Neurorehabilitation and Neural Repair
advertisement

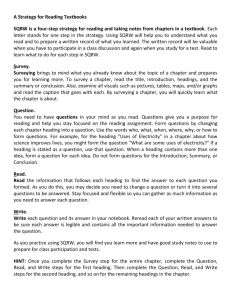
Neurorehabilitation and Neural Repair http://nnr.sagepub.com Stroke Affects Locomotor Steering Responses to Changing Optic Flow Directions Anouk Lamontagne, Joyce Fung, Bradford McFadyen, Jocelyn Faubert and Caroline Paquette Neurorehabil Neural Repair 2010; 24; 457 originally published online Jan 12, 2010; DOI: 10.1177/1545968309355985 The online version of this article can be found at: http://nnr.sagepub.com/cgi/content/abstract/24/5/457 Published by: http://www.sagepublications.com On behalf of: American Society of Neurorehabilitation Additional services and information for Neurorehabilitation and Neural Repair can be found at: Email Alerts: http://nnr.sagepub.com/cgi/alerts Subscriptions: http://nnr.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav Citations http://nnr.sagepub.com/cgi/content/refs/24/5/457 Downloaded from http://nnr.sagepub.com at MCGILL UNIVERSITY LIBRARIES on June 20, 2010 Research Articles Stroke Affects Locomotor Steering Responses to Changing Optic Flow Directions Neurorehabilitation and Neural Repair 24(5) 457–468 © The Author(s) 2010 Reprints and permission: http://www. sagepub.com/journalsPermissions.nav DOI: 10.1177/1545968309355985 http://nnr.sagepub.com Anouk Lamontagne, PhD,1 Joyce Fung, PhD,1 Bradford McFadyen, PhD,2 Jocelyn Faubert, PhD,3 and Caroline Paquette, PhD1 Abstract Background. Stroke patients manifest steering difficulties during walking, which may arise from an altered perception of visual motion. Objective.To examine the ability of stroke patients to control their heading direction while walking in a virtual environment (VE) describing translational optic flows (OFs) expanding from different directions. Methods. The authors evaluated 10 stroke patients and 11 healthy people while they were walking overground and visualizing a VE in a helmetmounted display. Participants were instructed to walk straight in the VE and were randomly exposed to an OF having a focus of expansion (FOE) located in 5 possible locations (0q, r20q, and r40q to the right or left). The body’s center of mass (CoM) trajectory, heading direction, and horizontal body reorientation were recorded with a Vicon-512 system. Results. Healthy participants veered opposite to the FOE location in the physical world, with larger deviations occurring at the most eccentric FOE locations. Stroke patients displayed altered steering behaviors characterized either by an absence of CoM trajectory corrections, multiple errors in the heading direction, or systematic veering to the nonparetic side. Both groups displayed relatively small CoM trajectory corrections that led to large virtual heading errors. Conclusions. The control of heading of locomotion in response to different OF directions is affected by stroke. An altered perception of heading direction and/or a poor integration of sensory and motor information are likely causes. This altered response to OF direction while walking may contribute to steering difficulties after stroke. Keywords heading, hemiparesis, kinematics, virtual reality, visual motion, walking Introduction The control of steering, or heading direction, is a requirement for goal-directed locomotion, allowing individuals to walk in the desired direction while avoiding obstacles along their path. Such control depends heavily on vision that provides information about the characteristics of the surrounding world and self-motion. Optic flow (OF) is a predictable pattern of visual motion generated at the moving eye during self-motion.1 Together with the perceived goal direction, it is one of the visual cues that can be used to control heading direction while walking.2-4 When walking straight, the OF describes a radial pattern of expansion with a focus of expansion (FOE) located in the direction of heading.4 When a change of direction is needed, the OF theory stipulates that the FOE is realigned with the desired heading direction.1 In support of this theory, it has been shown that offsetting the FOE of OF with prisms or through virtual reality causes healthy individuals to veer from their initial trajectory when instructed to walk straight ahead.2-4 Individuals who sustained a stroke are especially challenged in their daily activities as they have difficulties adapting their locomotion to environmental constraints. They show disrupted eye and body movement coordination patterns and altered walking trajectories when executing preplanned or cued changes of direction while walking, suggesting disrupted steering abilities.5,6 The loss of balance from executing a sudden turn of the head or body can result in a fall.7 Although motor deficits undoubtedly impair 1 School of Physical and Occupational Therapy, McGill University and Jewish Rehabilitation Hospital (Feil & Oberfeld/CRIR) Research Center, Montréal, Canada 2 Laval University and Québec Rehabilitation Research Institute (CIRRIS), Québec, Canada 3 School of Optometry, University of Montréal, Montréal, Canada Corresponding Author: Anouk Lamontagne, Jewish Rehabilitation Hospital (Feil & Oberfeld/ CRIR) Research Centre, 3205 Place Alton-Goldbloom, Laval (Québec), H7V 1R2, Canada Email: anouk.lamontagne@mcgill.ca 458 steering abilities, sensory deficits and altered sensorimotor integration are also likely to be involved.5,6 The ability to process