Document 10739757
advertisement

The Multiple Migratory Mechanisms of Systemically Infused Mesenchymal Stem
Cells to Sites of Inflammation
by
Grace Sock Leng Teo
B.Eng, Nanyang Technological University (2009)
Submitted to the Harvard--MIT Health Sciences and Technology in Partial Fulfillment of the
Requirements for the Degree of
Doctor of Philosophy in Medical Engineering and Medical Physics
at the
MASSACHUSETTS INSTitrTE
MASSACHUSETTS INSTITUTE OF TECHNOLOGY
OF TECHNOLOGY
June 2014
JUN 18 2014
©Massachusetts Institute of Technology. All rights reserved.
LIBRARIES
A.
Signature redacted
Signature of Author
vard-MIT IAealth/cience's
Certified by
____________________Signature
ieno
ogy
Nov 15, 2013
redacted
Jeftr y-M. Karp, Ph.D.
Associate Professor of Medicine and Health
Certified by
S
'Th
sCo-Supervisor
Tehnk6gy, BWH
Signature redacted
Ghristopher V. Carman, Ph.D.
Thesis Co-Supervisor
Assistant Profegsor of Medicine, BIDMC
Certified by
Signature redacted
Charles P. Lin, Ph.D.
Thesis Co-Supervisor
Associate Professor of Medicin3gMGH
Accepted by
Signature redacted /
/,""Emery Brown, M.D., Ph.D.
Director, Harvard-NTW
ealth Sciences and Technology
Professor of Computational Neuroscience and Health Sciences and Technology
The Multiple Migratory Mechanisms of Systemically Infused Mesenchymal Stem
Cells to Sites of Inflammation
by
Grace Sock Leng Teo
Submitted to the Harvard-MIT Health Sciences and Technology on April 28, 2014 in Partial
Fulfillment of the Requirements for the Degree of Doctor of Philosophy in Medical Engineering and
Medical Physics
ABSTRACT
Systemically infused mesenchymal stem cells (MSC) are being explored for their
immunomodulatory therapeutic potential in multiple inflammatory pathologies. This therapeutic
potential has been associated with the ability of MSC to accumulate at sites of inflammation
following infusion. However, there is a poor understanding of the mechanisms that mediate MSC
trafficking to inflamed tissue. Here, we first introduce key concepts in MSC biology and cellular
trafficking, and highlight the relevance of MSC trafficking. We also introduce key concepts in
cellular trafficking, particularly the leukocyte homing cascade, as a framework to approach MSC
trafficking. Then, we review the field of MSC trafficking in the second chapter, particularly the
methods employed to study MSC trafficking and associated challenges. In the third chapter, we
study MSC ability to perform transendothelial migration, a specific step in the process of MSC
trafficking, using high resolution confocal and dynamic imaging techniques. We found that MSC
transmigration is associated with both leukocyte-like and novel mechanisms, including nonapoptotic migratory blebbing. In the fourth chapter, we address the importance of non-endothelial
factors in MSC trafficking to inflamed tissues, including mechanical trapping in small vessels,
secondary interactions with endogenous immune cells and vascular permeability. Finally, we
conclude by proposing an integrated model of mesenchymal trafficking versus hematopoietic
trafficking, and highlight the potential role of the intravascular compartment as a major site of MSC
immunomodulation. We believe that this body of work has a broad impact on our understanding of
MSC biology and therapeutic potential, our comprehension of mesenchymal cell trafficking
(including metastasis) and the design of cell delivery strategies for clinical translation.
Thesis Co-Supervisor: Jeffrey M. Karp
Title: Associate Professor of Medicine and Health Sciences and Technology, BWH
Thesis Co-Supervisor: Christopher V. Carman
Title: Assistant Professor of Medicine, BIDMC
Thesis Co-Supervisor: Charles P. Lin
Title: Associate Professor of Medicine, MGH
3
4
ACKNOWLEDGEMENTS
My research co-advisors. Prof. Jeffrey Karp, your active support of my education and career is
unquestionably a major reason I entered science and research to start with. I am immensely grateful
for your confidence in me. The opportunities you have given me to challenge myself and grow in the
Karp Lab are innumerable. Prof. Christopher Carman, most of my favorite science conversations
have been with you. Thank you for sharing the moments of exciting discoveries and guiding me
through the more mundane and tortuous times. You are one of the biggest influences in the way I
think about biology. Prof. Charles Lin, without your support I would not have been able to
complete my PhD. Thank you for taking me into your lab and your encouragement from the start.
My thesis committee members, Prof. Elazer Edelman and Prof. Carla Kim, thank you for your
critical feedback and pushing me to my fullest potential.
Members of the Karp, Carman and Lin laboratories, especially Debanjan Sarkar, James Ankrum,
Kelvin Ng, Shrey Sindhwani, Oren Levy, "Jay" Zijiang Yang, Megan Connelly, Roberta Martinelli,
Peter Sage, Rens Zonneveld, Luke Mortensen, Judith Runnels and Clemens Alt. Your mentorship,
collaboration, generous help and encouragement would have been impossible to do without. The
lunch and coffee breaks I have taken with you have helped to shape my PhD.
My undergraduate interns, especially Sarah Boetto and Kayla Simms. For the times that I was able to
mentor you, you were often the highlight of my work day.
The house sisters of Alpha Chi Omega - Theta Omicron Chapter. You have been the best study
breaks from thesis writing I could ask for.
Friends in Singapore and Europe, especially Elizabeth Chay, Adele Lee, Amy Tan, Shufen Chew,
Ee-reh Owo. Trans-atlantic friendships are hard to come by; your support from far away has often
felt incredibly close.
Friends in Boston, especially Lynnae Ruberg, Caroline Barker, Kerri Trachsler, Jordan Grubb,
Cecilia Jiang, Julie Paul, Rachel Perez, Alice Tin, Cheryl Cui, Jonathan Ong, Anna and Sam Kim
(and the children), Stephen and Emily McAlpin and Benjamin and Katherine Hampson. You have
made Boston a second home for me.
My parents, Matthew and Kim Teo, and beautiful sisters, Joy and Amy. Thank you for loving me
through all, grounding me, sharing your wisdom and teaching me what matters most in life.
God. It has been a privilege discovering the wonders of your creation.
5
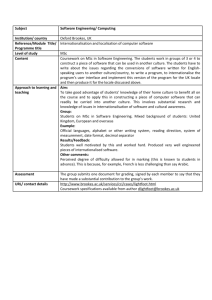
TABLE OF CONTENTS
Title
Page
Title Page
Abstract
Acknowledgements
Table of Contents
List of Tables
List of Figures
1
3
5
6
9
11
Introduction
Preface
1.1
1.2 Mesenchymal Stem Cells: Identity, Function and Therapeutic
Potential
Cellular Trafficking
1.3
1.4 Thesis Outline
13
13
13
20
27
2
A Comprehensive Review of Mesenchymal Stem Cell Trafficking
Preface
2.1
Introduction
2.2
Can MSCs be Mobilized into Peripheral Blood?
2.3
Factors Influencing the Distribution of Systemically Infused MSCs
2.4
Analyzing MSC Engraftment
2.5
Engineering Mesenchymal Stem Cell Trafficking
2.6
Summary and Prospective
2.7
28
28
28
31
32
34
47
48
3
A High-Resolution Microscopic Analysis of Mesenchymal Stem Cell
Transmigratory Ability In Vitro
Preface
3.1
Introduction
3.2
Methods
3.3
Results
3.4
Discussion
3.5
Supplemental Figures
3.6
Supplemental Videos
3.7
51
Chapter
1
51
51
53
59
75
80
85
Chapter
Title
Page
4
An Intravital Study of Mesenchymal Stem Cell Trafficking in a Murine
Model of Dermal Inflammation
Preface
4.1
Introduction
4.2
4.3
Methods
4.4
Results
4.5
Discussion
Supplemental Figures
4.6
Supplemental Videos
4.7
88
5
Conclusion
5.1
Using Microscopy to Study Cell Trafficking
5.2
A Hematopoietic versus Mesenchymal Model of Trafficking
5.3
Factors to Consider in Choosing Cell Types for Therapies Involving
Their Trafficking
5.4
The Intravascular Compartment as a Site of MSC
Immunomodulation
88
88
90
94
104
108
114
115
116
117
121
122
124
References
7
8
LIST OF TABLES
Table
Title
Page
1.1
2.1
2.2
5.1
5.2
Features of the three types of capillaries
MSC homing efficiencies after systemic delivery
Problems faced in the field of MSC trafficking
Characteristics of hematopoietic versus mesenchymal trafficking
Characteristics of amoeboid versus mesenchymal migration
25
41
49
120
120
9
10
LIST OF FIGURES
Table
Title
Page
2.1
2.2
3.1
The active MSC homing circuit
Model for passive versus active homing
MSC preferentially transmigrate through TNF-a activated lung and cardiac
endothelium
The 5 stages and 2 routes of MSC transmigration
MSC transmigration kinetics and absence of lateral migration
MSC exhibit extensive non-apoptotic blebbing on endothelium
MSC use non-apoptotic blebs to exert force on surroundings
Comparison between the leukocyte transmigration cascade and the proposed
MSC transmigration cascade
Analysis of endothelial adhesion molecule expression and MSC senescence
Impact of PTX on MSC viability and role of cytokines, VCAM-1 and
integrins MSC on adhesion and transmigration
Expression of tight and adherens junctional molecules at site of paracellular
migration
Extravasation kinetics and distribution of MSC in the inflamed ear
MSC and leukocyte distribution in the inflamed ear is correlated
Large fraction of intravascular MSC found in contact with neutrophils and
platelets
Platelet depletion decreased preferential trafficking of MSC to inflamed ear
30
35
60
Fraction of intravascular MSC in contact with neutrophils is maintained
after platelet depletion
Vascular permeability in inflamed ear increases after platelet depletion
Extravasation kinetics and distribution of MSC in the inflamed ear
MSC and leukocyte distribution in the inflamed ear is correlated
MSC adhere to neutrophil extracellular traps
103
3.2
3.3
3.4
3.5
3.6
S3.1
S3.2
S3.3
4.1
4.2
4.3
4.4
4.5
4.6
S4.1
S4.2
S4.3
11
63
66
69
72
76
80
82
84
95
97
99
101
103
108
110
112
12
CHAPTER ONE
INTRODUCTION
1.1 PREFACE
Mesenchymal stem cells (MSC) have gained much attention for their therapeutic potential.
Specifically, exogenously cultured MSC have been systemically infused into multiple models of
inflammatory disease, and observed to accumulate at sites of inflammation and exert
immunomodulatory effects. The focus of this thesis is the MSC ability to migrate to sites of
inflammation.
As an introduction, this chapter aims to orient the readers to the fields of MSC biology and
cellular trafficking.
MSC trafficking is an important process for both the physiological function and therapeutic
potential of MSC. Hence, elucidating the mechanisms underpinning this process will impact
both our understanding of MSC biology and our design of MSC therapeutics, as described in
Section 1.2.
The field of cellular trafficking has gleaned many insights from the study of leukocyte homing
and cancer metastasis. A holistic overview of the different migratory mechanisms employed by
different cell types, which forms the basis for investigating MSC trafficking, is described in
Section 1.3.
Finally, the thesis is outlined in Section 1.4.
1.2 MESENCHYMAL STEM CELLS: IDENTITY, FUNCTION AND THERAPEUTIC
POTENTIAL
1.2.1
Definitions and identity
Friedenstein and colleagues first demonstrated in the 1960s and 70s that a minor subpopulation
of cells from the bone marrow had osteogenic potential after heterotypic transplantation(1).
These cells were distinguishable from the majority of hematopoietic bone marrow cells by their
rapid adherence to tissue culture plastic, and fibroblast-like in vitro appearance. Based on the
13
presence of cells in the mesoderm which could also differentiate into both osteogenic and
cartilaginous cells in vitro, the concept of a MSC was then coined less than 3 decades ago(2).
Since then, the term "MSC" has generated much controversy. On one end of the spectrum, a
position paper was released by the International Society for Cellular Therapy (ISCT) to define
human MSC as satisfying the following criteria(3):
1. Plastic-adherent under standard culture conditions
2. Expresses CD105, CD73
CD79a/CD19, HLA-DR
and
CD90,
but
not
CD45,
CD34, CD14/CD11b,
3. Differentiates into osteoblasts, adipocytes and chondroblasts in vitro
It should be noted that based on this definition, MSC do not express any unique cell surface
marker, which contributes to the difficulty of identifying the in vivo analog of this in vitrodefined cell.
The ISCT definition has come under attack by researchers at the other end of the spectrum, who
feel that use of the term 'stem cell' should include the criteria of multipotency and self-renewal
ability, to prevent misconceptions by other researchers and the public(4, 5). These researchers
also believe that MSC should alternately be termed 'skeletal stem cells' (SSC) to reflect a much
more limited differentiation potential than has been attributed to these cells, and require
stringent clonogenic and in vivo multipotency assays during isolation.
This is in contrast to current isolation procedures of MSC largely based on plastic-adherence
which likely represent a very non-specific heterogenous population of stromal cells that can be
isolated from most tissues(4). Indeed, MSC based on the ISCT definition were found in virtually
every postnatal tissue and organ(6). In contrast, opponents to the ISCT definition believe that
MSC/SSC can only be isolated from bone marrow.
Currently, ISCT-defined MSC are widely used experimentally and in clinical trials. Hence, to
achieve the broadest impact, we have chosen to study ISCT-defined MSC, although their
heterogeneity likely precludes the elucidation of a single, well-defined trafficking mechanism.
1.2.1.1
Multipotency
Based on the ISCT definition, the multipotency of MSC has extended as far as having
seemingly transgermal differentiation potential. This refers to MSC the ability to
differentiate into cell types derived not only from mesoderm, but also ectoderm and
endoderm(7-9).
The more accepted differentiation potential of MSC is limited to adipogenic, osteogenic
and chondrogenic differentiation potential, as based on the ISCT definition, and
potentially other non-skeletal mesenchymal tissues(10). However, based on the standard
differentiation assays in the MSC field, the same opponents of the ISCT definition have
criticized these assays to merely indicate the "ability to accumulate (under artificial
chemical cueing) hydrophobic, mineralized or polyanionic materials"(5).
14
As an alternative to the ISCT definition, and based on the original MSC concept in
Friedenstein's work, it has been proposed that MSC/SSC should possess the ability of
single progenitor cells from bone marrow to form heterotypic ossicles in vivo(4). This
indicates a physiologically relevant ability to reconstitute all elements of the skeleton in
vivo in a cell autonomous manner, without the need for external cues.
