of the scapula in a
simulated wheelchair push. Clin Biomech 1993;8(2):81–90.
[9] de Groot JH, Brand R. A three-dimensional regression model of the shoulder
rhythm. Clin Biomech 2001;16(9):735–43.
[10] Johnson GR, Stuart PR, Mitchell S. A method for the measurement of
3-dimensional scapular movement. Clin Biomech 1993;8(5):269–73.
[11] Meskers CG, Vermeulen HM, de Groot JH, van Der Helm FC, Rozing PM. 3D
shoulder position measurements using a six-degree-of-freedom electromagnetic tracking device. Clin Biomech 1998;13(4–5):280–92.
[12] Barnett ND, Duncan RD, Johnson GR. The measurement of three dimensional
scapulohumeral kinematics—a study of reliability. Clin Biomech
1999;14(4):287–90.
[13] Meskers CG, van de Sande MA, de Groot JH. Comparison between tripod
and skin-fixed recording of scapular motion. J Biomech 2007;40(4):
941–6.
[14] Brackbill E, Hall S, Richards J, Haight J. A novel method of scapular tracking
using tissue deformation. In: Proceedings of the 12th annual GCMAS meeting;
2007.
[15] Talkhani IS, Kelly CP. Movement analysis of asymptomatic normal shoulders: a
preliminary study. J Shoulder Elbow Surg 2001;10(6):580–4.
[16] Mandalidis DG, Mc Glone BS, Quigley RF, McInerney D, O’Brien M. Digital
fluoroscopic assessment of the scapulohumeral rhythm. Surg Radiol Anat
1999;21(4):241–6.
[17] Petuskey K, Bagley A, Abdala E, James MA, Rab G. Upper extremity kinematics
during functional activities: three-dimensional studies in a normal pediatric
population. Gait Posture 2007;25(4):573–9.
[18] Wu G, van Der Helm FC, Veeger HE, Makhsous M, Van RP, Anglin C, et al. ISB
recommendation on definitions of joint coordinate systems of various joints
for the reporting of human joint motion—Part II: shoulder, elbow, wrist and
hand. J Biomech 2005;38(5):981–92.
[19] Roebroeck ME, Harlaar J, Lankhorst GJ. The application of generalizability
theory to reliability assessment: an illustration using isometric force measurements. Phys Ther 1993;73(6):386–95 [discussion 396–401].
[20] Meskers CG, van Der Helm FC, Rozendaal LA, Rozing PM. In vivo estimation of
the glenohumeral joint rotation center from scapular bony landmarks by
linear regression. J Biomech 1998;31(1):93–6.
[21] van Andel CJ, Wolterbeek N, Doorenbosch CA, Veeger DH, Harlaar J. Complete
3D kinematics of upper extremity functional tasks. Gait Posture 2008;27:
120–7.
[22] Bey MJ, Zauel R, Brock SK, Tashman S. Validation of a new model-based
tracking technique for measuring three-dimensional, in vivo glenohumeral
joint kinematics. J Biomech Eng 2006;128(4):604–9.
[23] Meskers CG, Koppe PA, Konijnenbelt MH, Veeger DH, Janssen TW. Kinematic
alterations in the ipsilateral shoulder of patients with hemiplegia due to
stroke. Am J Phys Med Rehabil 2005;84(2):97–105.
[24] Lukasiewicz AC, McClure P, Michener L, Pratt N, Sennett B. Comparison of
3-dimensional scapular position and orientation between subjects with and
without shoulder impingement. J Orthop Sports Phys Ther 1999;29(10):
574–83.