different types of visual motion was shown to be altered by brain lesions in the occipitoparietal, parietotemporal, and posterior parietal regions possibly involving the MT (V5) complex.8-11 It would also be affected by a lesion of the frontal lobe.12 Whether such altered perception of OF direction translates into poor steering abilities after stroke, however, is not known. The goal of this study was to examine the ability of individuals with stroke to control their heading direction while walking in a virtual environment (VE) describing translational OFs expanding from different directions. It was hypothesized that these individuals would display an altered control of their heading direction in response to the shifts in the foci of expansion, as reflected either by reduced adjustments and/or directional errors in their walking trajectories. Methods Participants A convenience sample of 10 patients with stroke and 11 healthy persons participated in the study (Table 1). The 2 groups were of the same age (t test, P .12) and presented similar anthropometric characteristics. The inclusion criteria for the patients were the following: a first unilateral stroke in the middle cerebral artery (MCA) territory with residual deficits, confirmed by computerized tomography; walking independently over 10 m, with or without a walking aid, at a walking speed inferior to 1.0 m/s; and presenting with significant motor deficits of the affected lower limb, as reflected by a Chedoke-McMaster leg and foot impairment inventory score of less than 7.13 Exclusion criteria for the patients were the following: cognitive problems compromising the ability to give informed consent and to follow instructions as well as the presence of a visual field defect, as assessed by the Goldman visual field and/or equivalent computerized test. Patients with stroke were also free of visual spatial neglect, as assessed by the Bell’s Test14 or Star Cancellation Test,15 except for 2 of them (Table 1, patients S3 and S4) who were enrolled in the study before neglect was confirmed. When appropriate, the behavior of these 2 patients is described separately. Both healthy participants and those with stroke were free of visual problems not corrected by eyewear as well as of other neurological or orthopedic conditions interfering with locomotion. All participants signed an informed consent document, and the project was approved by the Montréal Center for Interdisciplinary Research in Rehabilitation (CRIR) establishments’ Research Ethics Board. Neurorehabilitation and Neural Repair 24(5) Setup and Procedures Participants were evaluated while walking overground at their comfortable speed in a large open space (12 m u 8 m), with their walking aid when applicable (see walking aid description, Table 1). They were visualizing, in a helmetmounted display (HMD) unit, a VE representing a large (40 m u 25 m) and symmetrical room created in Softimage XSI (Figure 1A). The virtual room was created to provide a richtextured VE and had pillars at its extremities,3 which were separated by 8 m. The HMD (Kaiser Optics ProView XL50) had a field of view of 50q diagonal, 30q vertical by 40q horizontal. Three-dimensional body coordinates were recorded using a 10-camera Vicon-512 motion capture system (Denver, CO). Passive reflective markers were located on specific body landmarks according to the PlugIn-Gait Model from Vicon, except for the head that was represented by a 3-marker model with markers located on the front, left side, and right side of the HMD. Location of the body’s center of mass (CoM) was calculated based on a 15-segment kinematic model and the anthropometric characteristics of the participants. The 3D head coordinates were tracked in real time by the Tarsus real-time engine from Vicon and fed to the Caren-2 virtual reality system from Motek (Motek Medical, Amsterdam). This feedback system synchronized the virtual scene in real time with head motions through the physical space (Figure 1B). When applicable, a visual perturbation could also be superimposed onto the motion of the scene caused by the head displacements of the participants. The delay in updating the virtual reality display in the HMD is less than 10 ms. The sampling frequency was set at 120 Hz. As they were walking forward, participants were exposed to a translational OF that was expanding from a FOE located in 5 possible locations (Figure 1C): 40q and 20q to the left or nonparetic side, 0q, as well as +20q and +40q to the right or paretic side. A FOE angular offset (4) was obtained by translating the scene laterally (x) based on the participant’s forward displacement (y), such that x ytan(4). Based on the forward walking speed of the participants, this corresponds to average rates of mediolateral translation of the scene of 0.32 m/s (r40q FOE) and 0.14 m/s (r20q FOE) for the patients and to 0.64 m/s (r40q FOE) and 0.28 m/s (r20q FOE) for the healthy controls. Participants were instructed to walk straight in the VE, that is, to “walk straight with respect to the scene they were visualizing in the HMD,” as opposed to the physical world. For a FOE located at 20q to the right, for instance, participants should perceive their virtual heading direction as translating forward and toward the right (Figure 1D). In an attempt to walk straight, they should veer to the left in the physical world, such