1.2.1.2
Self-renewal
In addition to multi-potency, opponents to the ISCT definition further require evidence
of self-renewal capacity in vivo for MSC, much like the ability of single HSCs to
reconstitute the entire hematopoietic system of lethally irradiated animals. Here, MSCs
isolated from the heterotypic ossicles generated from a primary transplantation of MSC,
should again be able to generate heterotypic ossicles in a secondary transplantation to
demonstrate self-renewal ability(5).
1.2.2
Physiological function
As can be expected, the two opposing ISCT and SSC definitions of MSC are associated
with different understandings of the role of the MSC in a physiological state.
1.2.2.1
Hematopoietic stem cell support
The stem cell niche was first conceptualized in 1978(11), which proposes that stem cells
are maintained in a quiescent state by association with a discrete cellular
microenvironment. MSC/SSC and ISCT-defined MSC are both believed to be
osteoprogenitors residing in a perivascular position in the bone marrow, which support
the hematopoietic stem cell (HSC) niche. Several lines of evidence have been shown to
support the MSC as part of the HSC niche(12):
Rarity of MSC in the bone marrow. Since HSC only comprise 0.005-0.01% of bone
marrow cells, it is reasonable that niche cells should similarly be found at such low
density.
2) Physical proximity between MSC and HSC.
3) Synthesis of HSC maintenance genes by MSC.
4) Ability of MSC to specifically respond to signals that regulate HSC niche.
1)
Specifically, MCAM/CD146-expressing cells in the bone marrow stroma were recently
recognized to be able to self-renew and form heterotopic bone marrow in vivo, key
characteristics of MSC/SSC(13). Interestingly, these cells were found perivascularly in
assoiciation with sinusoidal endothelium, and produced high amounts of angiopoietin-1,
a key molecule of the HSC niche.
15
The role of MSC in the HSC niche was confirmed by another study, which labeled
Nestin+ cells in the bone marrow. These perivascular cells were found in close proximity
to HSC, expressed high levels of other HSC regulatory molecules, including
Angiopoietin-1, SCF and VCAM-1, that was downregulated by signals that typically
induce HSC mobilization(14). Further, these Nestin+ cells were innervated by SNS
fibers and expressed relatively high levels of f3 adrenegic receptors, CXCL12, and other
HSC regulatory molecules. Both adrenergic signals and CXCL12 have been found to
regulate HSC mobilization in vivo, while CXCL12-rich reticular cells were previously
recognized to be associated with HSC in the bone marrow(1 5). Most importantly, these
Nestin+ cells were able to generate ectopic bone, indicating their MSC/SSC identity.
In a follow-up study, depletion of CXCL12+ cells from mice induced HSC loss, and
bone marrow-derived CXCL12+ cells could also differentiate into osteoblasts and
adipocytes in vivo(16). These CXCL12+ cells also produced most of the stem cell factor
(SCF) in the bone marrow, a fact that has become more important in the light of a
recent study that found SCF+ cells to be mostly localized around sinusoids, the site of
MSC and HSC residence. When SCF production was deleted in LepR+ perivascular
cells, HSC numbers were altered(17), indicating that SCF+ cells had a role in HSC
maintenance.
Together, these evidence strongly support the role of MSC in supporting the HSC niche,
though it is currently unclear which cell surface markers might be the most specific for
MSC in the bone marrow, and how MSC-endothelial cell interactions may also be
important for HSC maintenance.
1.2.2.2
Vascular maintenance
A role for MSC in maintaining vascular function has also been proposed, though this is
largely for ISCT-defined MSCs. Indeed, the relationship of MSC and pericytes is of
great interest, as they seem to share many characteristics(18, 19). To note, the ISCT
definition of MSC is a purely in vitro definition, while pericytes have an in vivo
definition, hence it has been proposed that MSC are the in vitro analog of pericytes.
Firstly, pericytes have been shown to express many MSC markers and vice versa. MSC
isolated from multiple tissues, including brain, thymus, liver, kidney, bone marrow and
lung, expressed alpha smooth muscle actin (ctSMA), a pericytes marker(6). On the other
hand, pericytes isolated from multiple human organs based on expression of CD 146,
NG2, PDGF P expressed MSC markers in culture (20, 21).
Secondly, MSC are thought to reside in a perivascular position in vivo like pericytes.
MSC, which have been identified in vivo in the bone marrow using a Nestin marker,
were found to reside perivascularly(14). This is in addition to many other studies that
have isolated perivascular cells in multiple tissues and showed that the isolated cells
exhibit MSC characteristics(20, 22, 23).
16
Finally, MSC share functional characteristics of pericytes. Specifically, MSC can exert
stabilization effects on vasculature in vitro. During direct culture with endothelial cells,
vascular networks that formed with MSC persisted three times longer than without
MSC(24). In fact, functional vasculature formed by coculture of MSC and endothelial
cells were found to be stable for more than 130 days in vivo(25). MSC have also been
observed to have a pro-angiogenic effect in vivo. For example, there have been multiple
reports of MSC transplanted into models of myocardial ischemia, which have been
found to stimulate angiogenesis(26, 27). This potential has been further extended to
MSC function in tumors, where they similar increase tumor blood vessel density(28, 29).
1.2.2.3
Tissue renewal
The ability of MSC/SSC to form ectopic bone in vivo has naturally led to the theory that
MSC serve as stem cells that reconstitute the skeletal system. In addition, ISCT-defined
MSC have also been proposed to reconstitute other tissues. Interestingly, pericytes and
MSC have been found to have similar differentiation potential. Pericytes isolated from
multiple human organs were found to have osteogenic, chondrogenic and adipogenic
potential at the clonal level(20, 21). Indeed, this finding has been long preceded by
reports of the multipotency of pericytes(30), particularly in the osteogenic lineage(3133). These observations have also led to the hypothesis that MSC are a subpopulation of
pericytes that participate in homeostasis by acting as a reservoir of tissue-specific
progenitors. Indeed MSC isolated from different tissues have been found to have
preferentially differentiate into the parenchymal cells of the tissue they are isolated from,
supporting the notion that tissue-specific MSC contribute to the homeostasis of the
tissue in which they reside.
The SSC and ISCT definitions of MSC seem to meet a happy compromise in the final
possibility that MSC that reside in the bone marrow can migrate to other tissues, where
they serve as progenitor cells. Demonstrating this function requires that MSC in the
bone marrow can be labeled and tracked. A few studies have achieved this. In one, MSC
isolated from the bone marrow of transgenic EGFP mice was transplanted into lethally
irradiated mice with wild-type bone marrow cells. Subsequently, the MSC were found to
engraft in the bone marrow of the host, and contribute to intimal hyperplasia after
arterial ligation(34). Similar studies have also reported the migration of bone marrowresident MSC to endometrium(35-37) where they reconstituted both epithelium and
stromal cells, and to tumor sites where they promote cancer growth as cancer-associated
fibroblasts(38). In all cases, inflammatory signals (arterial ligation, endometrial
breakdown and repair during menstruation, and cancer) are thought to recruit MSC
from the bone marrow.
17
1.2.3
Therapeutic potential
There are several aspects of MSC therapeutic potential, including their
immunosuppressive activity, their ability to migrate to sites of inflammation for targeted
drug delivery and their use in tissue engineering.
1.2.3.1
Immunosuppressive activity
MSC immunosuppressive activity has been reviewed extensively elsewhere(39-43) and
will only be briefly covered here.
MSC have immunosuppressive effects on a range of immune cell types, including T
cells(44-46), B cells(47, 48), dendritic cells(49-51) and NK cells(52). The
immunosuppressive effects of MSC include the suppression of proliferation, activation
and migration of these cell types. Further, in models of wound healing e.g. myocardial
infarction, MSC can increase vascularization and decrease fibrosis(53-56). The
mechanism of MSC immunosuppressive activity is dependent on (i) paracrine factors
and (ii) direct cell-cell contact between MSC and cells of the immune system.
Several paracrine factors have been reported to mediate MSC immunosuppression. In a
model of myocardial infarction, MSC that were trapped in the lungs after systemic
infusion were found to form microembolisms, and consequently upregulate and secrete
TSG-6(57). TSG-6 is an anti-inflammatory protein, and the authors found that infusion
of TSG-6 was enough to recapitulate the therapeutic effects observed when MSC were
infused. Other soluble factors implicated in MSC immunosuppression include nitric
oxide(58), IDO(59), TGF-p(60), IL-10(59, 61) and PGE 2(59, 62). Further, multiple
reports have also shown that infusing MSC conditioned media can recapitulate MSC
therapeutic effects in vivo(63, 64), indicating the role of soluble factors in MSC
therapeutic ability.
Additionally, direct cell-cell contact between MSC and immune cells has also been
reported to be essential for MSC immunosuppression in some contexts. In one study, the
authors uncovered a novel role for adhesion molecules, ICAM-1 and VCAM-1,
expressed by MSC in immunosuppression(65). Earlier studies showed that MSC
secretion of NO was immunosuppressive; however, due to the short half-life of NO and
its limited range of diffusion, it is only potent within the local vicinity of MSC(58).
Hence, by adhering to T cells via ICAM-1 and VCAM-1, the proximity between MSC
and T cells was close and stable enough to achieve the immunosuppressive effect
mediated by NO(65). Other studies have similar shown cell-cell contact to important for
MSC immunosuppression of NK cells(52) and dendritic cells(66).
While MSC and immune cells both accumulate at sites of inflammation, the
requirement for MSC accumulation for immunosuppression seems to be context
dependent. In one study, activated dendritic cell migration from the flank to the lymph
18
node was impaired just 10 min after MSC infusion. Since the majority of MSC are
trapped in the lungs immediately after infusion, this strongly suggested that MSC
accumulation at the site of inflammation was not required for the observed
immunosuppressive effect(67). Interestingly, there is a potential that the adrenergic
signaling in the nervous system may also contribute to MSC immunosuppression,
accounting for the rapid kinetics in which MSC seemed to exert an immunosuppressive
effect in this study. Indeed, p2-adrenergic receptors are present throughout the lung(68)
where the majority of MSC rapidly accumulate following systemic infusion. Further,
adrenergic signaling has been shown to be important in inducing HSC mobilization
from the bone marrow - a significant observation given that MSC are an important
component of the HSC niche(69) and are thus likely responsive to adrenergic signaling.
Thus, it is conceivable that MSC may induce systemic immunosuppressive effects
through adrenergic signaling from their non-specific trapping in the lungs.
In contrast, other studies have reported a therapeutic effect associated with the specific
accumulation of MSC at sites of inflammation. In a model of myocardial infarction,
increasing MSC adhesiveness (by eliminating reactive oxygen species) increased MSC
engraftment in the heart 3 days after transplantation, and was associated with improved
therapeutic outcome(70). Similarly, in another study, MSC therapeutic effect in a model
of Sjogren's disease was reduced after CXCR4 blockade, which decreased MSC
engraftment in the salivary gland(71). Future studies will be needed to parse the systemic
and local immunomodulatory effects of MSC. Importantly, a better understanding of the
migratory mechanisms of MSC after systemic infusion will be very helpful to modulate
the biodistribution of MSC, and thus isolate the site-specific effects of MSC.
1.2.3.2
Targeted delivery
The accumulation of MSC at sites of inflammation has also lent itself to the possibility of
using MSC as vectors for targeted drug delivery to specific sites. This approach has been
extensively explored in the context of cancer therapies, which require high concentrations
of cytotoxic reagents specifically at the tumor.
Different techniques have been used to load MSC with the desired reagent. In one
approach, MSC were incubated with drug-loaded microparticles, which induced their
uptake of the microparticles and subsequently their release of the drugs into extracellular
space(72). Other studies have focused on genetic approaches, e.g. tumor necrosis factorrelated apoptosis-inducing ligand (TRAIL)-expressing MSC were found to localize to
tumors and reduce tumor growth(73, 74).
Importantly, such techniques should not affect the migratory properties of MSC. Again,
a better understanding of the migratory mechanisms of MSC after systemic infusion will be very
helpful to determine which MSC migratory properties need to be preserved.
19
1.2.3.3
Tissue engineering
The differentiation potential and vascular stabilization properties of MSC are also being
exploited in tissue engineering strategies.
In one approach, MSC can be implanted in scaffolds prior to implantation. For example,
MSC in a scaffold were implanted in a porcine model of mandibular distraction
osteogenesis. Sites implanted with scaffolds and MSC were found to have greater mineral
deposition and more adavanced gap obliteration that those implanted with scaffolds
alone(75). Another study that took advantage of the vascular stabilization properties of
MSC, found that transplantation of collagen gels implanted with both EC and MSC
were able to form functional and long lasting vasculature in vivo(25). This approach
depends on endogenous signaling after scaffold transplantation, with the option of
scaffold-derived signaling (e.g. absorption of proteins onto scaffold surface), to direct the
differentiation of exogenous MSC implanted in the scaffolds.
The second approach is more relevant to MSC trafficking. Here, scaffolds are implanted
without MSC, but with factors designed to recruit endogenous MSC to the scaffold. In
one study, scaffolds releasing stromal derived factor-i (SDF-1) was found to recruit
MSC from its surroundings in vitro, and induce their penetration into the pores of the
scaffold(76). Similar approaches have been designed with other chemoattractants,
including hepatocyte growth factor (HGF)(77) and platelet-derived growth factor
(PDGF)(78), though no studies to our knowledge have shown recruitment of
endogenous MSC in vivo. A better understanding of the mechanisms that mobilize and
recruit MSC will be essential for the successful design of such scaffolds.
1.3 CELLULAR TRAFFICKING
Cellular trafficking can be understood as the migration of a cell population from one point to a
distant site in the body. The blood and lymphatics connect distant tissues, and thus typically act
as conduits in the body for this migration. (An exception is the brain, which has an adapted
lymphatic system called the glymphatics, which, similar to the lymphatics, clears waste
metabolites from the brain and spinal cord(79, 80). It is unclear if cells can employ glymphatics
for migration.) The factors determining this journey can be classified into three groups:
I.
II.
III.
Factors influencing the cell's exit from its starting point into the blood or lymphatics
Factors influencing the cell's availability en route to the target site through the blood or
lymphatics
Factors influencing the cell's entry to the target site from the blood or lymphatics
There are many endogenous cell types, which engage in cell trafficking. Most hematopoietic
cells, which comprise the bulk of the cellular component of blood and lymphatics, traffic
extensively around the body. Leukocytes are a large class of hematopoietic cells with immune
20
function. Leukocytes comprise polymorphonuclear cells (neutrophils, eosinophils, basophils),
monocytes, macrophages B cells, T cells, dendritic cells and NK cells. In the blood, the most
abundant leukocyte is the neutrophil(8 1).The path that leukocytes travel throughout the body is
unique under physiological conditions, and can be even more complex in pathological contexts.
Under physiological conditions, common tissues which leukocytes target or exit from are the
bone marrow, lymph nodes, liver, spleen.