that their walking trajectory remains around neutral (0q) in the virtual world. They 459 73 79 51 73 68 79 S5 S6 S7 S8 S9 S10 7M/4F — — — 8M/2F M M M M F F M M M M Gender (F/M) 169 11 155-183 166 12 152-185 172 162 152 185 154 155 152 178 176 173 Height (cm) 79 13 63-104 70 15 48-96 70 50 60 96 90 48 68 72 73 75 Weight (kg) 0.73 0.18 0.50-1.00 0.44 0.23 0.20-0.80 0.20 (Quad) 0.20 (Cane) 0.60 (2 Canes) 0.66 0.34 0.3 (Cane) — — — — 1-51 Months — — N N N N N N Y Y N N Neglect (Y/N) 12.6 3.0 Months 2.2 Months 2.1 Months 51.0 Months 1.0 Months 2.9 Months 19.0 Months 14.0 Months 0.15 (Quad)b 0.18 (Quad) 27.7 Months 3.4 Months Time Since Stroke 0.35 (Cane) 0.80 Speed (m/s) — — — — R R L R L L R L R L Side of Lesion Intraparenchymal hemorrhage Ischemia Ischemia Ischemia Ischemia Ischemia Ischemia + small hemorrhage Massive Ischemia Ischemia + small hemorrhage Ischemia, lacunar Etiology 1 Capsulothalamicc 2 3 2 3 3 1 None 1 2a Groupa Temporoparietal junction, insular cortex Subcortical, postinternal capsule Frontotemporoparietal, basal ganglia Frontotemporoparietal, basal ganglia; caudate and thalamus spared Parietal, external capsule, and lenticular nucleus Parietal Subcortical, capsulethalamic Parietal periventricular region, thalamus Parietal Location of Cerebrovascular Accident Abbreviation: SD, standard deviation. a Individuals with stroke were assigned to different groups depending on their steering behaviors, as described in the Results section. (1) Minimal Veering Group; (2) Incongruous Veering Group; and (3) Nonparetic Veering Group. b The quad cane is a 4-legged cane. c Initial scans were negative. A subsequent report states the presence of a subcortical infarct in this patient having a contralateral sensorimotor involvement of the hemibody with mild dysarthria and dysphagia. 63 6 50-72 66 S4 Mean SD Range 71 S3 69 11 50-79 79 S2 Mean SD Range Controls (n 11) 50 Age (years) S1 Stroke (n 10) Table 1. Participant Characteristics 460 Neurorehabilitation and Neural Repair 24(5) Figure 1. This figure shows (A) the virtual room used for the experiment, (B) the control algorithm of the virtual environment (VE) is based on real-time tracking of head coordinates, (C) the different locations of the focus of expansion (FOE) used in the present experiment, and (D) a schematic representation of perceived, physical, and virtual walking trajectories. were provided with 3 to 5 practice trials, with and without perturbations, before the experiments. We also confirmed verbally that they understood the instruction, both prior to and after the data collection. Three trials per FOE location were recorded, for a total of 15 walking trials. Because of their limited endurance, participants with stroke succeeded in performing 2 to 3 trials per FOE location. An assistant was standing next to or walking along with the Downloaded from http://nnr.sagepub.com at MCGILL UNIVERSITY LIBRARIES on June 20, 2010 461 Lamontagne et al. Figure 2. Individual trials representing body center-of-mass (CoM) trajectory in the physical world (left panel) as well as heading orientation in the physical (middle panel) and virtual worlds (right panel) in (A) 1 healthy young individual and (B) 1 elderly control. CoM trajectories are illustrated in the anteroposterior (A/P) direction as a function of the mediolateral (M/L) direction. Heading angular orientations are illustrated as a function of CoM displacement along the A/P axis. Note that CoM and heading traces illustrated in this figure are referred to as positive when the participants are walking to the right. Trials at r40q in the healthy young individual were recorded only for a short distance because of large M/L deviations that were limited by the physical constraints of the room. Because of the forward and backward oscillations in body CoM position at gait initiation that lead to inconsistent heading orientations, the first 50 frames of each trials are not represented, so heading traces do not start at neutral position. participants at all times, and no falls occurred during the experiment. Outcome variables retained for analysis included CoM trajectory and horizontal orientations of head and feet with respect to the physical and virtual world’s coordinates. Displacement and angular orientation toward the right (controls) or the paretic side (stroke) are referred to as positive. In addition, heading direction was computed as the instantaneous angular orientation of body CoM trajectory along the mediolateral (x-axis) versus the anteroposterior (y-axis) direction. For every trial, heading orientation in the virtual world, also termed as virtual heading error, was estimated as the mean heading orientation measured between 2 m and 3 m of forward walking. When 3 m of forward walking could not be reached, the mean value between 2 m and maximal forward walking distance was used instead. Mean virtual heading errors were thereafter averaged across trials and participants. By convention, a negative heading error refers to an underestimation of the correction needed to reach a virtual heading of 0q, whereas a positive heading error means that participants overcorrected their walking trajectory. Within- and between-participant variabilities were obtained using standard deviation values calculated across trials and participants, respectively. Virtual heading errors and within-participant variability were compared across groups (stroke vs controls) and conditions (FOE location, 5 levels) using a 2-way analysis of variance for repeated measures. The relationships of the virtual heading errors with gait speed and age were assessed using Pearson correlation coefficients. Statistics were performed in Statistica with a level of significance accepted at P .05. Results Examples of CoM trajectory modulation of healthy participants in response to different FOE locations are illustrated in Figure 2. To help understand what a typical profile of modulation looks like, an example of a healthy elderly control is contrasted with that of a healthy young individual. For both participants, the CoM trajectory and heading 462 Neurorehabilitation and Neural Repair 24(5) Figure 3. Individual examples of body center-of-mass (CoM) trajectory in the physical world (left panel) as well as heading orientation in the physical (middle panel) and virtual worlds (right panel) in participants with stroke from the (A) Minimal Veering Group, (B) Incongruous Veering Group and (C) Nonparetic Veering Group. Axis labels and abbreviation are the same as in Figure 2, with the exception of positive CoM and heading traces indicating a displacement to the paretic side. Participants belonging to each group are identified as per their participant number in Table 1 (S1 to S10). Note that S2 is not shown in this figure and displayed a steering behavior similar to healthy controls. orientation in the physical world were characterized by a deviation in the direction opposite to the FOE location (left and middle panels). The amplitudes of the CoM trajectory and the heading corrections were scaled to the magnitude of the perturbation, being larger for the 40q than for the 20q and 0q perturbations. The healthy young individual displayed large yet incomplete heading corrections in the physical world (middle panel), resulting in heading errors that were biased toward the FOE location in the virtual world (right panel). This participant’s heading error, however, decreased in the virtual world and converged toward the midline (0q) as he continued walking forward. In comparison, the healthy elderly control presented with much smaller heading corrections in the physical world, resulting in larger heading errors in the virtual world. In comparison with healthy controls, stroke patients presented with a variety of steering behaviors, including heading corrections that were of the wrong magnitude and/ or in the wrong direction (Figure 3). Based on the steering behavior, patients were classified into 3 different groups. The Minimal Veering Group (n 3) presented with little or no modulation of their CoM trajectory and heading orientation in the physical world when exposed to FOE shifts. As a result, they displayed large heading errors in the virtual world that were approaching the magnitude of the FOE shifts. The Incongruous Veering Group (n 3) displayed 463 Lamontagne et al. Figure 4. Individual trials representing CoM trajectory as well as head and foot horizontal orientation in the physical and virtual worlds for 1 healthy control and 1 patient (S4) with visuospatial neglect. multiple and inconsistent directional errors, with heading corrections being made erratically sometimes toward the paretic and sometimes toward the nonparetic side for similar FOE perturbations. The Nonparetic Veering Group (n 3) veered to their nonparetic side in the physical world for most trials, regardless of the FOE location. This means that when the FOE was on the paretic side, participants corrected their heading in the expected direction by veering to their nonparetic side. When the FOE was shifted to the nonparetic side, however, they veered in the wrong direction, that is, the ipsilateral nonparetic side. This resulted in larger virtual heading errors for the paretic than the nonparetic side. Note that the 2 participants with stroke who had visuospatial neglect (S3 and S4) were included in the Minimal Veering Group and the Nonparetic Veering Group, respectively. One remaining participant with stroke (S2), not included in the 3 groups, displayed behavior identical to that of the healthy controls. An example of CoM trajectory modulation as well as of head and foot orientation is further detailed in Figure 4 for a healthy control and a stroke patient with visuospatial neglect. The CoM trajectory of the healthy control veered in the direction opposite to the FOE location in the physical world, but the correction remained incomplete, leading to some deviation error in the virtual world. The feet were aligned with the CoM trajectory in the physical world, but the head showed few changes in its orientation with FOEs of changing location. This head and foot orientation pattern is typical of what was observed in the healthy control group as well as in most participants with stroke. Alternatively, the patient with visuospatial neglect represented in Figure 4 invariantly veered to the nonparetic side, irrespective of the FOE location. As for the other patients in group 2, a directional error arose when the FOE was located toward the nonparetic side, which did not cause the patient to veer toward the paretic side in the physical world, as would be expected normally. For the patient shown in Figure 4, his head and nonparetic foot were oriented toward the nonparetic side in the physical world, whereas the paretic foot remained in a more toes-out and widened position. 