Mesenchymal cells, which include MSC, are also migratory cells, though they are less commonly
found in the blood or lymphatics. Indeed, one distinguishing characteristic of mesenchymal cells
are their migratory abilities(2). The term 'mesenchyme' derives from Greek, and refers to the
ability of mesodermal/ mesenchymal cells to migrate between the ectodermal and endodermal
layers during embryonic development. Cancer cells are also thought to undergo "epithelialmesenchymal transition", which is characterized by enhanced migratory capacity and
invasiveness compared to the epithelial layer from which it originated(82). Cancer metastasis is a
process influenced greatly by factors influencing cellular trafficking. These factors will be
discussed here, with a focus on mechanisms that MSC might employ when trafficking through
the blood.
1.3.1
Factors influencing the cell's exit from its starting point into the blood or lymphatics
The exit of cells from specific tissue sites is precisely controlled by multiple factors. For
instance, under physiological conditions, neutrophils are produced in the bone marrow
by HSC, and exit from the bone marrow to circulate with a half life of 6-8 hours, before
homing to the bone marrow or liver where they are thought to be destroyed(8 1). Their
exit from the bone marrow is thought to be largely influenced by the local gradients of
stromal derived factor-1 (SDF-1), a chemokine(81). Neutrophils express the G proteincoupled receptor for SDF-1, CXCR4, and are retained in the bone marrow by their
interactions with SDF-1 produced by bone marrow stromal cells(83, 84). Apart from
chemokines, integrins have also been thought to be important for the retention of
neutrophils in the bone marrow(85). Specifically, SDF-1 can enhance neutrophil
adhesion to VCAM-1, which is expressed on sinusoidal endothelium and large
interdigitating cells in the bone marrow. Neutrophils express the VCAM-1 ligand, VLA4, and were released into circulation only when both VCAM-1 and CXCR4 were
blocked, but not either one alone(85).
It is currently controversial if endogenous bone marrow-resident MSC can be mobilized
into the circulation. Most MSC therapeutic strategies thus employ the use of exogenous
culture-expanded MSC, which are systemically infused directly into circulation. Hence,
this thesis focuses on the use of exogenous, culture-expanded MSC, bypassing the step of
egress into the circulation from their tissue of residence.
21
1.3.2
Factors influencing the cell's availability en route to the target site through the blood or
lymphatics
Margination is a process that sequesters cells intravascularly in certain tissues.
Neutrophils are known to marginate in liver, spleen, bone marrow and lungs - 49% and
51% of intravascular neutrophils are circulating and marginated, respectively, under
physiological conditions(86). Although the mechanisms of this sequestration is not
completely understood, it has been shown that adrenaline can increase the circulating
pool of neutrophils(8 1).
The margination of MSC in the circulation is not well understood, though it is well
accepted that most systemically infused MSC are trapped in pulmonary capillaries
immediately following infusion, and are slowly released into the circulation over
time(57). Pretreating MSC with a blocking antibody to the a4 integrin reduced their
duration of sequestration in the lung(87). Hence, MSC margination may be a
combination of both mechanical trapping and adhesion.
Survival of circulating cells is another factor that can determine the number of cells that
ultimately arrive at the target site. This is particularly pertinent for metastasis, which is a
highly inefficient process. Although large numbers of cancer cells are shed into the
bloodstream, few ultimately arrive at the target site(88). Indeed, for most adherent cells,
the loss of adhesion with extracellular matrix or other cells results in apoptosis, through a
process termed 'anoikis'. Cancer cells can avoid anoikis through several mechanisms(89).
For instance, cancer cells can express proteins which make them resistant to anoikis, e.g.
TrKB(89). Other alternative mechanisms include entosis, in which a live cell can invade
another live cell. Though most cells that engage in entosis are ultimately degraded in
lysosomes, some cells remain viable and are eventually released(90). Yet another reason
that most cancer cells do not survive the circulation is due to intravascular lysis by NK
cells. However, some cancer cells are shielded from such lysis by inducing platelet
aggregation on their surface, apparently preventing them from being 'seen' by NK
cells(91, 92). Finally, cancer cells that arrest in capillaries might also rupture due to the
pressure differential across the cell(88).
The survival of systemically infused MSC in the circulation is unknown, as is their
interactions with other circulating cells, e.g. platelets and NK cells. Only two studies to
date have implicated platelets in MSC trafficking. However, neither studied the effect of
platelets on MSC survival, but only on overall MSC accumulation at sites of
inflammation(93, 94).
1.3.3
Factors influencing the cell's entry to the target site from the blood or lymphatics
1.3.3.1
Endothelial factors
Endothelial cells comprise the innermost lining of blood and lymphatic vessels, and act
as a major barrier that cells must traverse to enter their target site.
22
Despite the wide array of leukocyte types and functions, a well-established multi-step
leukocyte homing cascade has been developed. This cascade describes leukocyte
interaction with the endothelial lining of vessels within the tissue they are trafficking to.
The cascade can be roughly split into two categories: (i) The arrest of the cells on the
endothelial lining (comprising tethering, rolling and firm adhesion), and (ii) the passage
of the cells through the endothelial lining (comprising crawling and transmigration).
Before further elaboration into each step of the multi-step leukocyte homing cascade, it is
timely to briefly overview endothelial heterogeneity. The endothelial lining of blood and
lymphatics have some key differences, such as the nature of the intercellular endothelial
junctions, but even within blood vessels, distinctions are plentiful. These distinctions are
essential to understand in the context of cellular trafficking, as the endothelium is the
primary interface between the target site and circulating cells. Hence, endothelium
functions as a major signaling beacon to recruit cells from the circulation.
Blood leaves the heart through the arteries, which branch into arterioles then capillary
beds, the smallest vessels of the body (typically <10tm in diameter). The capillaries then
merge into venules and re-enter the heart through the veins. The arteries carry the most
oxygenated blood while the veins carry the most deoxygenated blood, though this is
reversed in the lungs.
Leukocyte homing occurs preferentially in post-capillary venules, the venules
immediately following the capillaries. The post-capillary venules have three
characteristics that seem to favor leukocyte homing:
A. Greater adhesion molecule expression. Specific adhesion molecule expression on
endothelial surfaces act as "molecular zipcodes" that recruit certain subsets of
circulating cells with complementary adhesion molecule expression. Post capillary
venules of 20-30ptm in the mesentery were found to have the highest expression
of adhesion molecule ICAM-1(95), while capillaries and arterioles seemed to
have minimal expression, consistent with other studies that found leukocytes to
6
mainly adhere in mesenteric venules of 25-30ptm(9 ).
B. Lower shear forces. The lower shear forces in venules, compared to arterioles,
may partially account for increased leukocyte homing in venules by providing less
resistance to the formation of strong adhesive bonds between leukocytes and
endothelium(97). Indeed, the number of adherent leukocytes recruited into
venules by an inflammatory stimulus is inversely proportional to the wall shear
rate(98, 99). It should be noted, however, that decreasing shear flow in arterioles
alone cannot recapitulate the leukocyte adhesion seen in venules(100), leading to
conclusions that shear flow may only facilitate leukocyte adhesion and
transmigration, which are largely mediated by adhesion molecule expression.
C. Greater permeability. Post capillary venules are also characterized by hyperpermeability, apparently generated by the formation of intercellular endothelial
23
gaps in response to pro-inflammatory mediators(101, 102). This may facilitate
leukocyte extravasation across endothelium, which often occurs through gaps
between endothelial cells. (103)
Although this characterization of post capillary venules holds true in most cases,
differences in microvasculature across different organs is not uncommon. For example,
capillaries in the lung(104) and liver(95) have been found to have high expression of
ICAM-1, which also correlates with greater leukocyte adhesion in the capillaries of those
organs(105). Further, there are three different types of capillaries with different
endothelial phenotypes and junctions (Table 1.1), which can affect physiological
permeability of the tissue. For more details on endothelial heterogeneity, the reader is
referred to several excellent reviews(106-109).
The multi-step leukocyte cascade was mostly elucidated based on studies in vessels of the
mesentery or cremaster muscles, due to the ease of imaging in those anatomic locations.
However, the cascade may deviate in some organs, partly due to the heterogeneity of
endothelium as discussed(107-109). Although the actual homing process for each type of
leukocyte is unique and can deviate somewhat for this standard model of homing, the
cascade is broadly conserved in most situations, and forms the basis for comparison
between cell types and vascular environments.
The steps of the leukocyte homing cascade comprise:
A. Tethering and rolling. Here, leukocytes interact with endothelium via selectins,
glycoproteins expressed on the cell surface. These selectins have fast bond
association and dissociation kinetics, allowing them to effectively roll on the
endothelial surface( 110). Important selectins for rolling include P-selectin
(expressed by endothelium and platelets), L-selectin (expressed by all circulating
leukocytes) and E-selectin (expressed by endothelium) (111). Because P-selectin is
stored in endothelial vesicles known as Weibel-Palade bodies under baseline
conditions, endothelium can express P-selectin on their surface soon after onset
of inflammation. On the other hand, E-selectin must be transcribed and
translated de novo after onset of inflammation, hence it is expressed later in
inflammation compared to P-selectin(1 11).
B. Adhesion. The preceding event of rolling allows leukocytes to come into contact
with endothelium, where they may bind to chemokines expressed on the
endothelial surface through chemokine receptors. These chemokine receptors are
G-protein coupled receptors that span the membrane seven times. Chemokine
signaling can cause integrin activation of the leukocyte, which significantly
increases the adhesiveness of the integrin through a change in protein
conformation over a few minutes. Activated integrins on the leukocyte can then
bind to the complementary proteins on the endothelium, mediating firm
adhesion on the endothelium( 111). Important integrins for adhesion include
ICAM-1 and VCAM-1, which belong to the immunoglobulin superfamily of
molecules and are all upregulated on endothelium during inflammation.
24
Table 1.1 Features of the three types of capillaries
Types of Capillaries, Physiologic(106)
Continuous
Fenestrated
Discontinuous,
sinusoidal
Caveolae
+
+
Vesiculovacuolar
organelles (VVOs)
+
-
Intercellular gaps
-
-
+
Fenestrations and
-
+
+
Muscle, lung,
skin, brain
Kidney
glomeruli, GI
Liver, bone
marrow sinus
+
diaphragms
Anatomic sites
25
C. Crawling. After arrest, leukocytes flatten and polarize on the endothelium, in
which lamellipodia form at their leading edge. This is followed by crawling, a
process also known as 'lateral migration' or 'locomotion'. Crawling, which is
mediated by integrins, helps leukocytes to find sites permissible for
transmigration(112, 113). For example, leukocytes have been observed to crawl
to the nearest endothelial junction where they can initiate transmigration in
vitro(112). Leukocytes that cannot carry out crawling have delayed
transmigration despite being able to adhere and polarize.
D. Transmigration. Leukocytes can subsequently transmigrate via two potential
routes - paracellular (through endothelial junctions) or transcellular (through an
individual endothelial cell). Though the paracellular route is better recognized,
recent reviews have highlighted the relevance of the transcellular route in
vivo(1 14-116). The choice of route that a leukocyte takes seems to be dependent
on ease of paracellular gap versus transcellular pore formation under the
circumstances(1 16), i.e. the leukocyte seems to take 'the path of least
resistance(1 17)'. This is inferred from studies that find that, unlike most settings,
transcellular transmigration seems to be the dominant route of transmigration
across the blood-brain-barrier (BBB). Since the endothelial junctions in the BBB
are uniquely well-organized( 118), the transcellular route may provide an
alternative path for leukocytes to avoid traversing endothelial junctions.
Based on this multi-step cascade, the adhesion molecule expression of MSC and ability
to perform various steps of the cascade has been investigated. This is reviewed in the
Chapter 2. Further, the ability of MSC to transmigrate across endothelium is explored in
depth in Chapter 3.
1.3.3.2
Non-endothelial factors
In addition to primary interactions with endothelium, secondary interactions between
platelets and circulating cells have also been implicated in facilitating trafficking.
Firstly, platelets can adhere directly to endothelium or exposed subendothelial matrix
during inflammation. Leukocyte and cancer cells can either form aggregates with
platelets in the circulation that subsequently adhere to the vessel wall, or directly adhere
to platelets that have already arrested on the vessel wall( 119). Indeed, circulating
neutrophil-platelet complexes were found to be required for neutrophil activation and
subsequent migration in both models of peritonitis and lung infection(120). Further,
circulating platelet-monocyte aggregates are increased under inflammatory conditions
e.g. acute coronary syndrome(121, 122), and can promote the progression of
inflammatory disease(123). Hence, heterotypic interations between circulating cells often
exist during inflammation and can influence cellular trafficking.
Secondly, platelets have been shown to release microparticles in vivo. These
microparticles can coat the surfaces of circulating cell types and effectively transfer
26
platelet-endothelial adhesion molecules, thus promoting the recruitment of circulating
cells to a target site(124).
Thirdly, platelet adhesion to neutrophils can result in the intravascular formation of
neutrophil extracellular traps (NETs) neutrophil that can trap other circulating cells at
the site of inflammation(125-127). During certain types of inflammation and immune
reactions, neutrophils have been shown to extrude their nuclear DNA into the
extracellular environment forming an adhesive meshwork of material, a process termed
'NETosis'(128, 129). NETs consist of filaments approximately 17nm in diameter(130),
and studded with neutrophil granular proteins(131). In some studies, NETs formed
intravascularly in liver sinusoids in models of sepsis. There NETs were able to trap
bacteria and circulating tumor cells(126, 132). Hence, NETs may act as a site of
adhesion for certain circulating cells.
Finally, passive mechanical trapping of cells in small diameter vessels has been postulated
to mediate cellular entrapment in tissues, especially for larger cells like cancer cells and
MSC(133, 134).
MSC trafficking has largely focused on MSC-endothelial interactions, and neglected the
role of secondary interactions with other circulating cells and mechanical trapping. We
explore the role of these non-endothelial factors in Chapter 4.
1.4 THESIS OUTLINE
The three following chapters contain the bulk of the work that forms this thesis. Chapter 2
represents a broad and comprehensive review of our understanding of MSC trafficking, and
seeks to delineate the key questions pertinent to the field. Chapter 3 focuses on a specific step in
the migration of MSC to sites of inflammation - the transmigration of MSC across
endothelium. Chapter 4 moves beyond MSC-endothelial interactions, to determine the role of
non-endothelial factors in MSC trafficking in vivo.
The last chapter comprises a conclusion, reflecting on the implications of the findings for future
work.
27
CHAPTER TWO
A COMPREHENSIVE REVIEW OF MESENCHYMAL STEM CELL TRAFFICKING
2.1 PREFACE
The following chapter was adapted with permission from the publication:
Karp, J. and Teo, G., Mesenchymal Stem Cell Homing: The Devil is in the Details. Cell Stem Cell,
2009. 4(3): p. 206-216.