464 Neurorehabilitation and Neural Repair 24(5) Figure 5. (A) Mean (1 SD) virtual heading errors as well as (B) mean within-participant and (C) between-participant variability of virtual heading responses for the patients and controls across the different locations of the FOE. In A, the negative polarity of the virtual heading errors indicates an undercorrection of the heading trajectory with respect to the virtual world’s coordinates. Statistically significant results are indicated in A and B. No standard deviation error bars or statistical analyses can be computed for between-participant variability in C. Abbreviations: SD, standard deviation; FOE, focus of expansion. The average heading orientations in the virtual world, or heading errors, were compared between patients and healthy participants across FOE locations (Figure 5). All participants undercorrected their heading in response to FOEs of changing direction. Virtual heading errors increased at more eccentric FOE locations, both for patients and healthy participants (P .01). Given the different behaviors observed in the stroke patients, their mean virtual heading errors 465 Lamontagne et al. were found to be similar to those of the healthy participants (P ! .05), despite a tendency for larger heading errors in the patients at r40q of FOE perturbation. Within-participant and between-participant variabilities in the heading responses, however, were larger in the patients than in the healthy group (P .05, within-participant). Heading errors of patients and healthy participants were not correlated with walking speed (R2 0.00-0.07; P ! .05) or age (R2 0.00-0.19; P ! .05). A qualitative analysis of the heading behavior of patients with respect to the lesion site or the use of walking aids did not reveal any identifiable relationships (Table 1). Discussion This study provides the first evidence that individuals who sustained a stroke can manifest altered locomotor steering behaviors when exposed to OFs expanding from different locations. Such altered behaviors are reflected by abnormally small adaptations and/or by directional errors in the participants’ walking trajectories as well as by an increased variability across trials. The present results are consistent with the attenuated and/or altered gait speed modulation responses of participants with stroke when exposed to OFs of changing speeds.16 It has been shown that healthy young individuals exposed to an artificially shifted FOE while walking veer in the direction opposite to the goal in the physical world so that a virtual heading error close to zero can be reached.4 We have also shown that the larger the shift in the FOE, the larger the walking trajectory deviation in the physical world, and the larger the virtual heading error.3 In other words, the corrections in the physical walking trajectory are insufficient to lead to straight walking trajectories in the virtual world, and the heading errors increase at more eccentric locations of FOE. Present data collected in healthy controls who are older than the young individuals tested previously in other studies do support these observations. Brain Lesion and Altered Heading Perception An absence of response characterized the Miminal Veering Group, and multiple heading errors were displayed by the Incongruous Veering Group. No qualitative relationship could be established between the patterns of heading responses and the localization of the brain lesion. It cannot be excluded that the different heading behaviors (absence of responses vs errors) may just be different expressions of the same inability to perceive or use OFs to complete the heading task. It is worth investigating, however, whether the damaged brain areas of our participants could lead to an altered discrimination of visual motion direction and heading. The intact human brain shows activation in the occipital, parietal, and temporal cortical areas while viewing radial OFs.17 The human MT (V5) complex, and more specifically the MST area, were shown to be highly sensitive to changes in the characteristics of the OF stimuli.17,18 Discriminating heading, depending on the nature of the visual stimulus, would involve a complex network comprising posterior brain areas such as KO and V3a,19-21 the MT complex,20,22 temporoparietal and occipitotemporal areas,19,20 and even frontal areas12,22 and subcortical/limbic structures.19 Altered processing of visual motion direction has been previously reported in participants with a stroke in the occipitoparietal, parietotemporal, or posterior parietal brain areas, which were all believed to involve the MT complex.8-11 In the present study, the MCA territory lesions would spare the posterior visual areas supplied by the posterior cerebral artery, but the MT complex, potentially supplied by both the MCA and posterior cerebral artery, could not be excluded. Some of our patients also presented hemorrhagic events, which potentially extended the lesion beyond the MCA territory. It is noteworthy that our patients who displayed altered steering behaviors had lesions that invariantly involved the parietal lobe and/or thalamus. The parietal area is a key site for the integration of multiple sources of sensory information,23,24 and it is involved in the control of steering.25 The