The purpose of this review was to provide a critical analysis of the methods developed to track
the homing of exogenously infused MSCs. Pertinent considerations that were emphasized
included: (i) how MSCs are cultured, (ii) methods used to deliver MSCs, (iii) potential
mechanisms for MSC engraftment, (iv) methods used to quantify MSC homing, and (v)
methods used to characterize the MSCs following a homing event. We also discussed strategies
that have been employed to enhance trafficking of MSCs to particular tissues, and the hurdles
hindering their translation to the clinical setting.
2.2 INTRODUCTION
Mesenchymal stem cells (MSCs), also referred to as connective tissue progenitor cells or
multipotent mesenchymal stromal cells (3), have demonstrated significant potential for clinical
use. This capacity is due to their convenient isolation, lack of significant immunogenicity
permitting allogenic transplantation without immunosuppressive drugs, lack of ethical
controversy, and their potential to differentiate into tissue specific cell types (135, 136) with
trophic activity (137), to promote vascularization (138), and to promote potent
immunosuppressive effects (reviewed elsewhere (139)). Thus, MSCs have been the focus of a
regime of emerging therapeutics to regenerate damaged tissue and treat inflammation resulting
from cardiovascular disease and myocardial infarction (MI), brain and spinal cord injury,
cartilage and bone injury, crohn's disease, and graft versus host disease (GVHD) during bone
marrow transplantation (140). Although local transplantation or injection of MSCs represents a
potential approach that may be useful in certain settings (141, 142), the potential for minimally
invasive delivery of MSCs via systemic infusion is of particular interest (34, 143, 144). However,
a significant barrier to the effective implementation of MSC therapy is the inability to target
these cells to tissues of interest with high efficiency and engraftment.
28
The study of MSC homing following mobilization of host MSCs, or following systemic infusion
of exogenous MSCs is extremely complex. The challenges facing these efforts are due to a
number of factors including the lack of universally accepted criteria for defining the MSC
phenotype and their functional properties, by the rare presence of MSCs within blood, and by
the diverse methods used to culture MSCs and study their homing potential. Critical questions
pertinent to all studies in the MSC trafficking field include: (i) Can host MSCs be mobilized
into peripheral blood? (ii) Can exogenously delivered MSCs home to ischemic tissues or sites of
inflammation from peripheral blood and what is the efficiency of this process? And (iii), can host
MSCs be mobilized into peripheral blood and then target ischemic tissues? The different routes
for MSC trafficking represented in these questions are illustrated in Figure 2.1. The third
question is the most technically difficult to address and hence, least discussed in the current
literature. The first question has already been reviewed elsewhere(106), and thus will only be
briefly discussed.
This review will focus on providing a critical analysis of the methods developed to track the
homing of exogenously infused MSCs. Pertinent considerations that will be emphasized include:
(i) how MSCs are cultured, (ii) methods used to deliver MSCs, (iii) potential mechanisms for
MSC engraftment, (iv) methods used to quantify MSC homing, and (v) methods used to
characterize the MSCs following a homing event. We will also discuss strategies that have been
employed to enhance trafficking of MSCs to particular tissues, and the hurdles hindering their
translation to the clinical setting.
2.2.1
Definition of MSCs and MSC Homing
MSCs may be defined as multipotent cells capable of self-renewal that can give rise to a
number of unique, differentiated mesenchymal cell types(18). Despite this definition,
many researchers use different methods to culture MSCs, assess their differentiation
potential, and evaluate their capacity for self-renewal. Although MSCs may be derived
from multiple tissues, it is critical to consider that significant phenotypic differences in
MSCs exist which may reflect distinct functional properties (4), and this heterogeneity
may be a function of their tissue microenvironment (6). Also, it is critical to consider
that MSCs exhibit a striking similarity to vascular mural cells called pericytes that are
embedded within the vascular basement membrane of microvessels and capillaries
throughout the body (18, 20).
29
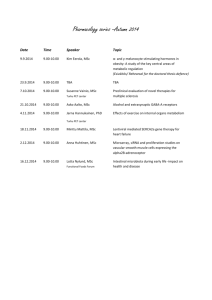
Figure 2.1 The active MSC homing circuit. MSCs play several roles (red text within pink boxes) depending
on their anatomic location. Studies have shown their presence in both peripheral blood and healthy tissues
and organs (listed in grey), in addition to the bone marrow where they have historically been isolated from.
Numerous active homing routes exist for MSCs (arrows). Red arrows represent paths which have been
substantiated by published studies. Sites of inflammation include acute inflammation due to injury, chronic
inflammation (e.g. GvHD), and tumors.
30
Given the lack of universally accepted criteria for defining a MSC, the Mesenchymal and
Tissue Stem Cell Committee of the International Society for Cellular Therapy (ISCT)
proposed a set of standards to define human MSC for both laboratory-based scientific
investigations and for pre-clinical studies(3). As part of the minimal criteria, human
MSCs must adhere to tissue culture plastic, be positive for CD105, CD73, and CD90
and negative for CD45, CD34, CD14 or CD1Ib, CD79a, or CD 19, and HLA-DR, and
must be able to differentiate to osteoblasts, adipocytes and chondroblasts under standard
in vitro differentiating conditions. Given the heterogeneity of typical MSC culture
procedures and a lack of enforcement of the above mentioned characterization criteria,
definitive conclusions based on the literature are often difficult to surmise.
MSC homing is defined as the arrest of MSCs within the vasculature of a tissue followed
by transmigration across the endothelium. Such a non-mechanistic definition is
appropriate given the current absence of a definitive MSC homing mechanism, unlike
the well characterized leukocyte adhesion cascade that defines leukocyte homing. The
lack of data describing the exact positioning of the MSCs following infusion makes it
difficult to determine if the cells have arrested within the vessels (localization) or have
undergone transendothelial migration (homing).
2.3 CAN MSCs BE MOBILIZED INTO PERIPHERAL BLOOD?
The potential for MSC trafficking under physiological steady state conditions is contentious,
with reports in the literature of diametrically opposed findings. Studies that support the presence
of MSCs within blood have reported only minute quantities of circulating MSCs(145), whereas
several studies report the inability to locate any circulating MSCs at all (reviewed
elsewhere(146)). The failure to harvest sufficient numbers of circulating MSCs at steady state
conditions is complicated by the need to access blood via venapuncture, which in theory could
release small quantities of pericytes or other connective tissue cells into the circulation.
Interestingly, Mereilles et al. was consistently unable to derive a long-term culture of MSCs from
portal vein accessed blood, a technique which reduced the possibility of pericyte or other
connective tissue cell contamination of the blood sample(147). However, the success of isolating
MSCs is also likely dependent on the methods of mobilizing MSCs into peripheral blood,
eliminating contaminating cells, and methods of culturing the isolated MSCs. It is important to
note that MSCs isolated from peripheral blood have shown heterogeneous marker expression.
Specifically, an early study isolated adherent, fibroblast-like stem cells with osteogenic and
adipogenic potential from the blood of 4 mammalian species including human, which were
distinguished from BM-derived human MSCs by the absence of Stro-1 and endoglin(145).
Other studies report the isolation of MSCs from peripheral blood using pre-selection methods
for CD133+ cells in G-CSF mobilized peripheral blood(148). These cells have potential to
differentiate into adipocytes, osteoblasts, chondrocytes, and neuronal/glial cells(149).
Of particular significance, increased numbers of MSCs have been isolated from peripheral blood
cells of injured mice (to induce intimal hyperplasia) compared to non-injured controls(150).
This trend correlated with significant increases in peripheral blood concentrations of the
31
cytokines VEGF and G-CSF. Moreover, MSCs from injured animals were cultured up to 10
passages and had tri-lineage differentiation potential in vitro, compared to MSCs from noninjured animals which could only be passaged twice. These results need to be repeated by several
groups before a central dogma - that the presence of circulating MSCs occurs only in response to
injury - can be developed.
2.4 FACTORS INFLUENCING THE DISTRIBUTION OF EXOGENOUSLY DELIVERED
MSCs
2.4.1
Culturing of MSCs
There are several factors regarding the MSC culture conditions that should be reported
for homing experiments as the culture condition may have a significant impact on MSC
function. For example, the confluency of MSCs cultured under laboratory conditions
before being infused can affect their migration potential. Increased culture confluence
was shown to inhibit transendothelial migration in MSCs by increasing the production
of a natural matrix metalloproteinase (MMP) inhibitor, TIMP-3(151) . The passage
number of MSCs used is also important as MSCs have been shown to gain or lose certain
surface receptors during culture which might influence their homing capability. Freshly
isolated MSCs have been shown to display enhanced homing ability compared to their
culture-expanded counterparts(152). Homing receptors, such as CXCR4, a chemotactic
receptor for SDF-1 which is upregulated in the bone marrow and in ischemic tissues, is
usually absent on the surface of culture-expanded MSCs(140, 144, 153, 154). However,
treating MSCs with a cocktail of cytokines in culture has been shown to induce high
surface expression of CXCR4 that enhanced homing ability(155). Given that the
expression of CXCR4 and other homing receptors are typically observed on a subset of
MSCs and often lost with culture expansion, it is plausible that these may be naturally
present on endogenous MSCs, but lost after culture(154). Interestingly, simulating
ischemic environments in culture, which some believe is representative of the MSC
niche, may also increase MSC motility. Hypoxic preconditioning increased MSC
migration through Matrigel by upregulating MMPs(156) and on tissue culture
plastic(157) compared to MSCs maintained in normoxic environments. In addition to
the passage number, confluency of the passaged cells, site of isolation, and properties of
the media and incubation environment, it is critical to consider the heterogeneity in
MSC surface receptor expression and resulting MSC behavior that has been observed
both within and between studies (147, 154, 158-160). Such variability of MSC
properties emphasizes the importance of comprehensive characterization of MSCs within
each study. It is especially important to have an accurate assessment of MSC properties
prior to injection or implantation of MSCs into the highly complex and varying
microenvironments that exist within the body.
32
2.4.2
Delivery of MSCs
For MSC trafficking experiments, the timing of delivery, number of cells delivered, and
site of MSC infusion may impact the engraftment efficiency and the destination of
exogenously delivered cells. Both higher numbers of infused MSCs and early delivery of
MSCs following an event causing ischemia (e.g. MCAO) have been shown to improve
engraftment rates( 161). MSCs were found to engraft in the myocardium at higher rates 1
day after MI as compared to 14 days after MI, suggesting that MSCs engraft specifically
in response to acute MI. (162) Although it may be expected that higher infused numbers
of MSCs should result in higher numbers of engrafted MSCs, and better functional
outcomes, there may be a plateau beyond which additional delivered cells may not
improve the outcome. For example, in a rat model of brain injury, although neurological
function after the systemic infusion of MSCs was improved for a dose of 1x106 cells, no
additional enhancement was observed when 3 X 106 MSCs were infused(163). Studies
that have attempted to optimize the protocol for MSC delivery in terms of numbers and
timing found that higher numbers of MSCs and MSCs delivered sooner after
presentation of ischemia resulted in higher engraftment rates, though differences in the
extent of functional outcome were not apparent (164).
The site of MSC delivery may impact the route MSCs travel to reach the target organ.
Systemic administration can be achieved by intravenous (IV) injection, intraperitoneal
(IP) injection, intraarterial (IA) injection or intracardiac (IC) injection. IV delivery is the
least invasive, however, IC and IA delivery have led to higher engraftment rates than IV
delivery in certain models of myocardial infarction (MI)(165, 166). IA injection close to
the target site (extracranial right internal carotid artery) in a model of brain injury was
shown by MRI imaging of radio-labelled cells to significantly enhance homing to the
brain versus distant IV injection (femoral vein)(167). IA injection may reduce
accumulation of MSCs within filtering organs such as the lung, liver, or spleen that is
often observed following IV delivery(144, 166, 168), however, IA may also lead to
increased probability of microvascular occlusions(167) which is termed 'passive
entrapment'. Since IC and IA delivery bypasses the initial uptake by the lungs, more
MSCs are available to engraft at the ischemic site. IP delivery is rarely used, but has been
employed to deliver MSCs to murine foetuses, in a mouse model of muscular dystrophy,
since IV delivery was deemed inappropriate for this application(169). Following birth,
the donor cells were found in both muscle and non-muscle organs. It is unknown why
IV delivery resulted in the consistent death of the foetuses. A final method of delivery is
local infusion, which entails injecting MSCs directly into the tissue of interest. DiI
labelled MSCs intravenously transfused into baboons were undetectable in limb muscles
compared to detection of DiO labeled MSCs following direct injection into the
muscle(170). However, local infusion is likely not clinically feasible in many cases due to
its potentially high degree of invasiveness (e.g. into the heart or brain), and locally
administered cells often die before significantly contributing to the healing response due
to diffusion limitations of nutrients and oxygen(171).
33
2.5 ANALYZING MSC ENGRAFTMENT
2.5.1
EFFICACY
It is presumed that therapeutic efficacy of infused MSCs relies on extravasation and
engraftment of systemically infused MSCs where they may exhibit local trophic or
paracrine activity, or, where MSCs may inhabit a tissue and release paracrine factors into
the vasculature for a systemic effect. However, few studies have provided insight into the
mechanisms of homing. Specifically, it is unclear if the MSCs actively home to tissues
using leukocyte-like cell adhesion and transmigration mechanisms (reviewed
elsewhere(172)), or become passively entrapped in small diameter blood vessels. Instead
of selectin and integrin-mediated cell arrest on inflamed endothelium(172), it is possible
that MSCs become passively arrested in capillaries or microvessels including arterioles
and post-capillary venules (144, 167) (refer to Figure 2.2). Passive entrapment is likely a
function of the cell's size and overall deformability. The mode of arrest is thus of
particular importance for MSCs since they are known to enlarge during in vitro cell
culture (173). Expansion of cell numbers in culture is a necessary step during MSC
therapy, however this practice may elevate the risk of entrapment of cells within nonspecific tissues including the lung (144, 166). Geometrical and mechanical entrapment
of cells has been previously described after systemic injection of MSCs (144, 166) and
after injection of endothelial progenitor cells into the tumor microvasculature (174).
Passive arrest may be distinguished from active arrest by the observation of an altered
blood flow (i.e. through blocking a vessel)(167). Cells that home via leukocyte adhesion
mechanisms quickly flatten and spread on the underlying vascular endothelium in
preparation for transmigration (175), which reduces the possibility for altered blood
flow. Understanding the mechanisms of passive and active arrest will likely be essential
for developing more effective MSC delivery strategies.