thalamus relays sensory information to different cortical areas, contributing crucially to motor actions. It seems reasonable to assume that lesions in such areas affect multisensory integration and can alter heading behaviors. Some of our patients also displayed lesion involving the frontotemporal region. There is evidence from intact or damaged brain studies that the frontal lobe,12 and more specifically the dorsal premotor area,22,25 is involved in heading identification. Those studies involved a ground plane or a radial OF pattern, which can resemble the type of stimulus used in the present study. According to Peuskens et al,22 such activation in the dorsal premotor area could be “ . . . a final stage in a parieto-premotor visuomotor connection, specifically related to transformation of heading information . . . into motor schemes.”(p 2460) In light of those findings, it appears likely that our patients had brain lesions that altered the perception and/or integration of heading information. Altered Sensorimotor Integration and Visuomotor Control The present paradigm also involved a sensory scenario in which visual stimuli were incongruent with proprioceptive and vestibular information. The central nervous system has the ability to reweight relevant sources of sensory information in a context-dependent fashion to maintain postural equilibrium.26-28 The transient aftereffect of self-motion experienced after treadmill running29 is another indirect 466 evidence of such a sensory reweighting process. The ability to reweight the relevant source of information appears to be reduced in older individuals30-32 and after stroke,33 so that those with stroke may be unable to upregulate vision and resolve the sensory conflict to control their heading. It was also suggested that gaze reorientation is a fundamental component of a locomotor steering synergy while changing direction34,35 and that active gaze would contribute to identifying heading by providing extraretinal cues.36 Passive viewing of OFs also triggers eye movements for the purpose of image stabilization.37 This emphasizes the intimate relationship between gaze control, visual perception, and the control of heading. In those with stroke, the coordination of gaze and posture during locomotor steering was shown to be disrupted.5 This suggests that both perceptual and motor aspects of visuomotor control could contribute to their altered heading responses. Visuospatial Neglect Perhaps one of the most unexpected findings of the present study was the behavior observed in the Nonparetic Veering Group, which consisted of walking trajectories consistently deviating to the nonparetic side in the physical world. Closer examination of present data reveals that the directional error occurred when the FOE was located on the nonparetic side, which should have caused a turn to the paretic side. This is not likely to be a result of biomechanical factors because those with stroke tend to walk with a horizontal rotational bias of their body toward their paretic side, therefore, favoring a physical turn toward the paretic side.6 It has also been demonstrated that looking to the side at an object causes a slight curvature in one’s walking trajectory toward the direction of gaze.38 In the absence of reliable vision cues such as when walking blindfolded, a walking trajectory deviation contralateral to the eye or head rotation is observed instead.39 In the present study, head and foot starting positions were aligned with the room’s coordinates before the participants started to walk, but the eyes might have been oriented in one or another direction. Even if this was the case, however, the effect would be very limited as in Jahn et al,39 for instance, a gaze rotation of 35q leads to a small trajectory deviation of 2q to 4q. Results of our study also show that one of the participants of the Nonparetic Veering Group had neglect, whereas the 2 others were theoretically free of such problems. In neglect, the paretic hemispace is less attended, and the subjective midline would be displaced to the nonparetic or ipsilesional side.40 This predicts that those with neglect should steer toward their paretic side in an attempt to walk straight,41 a prediction that is not supported by the present results. In reality, there is conflicting evidence as to whether those with neglect veer to their paretic or nonparetic sides as they walk.41,42 It also remains possible that some of our Neurorehabilitation and Neural Repair 24(5) participants might have had far extrapersonal space neglect that was not picked up by paper-pencil tests.43 Limitations Our results outline the within-individual and interindividual variability of behavior usually observed in stroke. Given the exploratory nature of this study, inclusion criteria were purposely kept large, but factors such as walking capacity, chronicity, and the extent of the brain lesion may have contributed to the heterogeneity of behaviors. The nature of the brain imaging tool (CT scans) and variability in the depth of the information available in the patients’ charts also limited our interpretation of results in terms of the lesion site and its effects on heading behaviors. It is hoped that higher resolution imaging tools will help shed light on the role of specific brain areas in locomotor steering behaviors. Factors such as attention and the sense of presence (sense of “being there,” within the VE), which have not been quantified in this study, may also differ between those with stroke and healthy participants and account for some of the differences between the 2 groups. It could also be argued that gait speed, which was slower in the stroke participants, was partly responsible for their altered behavior. Indeed, walking faster or running, as compared with walking slower, reduces the deviations in walking trajectory when walking with shifted OFs,44 blindfolded,45 or when presenting a vestibular imbalance. 46 However, the fact that larger heading errors were not associated with slower gait speeds in the present study suggests that speed is not an explanatory variable. It was unfortunate that gaze behavior could not be monitored in the present study. Although this limitation does not invalidate the present results, it also cannot reveal the presence or absence of an altered gaze behavior associated with the identification and control of heading direction in stroke participants. Conclusions and Future Directions The present results show that stroke affects the control of heading of locomotion in response to translational OFs expanding from different directions. An altered perception of heading direction and/or a poor integration of sensory and motor information are likely causes. Gaze shifts, which help in identifying heading direction through extraretinal cues, might also be involved, contributing in part to the altered heading behaviors. The altered heading responses to OF direction observed in the stroke participants may likely contribute to their steering difficulties. Future directions for research should include examining the effects of specific circumscribed brain lesions on locomotor steering behaviors as well as exploring the role of oculomotor control and the use of other sources of visual information, such as 467 Lamontagne et al. perceived target location, in the perception and control of locomotor heading after a brain lesion. Acknowledgments We would like to thank the people who participated in this study. We are also thankful to Eric Johnston and Christian Beaudoin for their skilful technical assistance. Authors’ Note Present address for Caroline Paquette: Neuroplasticity Laboratory, Department of Neurology and Neurosurgery, McGill University at SMBD-Jewish General Hospital and Lady Davis Institute, Montréal, Canada. Declaration of Conflicting Interests The authors declared no conflicts of interest with respect to the authorship and/or publication of this article. Funding This study was funded by the Québec Rehabilitation Research Network (REPAR), the Canadian Institutes of Health Research (CIHR) and the Heart and Stroke Foundation of Canada. A. Lamontagne is supported by a CIHR New Investigator Salary Award. Part of the equipment used for this experiment was funded by an infrastructure fund (New Opportunities Funds) from the Canada Foundation for Innovation. References 1. Gibson JJ. The visual perception of objective motion and subjective movement. 1954. Psychol Rev. 1994;101:318-323. 2. Harris JM, Bonas W. Optic flow and scene structure do not always contribute to the control of human walking. Vision Res. 2002;42:1619-1626. 3. Sarre G, Berard J, Fung J, Lamontagne A. Steering behaviour can be modulated by different optic flows during walking. Neurosci Lett. 2008;436:96-101. 4. Warren WH Jr, Kay BA, Zosh WD, Duchon AP, Sahuc S. Optic flow is used to control human walking. Nat Neurosci. 2001;4:213-216. 5. Lamontagne A, Fung J. Gaze and postural reorientation in the control of locomotor steering after stroke. Neurorehabil Neural Repair. 2009;23:256-266. 6. Lamontagne A, Paquette C, Fung J. Stroke affects the coordination of gaze and posture during preplanned turns while walking. Neurorehabil Neural Repair. 2007;21:62-67. 7. Hyndman D, Ashburn A, Stack E. Fall events among people with stroke living in the community: circumstances of falls and characteristics of fallers. Arch Phys Med Rehabil. 2002;83:165-170. 8. Plant GT, Laxer KD, Barbaro NM, Schiffman JS, Nakayama K. Impaired visual motion perception in the contralateral hemifield following unilateral posterior cerebral lesions in humans. Brain. 1993;116(pt 6):1303-1335. 9. Vaina LM, Soloviev S. First-order and second-order motion: neurological evidence for neuroanatomically distinct systems. Prog Brain Res. 2004;144:197-212. 10. Braun D, Petersen D, Schonle P, Fahle M. Deficits and recovery of first- and second-order motion perception in patients with unilateral cortical lesions. Eur J Neurosci. 1998; 10:2117-2128. 11. Vaina LM, Cowey A, Eskew RT Jr, LeMay M, Kemper T. Regional cerebral correlates of global motion perception: evidence from unilateral cerebral brain damage. Brain. 2001;124(pt 2):310-321. 12. Billino J, Braun DI, Bohm KD, Bremmer F, Gegenfurtner KR. Cortical networks for motion processing: effects of focal brain lesions on perception of different motion types. Neuropsychologia. 2009;47:2133-2144. 13. Gowland C, Stratford P, Ward M, et al. Measuring physical impairment and disability with the Chedoke-McMaster Stroke Assessment. Stroke. 1993;24:58-63. 14. Gauthier L, Dehaut F, Joanette Y. The Bells test for visual neglect: a quantitative and qualitative test for visual neglect. Int J Clin Neuropsychol. 1989;11:49-54. 