34
A Deceleration
Tethering
...........
ii. Rolling
P-selectin
VLA-4/VCAM-1
I
B Arrest
Wi. Firm Adhesion
-
?ICAM-1
VLANC~A-4/CAM-I
w
C Extravasation
iv. Transmigration
VLA-4/VCAM-1
MMPs, TIMPs
1~
Capillaries
'go
Post-Capillary Venules
Figure 2.2 Model for passive versus active homing. (A) There are two potential mechanisms for how MScs
may decelerate within the vasculature during the homing process. The large size of MSCs and/or narrower
capillaries may reduce the cell velocity due to physical interactions leading to passive entrapment (top cell).
Alternatively, MSCs which deform, likely pass through capillaries to post-capillary venules similar to
leukocyte homing (176) can (i) tether and (ii) roll on activated vasculature at sites of inflammation, where a
chemokine gradient (red gradient) is established. (B) During passive arrest, an altered blood flow (arrows)
may be observed. In contrast, during active arrest, cells quickly flatten and spread on the underlying
endothelium, and blood flow is virtually unchanged. Although ICAM-1 expression on ECs has been
implicated in active arrest of MSCs, it is not known which ligands present on MSCs interact with this
receptor. (C) After active arrest, MSCs may transmigrate, but the fate of passively arrested MSCs is unclear.
The molecular interactions that regulate MSC homing are listed in green. A third possibility for MSC
engraftment within inflammatory tissues (not illustrated) involves passive arrest within the vasculature
proximal to the site of inflammation, followed by transmigration in response to a chemokine gradient in the
surrounding tissue. It is also possible that the physical properties of culture-expanded MSCs (i.e., increased
size) reduces the cell velocity enough within post capillary venues to permit engagement of firm adhesion
receptors (negating the need for rolling receptors), thus leading to a proposed mechanism that incorporates
both aspects of active and passive homing.
35
2.5.1.1
Local Irradiation Enhances Engraftment Efficacy
There is substantial evidence that infused MSCs have higher engraftment efficiencies
within sites of inflammation or injury. An interesting study by Francois et. al. examined
this through subjecting mice to total body irradiation (TBI), and in some cases in
combination with additional local irradiation within the abdominal area or hind
leg(177). The engraftment of systemically infused MSCs was measured 15 days later, and
engraftment levels were found to be higher in mice subjected to TBI compared to
nonirradiated mice. TBI induced a 2.8-fold increase on engraftment levels of MSCs in
the brain, 3-fold in the heart, 2.5-fold in the liver, 2.6-fold in BM, and 1.7-fold in
muscles, while levels of engraftment in the lung were not affected. This pattern suggests
that MSCs engrafted in response to radiation damage except in the lung, in which
engraftment rates remained the same with or without radiation. Presumably, this lack of
change is because their presence in the lung resulted from a passive process. However, we
cannot discount the possibility that in addition to integrin upregulation, especially that
of VCAM-1(178), irradiation or the induction of MI also leads to local changes in
microvessel diameter (i.e. constriction)(179, 180), affecting passive arrest and thus
explaining the accumulation of MSCs in inflamed tissue.
2.5.1.2
Methods Used to Probe the Active Arrest of MSCs
The most significant evidence for active arrest of MSCs within inflamed tissues is
supported by methodology involving integrin blocking(181) and knockout studies(153)
that show a dependence on selectin and integrin interactions. For example, Ip et al.
showed that blocking the PJ1 integrin on MSCs, a component of the adhesion molecule
VLA-4 that governs the arrest of leukocytes on activated endothelium, reduced their
engraftment in ischemic myocardium(181). Furthermore, using P-selectin knockout
mice, Ruster et al. showed via intravital microscopy that fewer MSCs slowed down in
post-capillary venules compared to wild type mice(153). These results suggest that the
engraftment of MSCs within target tissues depends on specific molecular interactions
prior to the transmigration step, rather than a non-specific passive steric phenomena.
These molecular interactions can readily be studied in vitro via standard leukocyte
adhesion assays.
To date only one study has examined MSC rolling on endothelial cells in vitro. Ruster et
al. showed that MSCs bind to endothelial cells in a P-selectin dependent manner and
that rolling MSCs interact with VLA-4/VCAM-1 that promotes firm adhesion on the
endothelial cells(153). However, the rolling velocities reported were -100-500 pm/s at
shear stresses of 0.1-1.0 dynes/cm 2. To provide context, leukocyte rolling has been
typically observed to be less than 5 pm/s at shear stresses up to 4 dynes/cm 2 (172, 182).
The observation of high rolling velocities of MSCs is likely explained by the lack of in
vitro activation (e.g., by TNF-a) required to mimic endothelium within inflamed or
injured tissues, which promotes the expression of cell adhesion receptors that regulate cell
rolling and firm adhesion. Also, it is important to note that interacting leukocytes are
36
typically defined by velocities lower than 50% of the free stream velocity(183). However,
this study used a more generous criterion; namely, cells traveling at less than the free
stream velocity were considered to be rolling. Although velocities of MSCs traveling on
activated endothelium were not reported, experiments that examined retention of firmly
adherent MSCs under shear showed a significant increase in the number of MSCs that
remained adhered to endothelial cells after activation with TNF-M at shear stresses
between 0.1-2.0 dynes/cm 2 . Nevertheless, given the generous criteria for an interacting
cell, the implications of this study into the mechanisms of MSC homing are limited.
Clearly, studies that examine MSCs rolling on activated endothelium, at velocities and
shear rates which are physiologically relevant are essential to further elucidate potential
MSC homing mechanisms. A study by Segers et. al. examined the firm adhesion of MSC
under static and various shear stress conditions on activated endothelium (184). Similar
to the study by Ruster et. al., this study highlighted the dominant role of VLA-4 and
VCAM-1 as effectors of firm adhesion. Interestingly, firm adhesion receptor/ligand
interactions including the VLA-4/VCAM-1 axis mediates rolling due to changes in their
tertiary conformations (185-187). Similar studies to elucidate the actual mechanisms of
MSC arrest on vasculature demands attention in the field of MSC trafficking.
2.5.1.3
Methods Used to Probe the Transmigration of MSCs
Very few studies have examined the transmigration of MSC. Steingen reported that
MSCs can transmigrate through non-activated endothelial monolayers via VCAM1 /VLA-4 interactions, but rather than undergoing complete diapedesis as is observed for
leukocytes, MSCs tended to integrate with the endothelial layer, perhaps as embedded
pericytes(188). The time course for transmigration was long compared to leukocytes
which take 5-20min (172) - specifically, the endothelial monolayer resealed over the
integrated MSCs after 240min, leaving the MSCs beneath the monolayer. This deviance
from previously studied leukocyte transmigratory behavior might have resulted from the
use of non-activated endothelium, rather than a physiologic inability of MSCs to
transmigrate. Lymphocytes for example exhibit significantly reduced transmigratory
activity on non-activated endothelium due to the absence of pertinent cell surface
adhesion molecules. Such subtleties are important to consider when interpreting and
comparing results between studies. Results thus far suggest that specific MSCendothelium interactions regulate transmigration, although further studies are required
to examine this phenomenon under conditions that mimic an active inflammatory state.
2.5.1.4
Methods Used to Promote Chemotaxis of Systemically Infused MSCs
In addition to adhesive interactions that mediate MSC homing to specific sites,
chemokines released from tissue or endothelial cells may promote activation of adhesion
ligands, transendothelial migration, chemotaxis and/or subsequent retention in
surrounding tissue(189-191). For example, systemically infused GFP labeled MSCs that
express the MCP-1 receptor CCR2 on their surface were infused into transgenic mice
with MCP-1 specifically expressed in the myocardium. MCP-1 is typically expressed at
37
sites of inflammation, and thus represents a model homing chemokine (Belema-Bedada
et al., 2008). GFP-positive cells were found in the myocardium at high frequencies of 20
cells/microscopic field compared to none in the hearts of control mice 7 and 14 days
later. These frequencies were also 20 times higher than those for GFP-positive cells
found in skeletal muscle, brain and kidney as detected by immunofluorescence, and -8
times higher as detected by RT-PCR analysis of whole organs for eGFP mRNA.
Unfortunately, the number of MSCs found in the lung were not reported, a likely
destination for infused MSCs (168). It possible that indirect effects, rather than the
interaction of MSCs with MCP-1 via the CCR2 receptor was responsible for difference
in the distribution. For example, MCP-1 is known to upregulate adhesion molecules on
the endothelial surface and increase endothelial permeability(192). Hence, MSCs were
transfected with a vector expressing a truncated version of FROUNT (DN-Frount).
FROUNT binds to CCR2, enabling CCR2-mediated chemotaxis towards MCP-1, but
not HGF, SDF-1 or VEGF. DN-Frount competes with endogenous FROUNT for
CCR2-binding and acts as a dominant negative effector of CCR2-mediated chemotaxis.
DN-Frount-transfected MSCs lacked the capability to home to the hearts of the MCP-1
transgenic mice compared with non-transfected MSCs. Hence, the direct interaction of
CCR2 with MCP-1 was crucial to the engraftment of MSCs in ischemic heart tissue in
this model. In a similar study, systemically administered MSCs detected in the
myocardium doubled after the expression of another inflammatory chemokine, MCP-3
(a ligand for CCR2 and CCR1), was induced in the myocardium compared to nontransfected controls(162). This study, unlike Belema-Bededa et al., did not present
evidence that the response was directly due to the interactions between CCR2 or CCR1
and MCP-3.
2.5.1.5
Methods Used to Assess the Role of Enzymes in MSC Homing
In addition to chemokines and adhesion molecules, invasive cells often secrete enzymes
which are essential for their migratory activity. MSCs secrete proteases which regulate
transmigration, invasion of the basement membrane of endothelium and degrade
extracellular matrix during chemotaxis. Both blocking antibodies toward MMP2, and
SiRNA knock-down of MMP2 in MSCs reduce transendothelial migration in
vitro(151). The role of MMP2, as well as MT1-MMP and TIMP-2, in MSC invasion
was further confirmed by Ries et al. who also showed that chemotactic invasion of MSCs
through human extracellular matrix (ECM)-coated transwell chambers could be
hindered by inhibition of the proteases(193). Down-regulation of MMP-2, MT1-MMP,
and TIMP-2 via RNAi significantly impaired the migration of MSCs by 72%, 75%, and
65%, respectively, when compared with control cells that had received a non-targetdirected siRNA. Steingen et al. also perfused MSCs through isolated mouse hearts, and
detected the presence of gelatinases at sites of MSC invasion through in situ
zymography(1 88). Thus MSCs possess the ability to breakdown endothelial basement
membrane, and migrate towards chemotactic factors.
38
The substantial migratory properties of systemically infused MSCs was also
demonstrated in a recent study using a rat model of middle cerebral artery occlusion
(MCAO) Specifically, Feridex-labeled human MSCs were directly infused into either the
ipsilateral or contralateral hemisphere of the injured brain(194) and imaged via MRI
once a week up to 10 weeks. Regardless of the site of infusion, MSCs were found to
migrate and localize in both the boundary and core of the infarcted tissue. This result
was confirmed by Prussian blue staining and immunohistochemistry using a human
nuclei-specific antibody, in which cells positive for both stains were exclusively found in
the infarcted region. The time series imaging which showed the gradual movement of the
MSCs towards the site of inflammation, in the case of contralateral infusion, supports
the notion that MSCs possess extensive migratory capabilities within a tissue. Such
capabilities are likely a function of their responsiveness to chemotactic factors and
production of ECM-degrading enzymes.
2.5.2
EFFICIENCY
Although it has been well established that systemically infused MSCs localize within
injured, inflamed, and cancerous tissues, their efficiency of homing as a function of local
tissue properties is unclear and the method of detection, method of quantification, and
timing of quantification can significantly impact the result. MSCs are often detected in
vivo using radioactive labelling(165, 166, 168, 195), fluorescent labelling(196),
transduction of MSCs with reporter genes(166, 197), species mismatch (i.e. injection of
human MSCs into a rodent), and probing for sex mismatch (i.e. injection of female cells
into a male rodent) via specific genes by fluorescent in-situ hybridization(198, 199) or
real time polymerase chain reaction (RT-PCR) (189, 200). These tracking and assessment
methods have been used for models such as acute myocardial infarction, cerebral
intimal
fibrosis(201),
pulmonary
stroke( 161),
brain injury(163),
ischemic
hyperplasia(150) and chronic graft rejection(202) and are described in Table 2.1. The
different sensitivities between methods may account for some of the variability that is
often observed(168, 203).
The quantification of homing efficiency within a target tissue is typically assessed by one
of two techniques: (1) Quantification of the relative level of radioactivity in excised
tissues and organs(166), or (2) averaging the number of fluorescently labelled cells
present in a fixed number of microscopic fields per tissue sample(166, 196, 198). Of
particular interest is the capability for real-time in vivo tracking of MSCs rolling along
the vascular endothelium(153) and diapedesis of MSCs through the endothelium within
specific tissues(1 4 4 ). The available methods for assessing MSC trafficking have shown
that systemically infused MSCs can (i) preferentially target, with limited efficiency,
inflammation, sites of injury, tumors, as well as specific tissues such as the bone
marrow(144, 189, 197), and (ii) non-specifically distribute throughout various tissues
and organs(204) including the lung, liver, kidney and spleen where a high percentage of
infused cells are often observed(166, 168). However, the methods used to assess MSC
homing efficiency arc often relative, comparing between the densities of engrafted MSCs
39
in experimental and control groups versus quantifying the total number of MSCs which
have homed to a particular tissue. Furthermore, no robust positive controls for high
homing efficiencies exist. Emerging techniques for tracking MSCs which include labeling
with super paramagnetic iron oxide nanoparticles(205, 206) or quantum dots(207) may
enhance the assessment of MSC homing, although the utility of these techniques requires
further analysis.
40
Table 2.1 MSC homing efficiencies after systemic delivery
Animal
model
I
2
Dog (2530kg); acute
MI
Pig; acute
Site of
infusion
Limited
details
provided
Target site
Anterior apex
of heart
Time/Method of
detection
Day 1/
SPECT/CT
imaging
Homing efficiency to
target site1
4.1% (normalized to
number of cells that
targeted the lung on Day
1)
Day 2
4.6%
Ear vein
Heart
Week 2/
MSCs cultured
with iridium, and
hearts assayed for
iridium content
0%
MI
3
Rat; acute
MI
Left
jugular
vein
Heart
24 hours/
MSCs labeled
with PKH-26
3%
4
Female rat;
acute MI
Tail vein
Heart
Day 3/
FISH probing for
Y chromosome
gene
Week 1
0.0006%
Week 4
0.0012%
Week 8
0.0012%
Week 4/
MSCs labeled
with DAPI
For untreated MSCs,
0.0005% (percentage of
total cells infused, per
microscopic field)
5
Rat; acute
MI
Tail vein
Heart
Other key results
Reference
Detection of MSCs was only possible via
SPECT/CT Imaging
Number of engrafted MSCs was below
detection threshold of MRI.
(168)
Functional improvement not evaluated
IC and endocardial administration resulted
in 2.9 and 1.4 x 10A6 cells (out of total 40
million infused) in the infarcted zone
respectively
Functional improvement not evaluated
MSCs in the heart were concentrated in
ischemia border zone at Week 4
Functional improvement observed.
Functional improvement observed
(165)
(27)
(208)
0.0012%
IGF- 12 treatment of MSCs increased
CXCR4 surface expression in a dose- and
time-dependent manner
Functional improvement observed
For treated MSCs,
0.002% (percentage of
total cells infused, per
microscopic field)
(209)
6
7
Mouse; acute
MI
Rat;
traumatic
brain injury
Femoral
vein
Tail vein
Heart
Brain
4 hours/
Gamma camera
imaging on
""'Tc-labelled
cells
<1%
3 months/
Staining with
antihuman nuclei
antibody
For 2 or 8 million MSCs
Lungs showed greatest engraftment
compared to heart, liver, kidneys, bladder
(166)
Lung engraftment reduced in IC injection
route.
IC infusion resulted in 4.5 fold increase in
MSC heart engraftment
infused, 00025%
(percentage of total cells
infused, per mm 2 of tissue
section)
Functional improvement not evaluated
Homing efficiency depended on the number
of MSCs infused
(210)
Functional improvement observed
For 4 million MSCs
infused, 0.00045%
(percentage of total cells
2
infused, per mm of tissue
8
9
Rat; cerebral
ischemic
stroke
Rat; cerebral
ischemic
stroke
Limited
details
Tail vein
Brain
(penumbra
lesion)
Brain
Day 7/
MSCs transduced
with LacZ+ and
stained for 3galactosidase
Day 14/
Measurement of
Brd-U reactive
cells
section)
0.0042% (percentage of
total MSCs infused, per
mm 2 of tissue section)
(211)
Functional improvement observed
For
1 million MSCs
infused, 0.75%
For 3 million MSCs
infused 24h after MCAO 2,
1.1%
Day 35
No MSCs detected in undamaged brain
hemisphere
For 3 million MSCs
infused 7 days after
MCAO 2, 0.52%
42
Homing efficiency depended on the number
of MSCs infused, and the time after
induction of injury
Functional improvement observed
(161)
10
Mouse;
Kaposi's
Tail vein
Tumor
Sarcoma
tumors
11
Female
mouse;
pulmonary
Jugular
vein
Lung
fibrosis
Day 3/
MRI on
superparamagneti
c iron oxide
particle-labeled
MSCs
Day 7
0.0012%
(percentage of total MSCs
infused, per microscopic
field)
Day 14/
FISH probing for
Y chromosome
gene
5.1 8 xO4% of total lung
epithelial type II lung cells
DNA
Less bleomycin-induced inflammation and
collagen deposition was observed after MSC
infusion compared with controls
Day 14/
MSCs transduced
with LacZ+ and
stained for 1galactosidase
8-10% of fibroblastoid
cells isolated from heart
allografts
Most engrafted MSCs had a fibroblast-like
morphology
Day 17/
RT-PCR
detecting eGRP
transgene in
eGFP-transduced
MSCs
For BM aspirate, 0 eGFP*
cells (per 0 pg of input
PCR DNA)
(exposure to
bleomycin)
12
Rat; chronic
rejection of
heart
Limited
details
provided
Heart
allografts
allografts
13
Baboon;
Lethal total-
body
irradiation
(1000 Gy
over 4 days)
Jugular
and
femoral
veins
BM
(posterior iliac
crest or
proximal
humerus)
(212)
Most engrafted MSCs had an epithelial-like
morphology
(201)
0.00043%
DNA,
or 1.37x10-% of the total
(202)
Graft survival time was shortened after MSC
infusion
MSCs were able to home to the BM
irrespective of conditioning or
immunohistocompatibility.
Both autologous and allogeneic MSCs were
able to engraft for more than a year in the
BM.
Day 30
Day 511
Antitumorigenic effects of hMSCs through
inactivation of Akt protein kinase,
dependent on cell-cell contact and presence
of E-cadherin
For BM biopsy, 5271
eGFP* cells
For BM biopsy, 29 eGFP*
cells
43
(197)
Baboon
Day 14
For BM aspirate, 144.2
eGFP' cells
For BM biopsy,
0 eGFP* cells
Day 377
For BM biopsy,
377 eGFP* cells
Day 442
For BM biopsy,
0 eGFP* cells
14
15
16
Mouse
Mouse
Mouse
Mouse;
Sublethally
Tail vein
Tail vein
Tail vein
BM (dorsal
skull)
BM
BM (based on
a total BM
volume 16
times that of
one femur)
1 hour/
Intravital
confocal
microscopy of
MSCs labeled
with Vybrant
DiD
Week 4/
RT-PCR
Day 1/ CFU-F
assay for eGFPMSCs
For unmodified MSCs,
0.0067% (percentage of
total MSCs infused, per zstack image)
For sugar-modified MSCs
(HCELL+), 0.067%
(percentage of total MSCs
infused, per z-stack image)
For unmodified MSCs,
2.5% (percentage of cells
which were donor-derived)
For modified MSCs,
22.5% (percentage of cells
which were donor-derived)
For primary MSCs, 4.3%
For primary MSCs,
41-53%
irradiated (3
or 7 Gy)
For culture-expanded
MSCs, none detected
44
MSCs with a modified surface glycan with
E-selectin binding capabilities, HCELL2 ,
homed to the BM and formed rare foci of
osteoid.
(144)
The a4 subunit of VLA-4 was upregulated
in MSCs via adenoviral transduction,
increasing BM engraftment, and decreasing
lung engraftment.
(200)
Culture-expanded MSCs had a diminished
ability to home to the bone marrow
compared to primary MSCs.
(213)
17
18
Rat
Femoral
vein
Mouse;
Osteogenesis
imperfecta
Intraperito
neal
injection
Bones (Tibiae
and femurs;
no
differentiation
between
native bone
and bone
marrow)
Long bone
(without BM)
BM
1Unless
2
48 hours/ MRI
imaging on 1".In
oxine-labeled
MSCs
2.5 months/
FISH assay for Y
chromosome
Without co-injection of
vasodilator, 0.5%
With co-injection of
vasodilator, 1.2%
The co-injection of vasodilator increased
bone marrow and liver engraftment, and
decreased lung engraftment.
(195)
A decrease in lung, but increase in liver
engraftment was observed at 48 hours,
compared to immediately after infusion.
7% (percentage of cells
which were donor-derived)
(199)
5% (percentage of cells
which were donor-derived)
otherwise mentioned, homing efficiency is based on a percentage of the total cells infused
IGF-1, insulin growth factor-1; MCAO, middle cerebral artery occlusion; HCELL, hematopoeitic cell E-selectin/L-selectin ligand.
45
............
2.5.2.1
Methods for Imaging the Precise Location of MSCs as a Function of Time
It is important to consider that systemically infused MSCs may redistribute after their
initial localization in tissues. Using SPECT/CT imaging, Kraitchman et. al. showed that
the initial concentration of MSCs in the lung post-transfusion decreased after 24h, with
a simultaneous increase in MSCs found in the infarcted heart tissue(168). Gao et al. also
found that MSCs gradually moved from the lung to the liver, spleen, kidney and bone
marrow(214). This observation suggests that the amount of time between transfusion
and detection must be considered when interpreting such studies, as the relative
distribution among tissues and organs will vary depending on when the detection takes
place. Also, at earlier time points (e.g. less than 24h), it becomes especially important to
distinguish the local position of MSCs within the tissues with respect to blood vessels.
Presumably, MSCs which remain inside the vasculature of the tissue in which they are
detected cannot be assumed to have engrafted until they have extravasated through the
vessel wall. It is critical to know if MSCs are transiently residing within vessels in the
tissue, passively entrapped in vasculature(174), or have extravasated. Discriminating
between these options requires high resolution imaging with relevant staining for blood
vessels and specific tissue structures as is performed in Charles Lin's laboratory(144).
One must also be cautious and consider the possibility that the localization of observed
donor MSCs may be due to fusion with endogenous cells(215).
2.5.3
Characterization of MSC post-delivery
Characterization of engrafted MSCs following systemic infusions is a big unmet need in
the field of MSC trafficking. Achieving progress in this area would be useful to
determine if these exogenous MSCs can form an 'MSC niche' following engraftment. It
is important to consider that data generated during the 80s showed engraftment of donor
stromal cells following human bone marrow transplantation(216), but was later
refuted(217). More recently, within a clinical setting, using sex-mismatched bone
marrow T-cell-depleted allografts, a limited reconstitution of marrow mesenchymal cells
was demonstrated. Specifically, stromal layers containing donor-type cells were observed
in 14 out of 41 patients in one study(218) and 4 out of 14 patients in another
study(219). (For more detailed examination of MSC engraftment following bone
marrow transplantation, please see(152, 220, 221)). In another study of significant
interest, MSCs from eGFP transgenic mice were isolated from the BM, expanded in
vitro, and systemically infused into wild type mice (189). eGFP positive cells were
isolated from the BMs of the wild type mice 3 and 6 months later, expanded, and reinfused into an additional, secondary recipient. Again, eGFP positive cells could be
isolated from the BM of this third mouse and expanded, albeit at lower numbers.
Unfortunately, one limitation of the study was the lack of thorough characterization of
the MSCs after each isolation. Ideally, labelled cells should have been isolated from the
bone marrow after infusion, cultured and characterized as suggested by the ISCT(222).
The stemness of the isolated MSCs was confirmed by only assaying their ability to
express myocyte markers in response to appropriate inductive cues. Therefore, it remains
open to question whether the isolated cells were indeed MSCs or differentiated progeny,
and thus it is critical that future experiments include thorough characterization of the
MSC phenotype.
Given the lack of sufficient characterization methods of systemically infused MSCs
following engraftment, it is unknown whether they engraft in their native state, or
differentiate to replenish the parenchymal and stromal cells at an ischemic site.
Delineation between MSCs and their differentiated progeny has been attempted by
assaying for markers unique to mature cell types that MSCs were expected to
differentiate into based on the tissue of interest(169, 202, 223). For example, infused
cells or their progeny have been found to express dystrophin in a muscular dystrophy
model(169), cytokeratin in a model of intestinal epithelium irradiation damage(223),
and osteocalcin in a model of MSC homing to healthy bone marrow(144). The current
challenges associated with characterization of MSCs following systemic infusion are a
consequence of the combined complexity of defining what is an MSC, with sensitive
means for detection and isolation of MSCs within an in vivo system.
2.6 ENGINEERING MESENCHYMAL STEM CELL TRAFFICKING
Methods of improving the trafficking and engraftment of MSCs and other cell types are a high
priority for cellular therapies. Although culture expanded MSCs express certain cell surface
receptors that mediate aspects of homing including VLA-4 (153) and certain chemokine
receptors (191), they do not express PSGL-1(144) and have low expression levels of other
pertinent adhesion and chemokine receptors (e.g. CXCR4) which typically governs tethering and
rolling of circulating cells on activated vascular endothelium.
Retrovirus vectors encoding homing receptors such as CXCR4 have been recently used to
enhance homing and engraftment of HSCs and MSCs through increasing cell invasion in
response to SDF-1, the ligand for CXCR4 which is typically present at inflammatory sites (224226). In one example, genetically modified MSCs over-expressing CXCR4 on their surface
homed to ischemic myocardium following systemic administration and enhanced postmyocardial infarction recovery of left ventricular function in a rat model (226). In another study
the a4 subunit of the VLA-4 integrin was similarly upregulated on MSCs using an adenovirus
vector, found to successfully dimerize with Pf1 intergrin to form VLA-4, and increase the homing
of MSCs to the bone marrow by more than 10-fold as compared to non-transduced MSCs
(200). Interestingly, the engraftment of MSCs in the lung simultaneously decreased.
An alternative approach to gene therapy, which may present potential safety concerns, involves
chemical engineering of cell surface glycans to initiate cell rolling (144). A critical initial step in
the cascade of events during cell homing involves cell rolling, during which cells engage shearresistant, low-affinity interactions with vascular endothelial cells (227). Specifically, Sackstein
and colleagues enzymatically engineered an E-selectin binding motif that is responsible for
hematopoietic stem cell homing onto the surface of MSCs (144). Since E-selectin is highly
expressed in bone marrow, substantial bone marrow engraftment of systemically administered
47
MSCs was achieved along with rare foci of osteoid juxtaposed to the endosteal surface. A similar
approach has been applied to improve engraftment of cord blood derived HSCs (228). However,
these methods require complex sugar chemistry and the scope of potential alterations is limited
to modification of existing cell surface ligands. Another approach that could be applied to MSCs
involves the conjugation of antibodies to the cell surface via bispecific antibodies (229) or
palmitated protein G or protein A which permits cell surface functionalization by potentially any
antibody bearing an accessible Fc region (230). However, it is unclear how targeting based on
these firm adhesion approaches (i.e. with antibodies) would compare to approaches that promote
cell rolling at the target site.
We have recently demonstrated that a robust MSC rolling response can be induced on P-selectin
substrates in vitro by chemically attaching ligands to the surface of MSCs. The method, which
involves covalent attachment of biotin to the cell surface followed by streptavidin and a
biotinylated ligand can be used to attach potentially any adhesion ligand to the surface of any
cell type to enhance targeting to specific tissues following systemic infusion(231). In addition,
culture conditions may be used to stimulate the expression of certain homing receptors, such as
CXCR4 (173, 232). Taken together, these approaches provide significant potential for
enhancing the homing of MSCs to specific tissues.
2.7 SUMMARY AND PROSPECTIVE
There are several clinical trials being performed worldwide to examine the systemic
administration of MSCs to treat a variety of diseases and tissue defects. Despite the general
excitement about these trials and the promising results thus far, there is major lack of
understanding of how MSCs target specific tissues. This gap in our knowledge may be why
current clinical dosing includes high numbers of cells that may range from 150-300 million
MSCs administered twice per week over the course of two weeks (233). Furthermore, the
balance between the beneficial effects from locally engrafted MSCs versus systemic effects from
secreted paracrine factors that diffuse into target tissues is unclear. Typical problems faced by
those in the MSC trafficking field and recommended actions are discussed in Table 2.2.
Whether MSCs mobilize and home under steady state conditions remains a common topic of
debate. Progress in this area has been stifled by the difficulties in identifying and isolating native
MSCs; most studies utilize culture expanded MSCs that do not express many of cell adhesion or
chemokine receptors that are responsible for the homing of leukocytes and haematopoetic stem
cells. Furthermore, tracking of MSCs after local transplantation or systemic infusion has relied
on techniques that have inherent disadvantages including indirect methodology, significant
manipulation of the host biology (e.g. bone marrow reconstitution), or use of an exogenous
MSC source.