15. Halligan P, Wilson B, Cockburn J. A short screening test for visual neglect in stroke patients. Int Disabil Stud. 1990;12:95-99. 16. Lamontagne A, Fung J, McFadyen BJ, Faubert J. Modulation of walking speed by changing optic flow in persons with stroke. J Neuroeng Rehabil. 2007;4:22. 17. Ptito M, Kupers R, Faubert J, Gjedde A. Cortical representation of inward and outward radial motion in man. Neuroimage. 2001;14:1409-1415. 18. Morrone MC, Tosetti M, Montanaro D, Fiorentini A, Cioni G, Burr DC. A cortical area that responds specifically to optic flow, revealed by fMRI. Nat Neurosci. 2000;3:1322-1328. 19. Beer J, Blakemore C, Previc FH, Liotti M. Areas of the human brain activated by ambient visual motion, indicating three kinds of self-movement. Exp Brain Res. 2002;143: 78-88. 20. Vaina LM, Soloviev S. Functional neuroanatomy of heading perception. In: Vaina LM, Beardsley SA, Rushton S, eds. Optic Flow and Beyond. New York, NY: Kluwer Academic Press; 2004:109-137. 21. Rutschmann RM, Schrauf M, Greenlee MW. Brain activation during dichoptic presentation of optic flow stimuli. Exp Brain Res. 2000;134:533-537. 22. Peuskens H, Sunaert S, Dupont P, Van Hecke P, Orban GA. Human brain regions involved in heading estimation. J Neurosci. 2001;21:2451-2461. 23. Meehan SK, Staines WR. Task-relevance and temporal synchrony between tactile and visual stimuli modulates cortical activity and motor performance during sensory-guided movement. Hum Brain Mapp. 2009;30:484-496. 24. Macaluso E, Driver J. Multisensory spatial interactions: a window onto functional integration in the human brain. Trends Neurosci. 2005;28:264-271. Downloaded from http://nnr.sagepub.com at MCGILL UNIVERSITY LIBRARIES on June 20, 2010 468 Neurorehabilitation and Neural Repair 24(5) 25. Field DT, Wilkie RM, Wann JP. Neural systems in the visual control of steering. J Neurosci. 2007;27:8002-8010. 26. Mergner T, Maurer C, Peterka RJ. A multisensory posture control model of human upright stance. Prog Brain Res. 2003;142:189-201. 27. Keshner EA, Kenyon RV, Langston J. Postural responses exhibit multisensory dependencies with discordant visual and support surface motion. J Vestib Res. 2004;14:307-319. 28. Mergner T, Schweigart G, Maurer C, Blumle A. Human postural responses to motion of real and virtual visual environments under different support base conditions. Exp Brain Res. 2005;167:535-556. 29. Durgin FH, Pelah A, Fox LF, Lewis J, Kane R, Walley KA. Self-motion perception during locomotor recalibration: more than meets the eye. J Exp Psychol. 2005;31:398-419. 30. Bugnariu N, Fung J. Aging and selective sensorimotor strategies in the regulation of upright balance. J Neuroeng Rehabil. 2007;4:19. 31. Mahboobin A, Loughlin PJ, Redfern MS. A model-based approach to attention and sensory integration in postural control of older adults. Neurosci Lett. 2007;429:147-151. 32. O’Connor KW, Loughlin PJ, Redfern MS, Sparto PJ. Postural adaptations to repeated optic flow stimulation in older adults. Gait Posture. 2008;28:385-391. 33. Bugnariu N, Fung J. Stroke and selective sensorimotor strategies in the regulation of upright balance. Abstr Soc Neurosci. 2006;32:353. 34. Hollands MA, Patla AE, Vickers JN. “Look where you’re going!”: gaze behaviour associated with maintaining and changing the direction of locomotion. Exp Brain Res. 2002;143: 221-230. 35. Reed-Jones R, Reed-Jones J, Vallis LA, Hollands M. The effects of constraining eye movements on visually evoked steering responses during walking in a virtual environment. Exp Brain Res. 2009;197:357-367. 36. Wilkie R, Wann J. Controlling steering and judging heading: retinal flow, visual direction, and extraretinal information. J Exp Psychol. 2003;29:363-378. 37. Niemann T, Lappe M, Buscher A, Hoffmann KP. Ocular responses to radial optic flow and single accelerated targets in humans. Vision Res. 1999;39:1359-1371. 38. Cutting JE, Readinger WO, Wang RF. Walking, looking to the side, and taking curved paths. Percept Psychophys. 2002;64:415-425. 39. Jahn K, Kalla R, Karg S, Strupp M, Brandt T. Eccentric eye and head positions in darkness induce deviation from the intended path. Exp Brain Res. 2006;174:152-157. 40. Karnath HO. Subjective body orientation in neglect and the interactive contribution of neck muscle proprioception and vestibular stimulation. Brain. 1994;117(pt 5):1001-1012. 41. Huitema RB, Brouwer WH, Hof AL, Dekker R, Mulder T, Postema K. Walking trajectory in neglect patients. Gait Posture. 2006;23:200-205. 42. Robertson IH, Tegner R, Goodrich SJ, Wilson C. Walking trajectory and hand movements in unilateral left neglect: a vestibular hypothesis. Neuropsychologia. 1994;32:1495-1502. 43. Azouvi P, Bartolomeo P, Beis JM, Perennou D, PradatDiehl P, Rousseaux M. A battery of tests for the quantitative assessment of unilateral neglect. Restor Neurol Neurosci. 2006;24:273-285. 44. Jahn K, Strupp M, Schneider E, Dieterich M, Brandt T. Visually induced gait deviations during different locomotion speeds. Exp Brain Res. 2001;141:370-374. 45. Dickstein R, Ufaz S, Dunsky A, Nadeau S, Abulaffio N. Speed-dependent deviations from a straight-ahead path during forward locomotion in healthy individuals. Am J Phys Med Rehabil. 2005;84:330-337. 46. Brandt T, Strupp M, Benson J. You are better off running than walking with acute vestibulopathy. Lancet. 1999;354:746. Downloaded from http://nnr.sagepub.com at MCGILL UNIVERSITY LIBRARIES on June 20, 2010