48
Table 2.2 Problems faced in the field of MSC trafficking
Based on the knowledge derived from existing studies, we can conclude:
A. There is mounting evidence that host MSCs appear to mobilize in response to
inflammation or injury and target specific tissues via active mechanisms; however more
work is required to substantiate this model, and the origin and mechanisms of trafficking
of the mobilized MSCs remains unresolved.
B. Systemically infused MSCs are frequently observed in significant concentrations within
the bone marrow compartment, or within an injury or inflammatory site and these cells
have potential to reduce inflammation and promote tissue regeneration. However, the
exact location of the MSCs (within the vessel or tissue) and their phenotype remain
elusive and thus broad conclusions cannot be substantiated regarding their engraftment
or mechanisms that mediate their functional properties.
C. Direct methods of assessing native MSCs and their trafficking properties is a big unmet
need required to conclusively elucidate mechanisms of MSC trafficking during
physiological and pathological states. Detection of infused MSCs that remain in an
undifferentiated state compared to their differentiated progeny also presents a significant
challenge.
D. Homing of culture expanded MSCs is inefficient compared to leukocytes and HSCs,
which apparently is due to a lack of relevant cell adhesion and chemokine receptors,
however, engineering strategies are available to enhance the homing response. The
increased size of MSCs likely promotes passive cell entrapment and reduces the number
of MSCs that reach the target site.
As our understanding of the mechanisms of MSC trafficking grows, the ability to enhance
homing to specific tissues through engineered approaches should significantly reduce the number
of cells required to achieve a therapeutic effect, and presumably provide better outcomes for
patients. Accumulating evidence suggests that MSCs have a significantly larger role in regulating
wound healing and inflammatory diseases than previously thought. Given the systemic nature of
many diseases and the desire to have minimally invasive therapies, systemic infusion of MSCs
that can promote tissue regeneration and immunosuppressive effects represents an attractive
therapeutic approach. The number of potential therapeutic applications and their efficiency and
efficacy will continue to grow as the fundamental biology that is responsible for the MSC
regenerative properties and homing responses continues to be elucidated.
so
CHAPTER THREE
A HIGH RESOLUTION MICROSCOPIC ANALYSIS OF MESENCHYMAL STEM CELL
TRANSMIGRATORY ABILITY IN VITRO
3.1 PREFACE
The following chapter was adapted with permission from the publication:
Teo, G., et al., Mesenchymal stem cells transmigratebetween and directly through tumor necrosis
factor-a-activatedendothelialcells via both leukocyte-like and novel mechanisms. Stem Cells, 2012.
30(11): p. 2472-2486.
In this study, we aimed to characterize the basic cellular processes mediating this extravasation
and compare them to those involved in leukocyte transmigration. Using high-resolution confocal
and dynamic microscopy, we showed that, like leukocytes, human bone marrow-derived MSC
preferentially adhere to and migrate across TNF-a-activated endothelium in a vascular cell
adhesion molecule-1 (VCAM-1) and G-protein coupled receptor (GPCR) signaling-dependent
manner. As several studies have suggested, we observed that a fraction of MSC integrated into
endothelium. In addition, we observed two modes of transmigration not previously observed for
MSC: Para (between endothelial cells)- and trans (directly through individual endothelial cells)cellular diapedesis through discrete pores and gaps in the endothelial monolayer, in association
with VCAM- 1-enriched 'transmigratory cups'. Contrasting leukocytes, MSC transmigration was
not preceded by significant lateral migration and occurred on the time scale of hours rather than
minutes. Interestingly, rather than lamellipodia and invadosomes, MSC exhibited non-apoptotic
membrane blebbing activity, that was similar to activities previously described for metastatic
tumor and embryonic germ cells. Our studies suggest that low avidity binding between
endothelium and MSC may grant a permissive environment for MSC blebbing. MSC blebbing
was associated with early stages of transmigration, in which blebs could exert forces on
underlying endothelial cells indicating potential functioning in breaching the endothelium.
Collectively, our data suggested that MSC transmigrate actively into inflamed tissues via both
leukocyte-like and novel mechanisms.
3.2 INTRODUCTION
More than 100 clinical trials currently evaluate adult 'mesenchymal stem cells' (MSC) or
'multipotent stromal cells' for treatment of diverse inflammatory, cardiovascular and
autoimmune diseases (234). Approximately half of the clinical trials involve the systemic infusion
51
of MSC into the vascular circulation (234). Preclinical animal studies demonstrate that infused
MSC preferentially engraft into inflamed or ischemic tissues, a behavior that is thought to be
critical for their therapeutic efficacy (235). Additionally, physiological homing ability of
endogenous MSC is supported by studies reporting that endogenous MSC can be mobilized
from the bone marrow and recruited into wounds (196), tumors (38), ectopic endometrial tissue
in endometriosis (236, 237) and sites of intimal hyperplasia (34). A critical step in such
recruitment and engraftment is the exit of MSC from the vascular circulation (i.e.,
extravasation), which requires crossing the endothelial cell barrier that lines blood vessels. For
MSC, this process of extravasation remains incompletely understood.
In contrast, the process of leukocyte extravasation at sites of inflammation has been wellcharacterized as a dynamic and rapid (timescale of minutes) multi-step cascade (Fig. 6). During
inflammation, endothelium becomes activated by cytokines such as tumor necrosis factor-alpha
(TNF-0). They then upregulate chemoattractants and surface proteins, including selectins and
cell adhesion molecules (CAMs), which mediate rolling and adhesive interactions respectively.
Subsequently, leukocytes initiate a phase of lateral migration over the luminal surface and utilize
dynamic cytosketelal protrusions (e.g., lamellipodia, pseudopods and invadosomes) to cross the
endothelium through discrete gaps in intercellular junctions (i.e., 'paracellular diapedesis') or
directly through pores in individual endothelial cells (i.e., 'transcellular diapedesis') (114, 172,
238). In parallel, endothelium proactively generates its own actin-dependent protrusions (i.e.
'transmigratory cups') that embrace the leukocytes and guide their transmigration (238).
Like leukocytes, previous studies suggest that MSC may also be able to undergo selectinmediated rolling (153) and integrin-mediated adhesion (153, 184) preferentially on cytokineactivated endothelium. However, unlike leukocytes, a limited number of studies attempting to
investigate the cellular process of MSC transmigration have largely suggested an 'integration'based mode of transmigration. MSC integration has been described as the process in which
gross-scale retraction of endothelial cells allow for MSC spreading and incorporation into the
endothelial monolayer, before the endothelial monolayer ultimately reforms over the integrated
MSC (94, 239, 240). However, the molecular and cellular details of this process have not been
well resolved. For example, critical aspects such as detailed three-dimensional cellular
architecture, distribution of adhesion and endothelial junction molecules and dynamics have not
yet been carefully investigated.
We therefore employed high-resolution confocal and dynamic live-cell imaging in the current
study and found strikingly that, in addition to integration, MSC can transmigrate through
discrete pores and gaps in the endothelium by paracellular and transcellular diapedesis, in
association with endothelial transmigratory cups similarly to leukocytes. However, contrasting
leukocytes, MSC transmigration does not involve significant lateral migration, lamellipodia or
invadosomes in the initiation of transmigration. Instead, like some embryonic germ and
metastatic tumor cells (241-243), MSC exhibit non-apoptotic blebbing which can exert forces
on endothelial cells during early stages of transmigration.
52
3.3 METHODS
3.3.1
Antibodies and Reagents
The following antibodies and were used for immunocytochemistry: IC1/12-Cy3 and
IC1/13-Cy3 were as described (244). ToPro3, Phalloidin-546 and 647, Cholera toxin B488 and 546 were from Invitrogen. Purified mouse anti-human CD90 (clone 5E10),
FITC mouse anti-human CD90 (clone 5E10) and mouse anti-human CD144 (VEcadherin; clone 55-7H1) were from BD Pharmingen (San Diego, CA, USA). Polyclonal
sheep anti-human VCAM-1 and Rabbit anti-human JAM-1 was from R&D Systems
(Minneapolis, MN, USA). Purified goat anti-rat VE-Cadherin (sc-6458) and mouse
anti-rat ICAM-1 (clone 1A29) were from Santa Cruz (Santa Cruz, CA, USA) and
(Raleigh, NC, USA), respectively. Rabbit polyclonal anti-human occludin was from
Abcam (Cambridge, MA, USA). Mouse anti-human P-catenin conjugated to Alexa Fluor
647 was from Cell Signaling Technology. Annexin V conjugated to Alexa Fluor 647 was
from Molecular Probes (Eugene, OR, USA). Antibody conjugation to Alexa488,
Alexa546 or Alexa647 bisfunctional dyes (Molecular Probes) was performed according to
manufacturer's instructions. The fluorescent lipophilic dyes, DiI and DiO were from
Invitrogen and used according to the manufacturer's instructions. The following
antibodies were used for function blocking experiments: Polyclonal sheep anti-human
VCAM-1 (R&D Systems), mouse anti-human alpha 4 integrin (HP2/1 Millipore), sheep
IgG isotype control (Jackson Labs) and mouse IgG1 isotype control (BD). The following
antibodies were used for flow cytometry analysis of MVECs or GPNTs: AlexaFluor488conjugated mouse anti-human CD54 (clone RR1/1) (generous gift from Timothy
Springer), FITC-conjugated mouse IgG1 isotype control (clone P3.6.2.8.1, eBioscience,
San Diego, CA, USA), PE-conjugated mouse anti-human CD106 (clone 51-10C9, BD),
PE-conjugated mouse IgG1 isotype control (BD), mouse anti-rat CD54 (clone IA29,
AbD Serotec), mouse anti-rat (CD10 , clone 5F10), rat IgG2A isotype control (clone
eBR2a, eBioScience), and FITC-conjugated goat anti-mouse secondary antibody
(Invitrogen). The following antibodies were used for flow cytometry analysis of MSCs
and CD4+ T cells: Mouse anti-human alpha 4 integrin (HP2/1, Millipore),
AlexaFluor488-conjugated mouse anti-human alpha 4 integrin (7.2R, R&D Systems),
mouse anti-human alpha 5 integrin (MAB1956Z, Chemicon), mouse anti-human beta 1
integrin (P4C10, Milllipore), mouse anti-human beta 2 integrin (TS1/18, gift from
Professor Timothy Springer), and murine IgGI isotype control (ICIGG1, Abcam).
3.3.2
MSC Culture
Primary human MSC were obtained isolated from the iliac crest of the hip bone of
healthy consenting donors and obtained from the Texas A&M Health Science Center,
College of Medicine, Institute for Regenerative Medicine at Scott & White Hospital
(Temple, TX, USA).. The donor inclusion criteria were that they must be normal,
healthy adults, at least 18 yrs of age, with a normal Body Mass Index and free of
infectious diseases (as determined by the blood sample screening performed one week
before bone marrow donation). In these studies MSC from four different donors were
used. MSC were maintained in a-Minimum Expansion Media (a-MEM; Invitrogen,
Carlsbad, CA, USA) supplemented with 15% Fetal Bovine Serum (Atlanta Biologicals,
Lawrenceville, GA, USA), 1%
L-Glutamine (Invitrogen), and 1%
Penn-Strep
(Invitrogen). Cells were cultured to 80% confluence before passaging. All experiments
were performed using MSC at passage 3-7 during which they expressed high levels of the
MSC markers CD90 and CD29 (>99% cells) and did not express hematopoietic markers
CD34 or CD45 (0% of cells), as determined by flow cytometry analysis (245). MSC
senescence at P3, P5 and P7 was assessed using the Senescence P-Galactosidase Staining
Kit from Cell Signaling Technology (Danvers, MA, USA), according to manufacturer's
instructions. In some cases, MSC were pretreated with 2.5 PM etoposide for 24 hours
followed by drug washout and an additional 72 h of culture in complete media to induce
apoptosis. Stained MSC were imaged using a Nikon TE2000E inverted microscope
equipped with a 20x bright-field objective, CCD camera and NIS Element software
(Melville, NY, USA). Five microscopic fields of view (each containing at least 50 MSC in
total) were captured and the percentage of total MSC in each field that were senescent
(i.e., showed blue colored P-Galactosidase reaction product) was calculated and averaged
among the five fields for each condition.
3.3.3
EC Culture
Primary adult human lung (hLMVEC) and cardiac (hCMVEC) microvascular
endothelial cells were purchased from Lonza and cultured on human purified fibronectin
(Invitrogen)-coated substrates in EBM-2 MV media (Lonza) and used at passage 4-6.
Five mg of fibronectin/cm2 was used for coating substrates. The immortalized Lewis rat
brain microvascular endothelial cell line GPNT was obtained from Dr. John Greenwood
(University College of London, UK), characterized as described (246, 247) and cultured
on collagen-IV-coated substrates (7 pg of collagen/cm2) in media comprised of a 1:1
ratio of F 10 (Invitrogen) and a-MEM (Invitrogen) supplemented with 10% Fetal Bovine
Serum and 1% Penn-Step. Aortic adventitial fibroblasts were obtained from Lonza, and
cultured in Dulbecco's Modified Eagle's medium (Invitrogen), supplemented with 10%
Fetal Bovine Serum and 1% Penn-Strep. Fibroblasts were used at passage 4-6.
3.3.4
Flow Cytometry
MSC and EC cultures were detached with 0.05% Trypsin-EDTA (Sigma) and
suspended in FACS buffer (phosphate buffered saline (PBS) containing 2% fetal calf
serum, 2 mM EDTA and 0.03% azide) and then incubated with primary antibodies (10
mg/ml) at 4oc for 30 min. Samples were washed three times with PBS, incubated
secondary antibodies, the re-washed and analyzed using a C6 Flow Cytometer (BD
Accuri, Ann Arbor, MI, USA) and CFlow software. EC were either resting or activated
by pretreatment with recombinant TNF-a (50 ng/ml for 16 h; Peprotech, Rocky Hill,
NJ, USA or Invitrogen) and/or IFN-y (100 ng/ml for 48 h; Invitrogen). For apoptosis
studies, MSC, EC or co-incubated MSC and EC were detached from tissue culture
54
plates with 0.05% Trypsin/EDTA and stained with Annexin V, and propidium iodide
(PI) using the Annexin V/Dead Cell Apoptosis Kit (Invitrogen) according to
manufacturer's instructions and then analyzed by flow cytometry. In cases, of MSC-EC
co-incubation, co-incubation time was 1 h and co-staining with CD90-647 was used to
distinguish MSC from EC. As indicated in some cases MSC were pretreated with 100
ng/ml pertussis toxin (PTX) or 1 mM hydrogen peroxide (H202) for 2 h.
3.3.5
Fixed-End Point Microscopic Analysis of MSC Adhesion and Transmigration
EC were plated at 90% confluency in 24-well plates (100,000 cells per 24 well)
containing circular coverglass (12 mm diameter) coated with fibronectin (5 ptg/cm 2 ; or
for GPNTs, collagen IV at 7 ptg/cm 2 ). These were cultured for 48-72 h and, as indicated,
and pre-activated for 16 h with TNF-a (50 ng/ml; Peprotech, Rocky Hill, NJ, USA or
Invitrogen) or for 48 h with IFN-y (100 ng/ml; Invitrogen). Cultured MSC were
detached using 0.05% Trypsin/EDTA (Invitrogen), resuspended in EBM-2 MV media,
added to the EC monolayers, and incubated at 37"C and 5% CO 2 for indicated and then
fixed with 3.7% formaldehyde. In some cases EC and/or MSC were pre-labeled with
membrane dyes DiI and DiO (1 pig/ml) respectively for 30 min at 37 0C, prior to coincubation. As indicated in some cases EC were pre-incubated with function with
blocking anti-VCAM-1 antibody (20 pg/ml; R&D Systems) for 30 min at 37 0C and
MSC were treated with PTX (100 ng/ml; Sigma-Aldrich) for 2 h at 37 0C.
In the case of pre-labeled (i.e., with DiI and DiO samples), imaging was performed
directly. For all other experiments (except anti-occludin staining), fixed samples were
blocked with 5% non-fat dry milk in phosphate buffered saline (PBS; Invitrogen) for 5
min, variously stained for CD90 (anti-human CD90-488, -546), GM1 gangliosides (an
alternate MSC marker; CTx-B-488, 546), VCAM-1 (polyclonal anti-VCAM-1-Cy3),
ICAM-1 (ICAM-1-Cy5), F-actin (phalloidin-647), nucleus (ToPro3), VE-cadherin
(anti-human-VE-cadherin-Cy5; anti-rat-VE-cadherin-488) and JAM-1 (anti-humanJAM-1-Cy3) in blocking buffer containing 0.05% Triton-X100 for 30min, and then
washed 3 times. Anti-occludin staining was performed as previously described (248, 249).
Confocal imaging was conducted on a Zeiss LSM 510 (Zeiss, Heidelberg, Germany)
using a 63x water immersion objective. For serial Z-stacks, the section thickness ranged
from 0.5 to 1.0 pim. Three-dimensional reconstruction and projection of Z-stacks was
performed with Axiovision software (Zeiss, Heidelberg, Germany). The stages of MSC
transmigration were determined from the relative distribution of VCAM-1 or ICAM-1
(used as surface marker for ECs), CD90 or CTx-B (used as surface markers for MSC)
and actin (to determine structure of both cells) fluorescence in both the x-y and z
dimensions using confocal microscopy as described (244). Five distinct stages in MSC
transmigration were defined and interpreted: 1) MSC adherence to the apical surface of
endothelium, 2) endothelial cup formation, 3) endothelial gap/pore formation (initiation
of transmigration), 4) subendothelial spreading of the MSC (advanced progression of
transmigration) and 5) barrier restoration (MSC is completely on the basal endothelial
surface). For some analyses these stages were collapsed into 3 major positions of MSC
55
relative to EC: Apical (Stages 1-2; MSC is completely on the apical side of the EC
monolayer); Transmigrating (Stages 3-4; MSC is spans across a gap or pore in
endothelial layer with portions remaining both apical and basal); Basal (Stage 5). Two
routes of transmigration (paracellular and transcellular) were defined as described(244)
using the relative distribution of VE-Cadherin (an endothelial adherens junction marker),
CD90 and VCAM-1. In paracellular transmigration, MSC migrated between two or
more endothelial cells with evident disruption of the VE-Cadherin stained adherens
junctions (i.e., 'paracellular gaps'). In transcellular transmigration, MSC migrated
directly through an individual endothelial cell via a transcellular pore located at least 1
pm from an intact adherens junction. MSC were scored as positive for membrane
blebbing activity if at least one clear membrane bleb was present. Blebs were defined as
hemispherical-shaped cell surface protrusions (seen through CD90 staining) of 1-5 pm in
diameter. Filopodia were defined as thin spike or rod-like cell surface protrusions.
3.3.6
Fluorescence Plate Reader-Based Adhesion Assay
Adhesion assay was as previously described(250). Briefly, confluent hCMVEC
monolayers were grown in 96-well plates and, where indicated, pre-activated with 50
ng/ml TNF-a for 16 h. hMSC were detached and incubated with a 0.5 pM solution of
2',7'-bis-(2-carboxyethyl)-5-(and-6)-carboxyfluorescein
(BCECF, Molecular Probes)
fluorescent dye for 15 min at room temperature in the dark in buffer A (Hanks Buffered
Salt Solution (HBSS, Invitrogen) supplemented with 20 mM HEPES (pH 7.2), 1%
human serum albumin). MSC were washed once with buffer A and resuspended at 2 x
105 cells/ml in EBM-2MV. 50 pl of MSC suspension was added to each well of
hCMVEC. In some cases MSC or EC were pre-incubated for 15 min with 20 pg/ml
mouse anti-alpha 4 integrin or sheep-anti-VCAM-1 function-blocking antibodies (or
correlating species-matched IgG controls), respectively, prior to MCS-EC co-incubation.
Plates were subjected to a brief centrifugation (<10 sec at 150 RCF) and then incubated
at 37"C for 10 min. The fluorescence of each well was read on a SpectraMax M5
microplate reader (Molecular Devices, Sunnyvale, CA, USA) both immediately before
and following two sequential washes with 100 pl of buffer A. Wells in which no MSC
were added were used to measure background fluorescence of the monolayer. Each
condition was done in triplicate. Results are presented as the post-wash fluorescence of
each well divided by the pre-wash fluorescence.
3.3.7
Live-Cell Imaging of MSC on Endothelium
ECs and MSC were transfected by Amaxa electroporation according to the
manufacturer's instructions (Lonza) with the following constructs as indicated: GFPactin (Clontech Laboratories, Mountain View, CA, USA), palmitoylated YFP ('memYFP'; Clontech) and palmitoylated DsRed ('mem-DsRed'; Clontech (244)). For MSC
nucleofection, 500,000 MSC were resuspended in 100 ml of Amaxa hMSC Nucleofector
solution. Next, 5 mg of the relevant plasmid (either mem-YFP or GFP-actin) was added
to the MSC suspension and then the mixture was transferred to an electroporation
56
cuvette, which was placed in the Amaxa electroporator and subject to the MSC-specific
electroporation program U-23. MSC culture media (500 ml) was then added to the
cuvette, the mixture and then transferred to a T75 flask containing 15 ml of MSC
culture media. Transfected MSC were incubated at 37'C/5% C02 for 24 h before use.
Survival rate was roughly 60% and transfection efficiency was -50%. For hLMVEC
nucleofection, 500,000 hLMVEC were resuspended in 100 ul of Amaxa hMVEC-L
Nucleofector solution. Cells were then transfected as above using the endothelial-specific
electroporation program S-005 followed by addition of EBM-2MV culture media and
plating on Delta T culture dishes from Bioptechs (Butler, PA, USA). Survival rate was
-50% and transfection efficiency was 40-60%. Transfected endothelial cells were used
48 h after plating and 12-16 h after activation with 50 ng/ml of TNF-a. Occasionally,
EC were alternatively stained with the fluorescent membrane marker Octadecyl
Rhodamine B Chlorideme (R18; Invitrogen) immediately before live-cell imaging. R18
was mixed with PBS at a 1:2000 ratio, and incubated with a confluent endothelial
monolayer in the dark at 37'C for 10 min, followed by washing twice with EBM-2MV.
Live-cell imaging was conducted on an Axiovert S200 epifluorescence microscope (Zeiss)
equipped with an Orca CCD camera (Hamamatsu, Japan) and Axiovision software
(Zeiss), both 40X and 63X oil-immersion objectives and a Delta T heating stage
(Bioptechs) to maintain temperature at 37"C. At intervals of 5-90 seconds, sequential
differential interference contrast (DIC), fluorescence, and interference reflection
microscopy (IRM; a modality that explicitly reports regions of close cell-substrate
interaction(251)) were acquired. Lateral migration velocities of apical MSC on
endothelium (28 MSC in four separate experiments) were obtained by tracking position
of individual MSC over a 30 minute duration using the AxioVision Tracking Module.
3.3.8
Live-Cell Imaging of MSC on Fibronectin-Coated Glass
To quantify MSC blebbing in the presence or absence of adhesive signals, we performed
live-cell imaging of MSC, with or without pre-incubation with the 120kDa achymotryptic cell attachment region of fibronectin (Millipore, Billerica, MA, USA), on
fibronectin-coated glass. Delta T culture dishes from Bioptechs were incubated with a 40
pg/ml solution of human purified fibronectin (Invitrogen) for at least 1 h. About
100,000 MSC were trypsinized and resuspended in 200 pl of buffer A, with or without
240 pg/ml of the cell attachment region of fibronectin. MSC were incubated in
suspension for 30 min at 37"C, pelleted, and then resuspended in 30pl buffer A with 0.1%
human serum albumin (HSA; Sigma-Aldrich). 10pl of the MSC suspension was then
carefully transferred onto the fibronectin-coated Delta T dish containing 4 0 0 pI buffer A.
At least 30 MSC were then imaged in 3 random fields over 3 consecutive 6 min
durations. Live-cell imaging was conducted as above using a 40X oil immersion objective.
Blebbing MSC were then expressed as a percentage of the total number of MSC imaged.
3.3.9
Transmission Electron Microscopy
57
Transmission electron microscopy was performed as described previously (252). Briefly,
MSC were incubated on TNF-t-activated GPNTs grown on fibronectin-coated glass for
30 min and then fixed with 2.5% glutaraldehyde and 2% paraformaldehyde in 1.0 M
sodium cacodylate buffer, pH 7.4, for 2 h, post-fixed in 1.5% sym-collidine-buffered
OsO4 for 1 h, stained en bloc with uranyl acetate, dehydrated in alcohol and embedded
in eponate. Thin eponate sections of 90 nm were visualized with a Philips CM-10
electron microscope.
3.3.10 Statistical Analysis
In our studies we used pooled MSC donor data whereby an individual experiment (i.e., n
= 1) was always done with MSC from a single donor and among the total averaged
replicates at least two different donors were included. Results were presented as mean ±
s.e.m for n > 3. For comparisons between two groups, Student's t tests were used.
Comparisons between multiple groups (>2) were performed with one-way analysis of
variance (ANOVA) with Tukey's post-hoc test, unless otherwise stated. Asterisks indicate
statistically significant differences of p<0.05 (*), p<0.0I (**) or p<0.001 (***).
58
3.4 RESULTS
3.4.1
MSC transmigrate in an inflammation-, Gai- and VCAM-1-dependent manner
To investigate the mechanisms for inflammation-specific extravasation of MSC, we set
up in vitro models of 'resting'/'quiescent' and cytokine-'activated' microvascular
endothelium. Specifically, we cultured confluent monolayers of primary human lung
(hLMVEC) and cardiac (hCMVEC) microvascular endothelial cells (MVEC) and
activated them with the potent inflammatory cytokine TNF-a. MVEC activation was
confirmed by strongly upregulated expression of the adhesion molecules VCAM-1 and
ICAM-1 (Fig.S3.1A). Early passage (P3-P7) primary human bone marrow-derived MSC
(which were confirmed to be minimally senescent; Fig.S3.1B (253)) were detached from
tissue culture dishes and incubated on TNF-a activated endothelial monolayers for 1
hour, followed by washing and fixation. Through imaging-based methods we confirm
previous observations (153, 184) that endothelial activation enhances MSC-endothelial
interactions, as noted by increased density of MSC remaining associated with the
endothelium (Fig. 3.1A).
To quantify and further characterize this observation we employed confocal fluorescence
microscopy. This allowed for assessment of MSC positioning with respect to the
endothelium in one of 3 states: 1) Apical: Completely on the upper/apical surface of the
endothelial monolayer, 2) Transmigrating: Spanning across the endothelium and
partially occupying both the apical and subendothelial/basal spaces or 3) Basal:
Completely under/basal to the endothelium (see Fig. 3.1Bi, schematic). We interpreted
these to represent MSC that had not yet initiated, were in the process of, or had
completed transmigration, respectively. We quantified both total MSC (all 3 states; as a
measure of overall interaction efficiency), as well as MSC that were either
Transmigrating or Basal to the endothelium (as a measure of transmigration frequency).
In both cases the numbers of MSC were increased 2-3 fold on TNF-ct-treated
endothelium (Fig. 3.1Bii) demonstrating that endothelial activation promotes both
adhesion and transmigration of MSC.
Activated endothelia express and present a range of chemokines(172, 254) some of which
have been implicated in MSC transmigration in bone marrow(255). To probe the idea
that MSC adhesion and transmigration in our model may be dependent in part on
chemokines, we employed PTX, a broad-acting inhibitor of chemokine receptor
signaling via ADP-ribosylation of the G protein Gai. Pretreatment of MSC with PTX
(under conditions that did not alter cell viability; Fig.S3.2A), indeed, significantly
inhibited their adhesion to and transmigration across activated MVEC (Fig. 3.1C).
Ai
AN
U
LU
w
Bi
Bii
150-
**
*
**
Q
A
U)
100-
Apical
Total MSC
interacting
with
Endothelium
.
0
t
50-
hLMVEC
LBasal
C
+
-
TNF-a:
Transmigration
0
*m
±
Spanning
MSC initiated
or Completed
U
A
V
-
+
4-oi
+
-
hCMVEC
+
-
hLMVEC
hCMVEC
Transmigrating and
All MSC
Basal MSC only
D
C1
--
60-
4*
C2
0
H7
4-
k-.~
A
0
**
40
40
-I-
VI
20
A
S
S
TNF-a: -
PTx:
+
M
All MSC
+
+
+
+
Transmigrating
and Basal
MSC only
TNF-w: -
IFN-y:Anti-VCAM-1:
+
A
0
-
V
0
0
1.
11
1,111,
+
-
0
0
0
+
-
+
-
+
+
+
+
-
-
-
+
+
-
-
+
-
All MSC
--
-
-
+
+
Transmigrating and
Basal MSC only
Figure 3.1 MSC preferentially transmigrate through TNF-a activated lung and cardiac endothelium.
(A) DiO-labeled MSC (green) were incubated on resting (i) or TNF-a activated (ii) DiI-labeled human lung
microvascular endothelium (hLMVEC; red) for 60 min, followed by fixation and imaging by fluorescent and
phase-contrast microscopy. Representative micrographs are shown. Scale bars represent 100 pm.
(B) MSC were incubated on resting or TNF-a activated hLMVEC and hCMVEC for 60 min, followed by
fixation, staining and imaging by fluorescent confocal microscopy. (i) MSC were counted and classified
according to their positions relative to endothelium: Apical, Spanning or Basal. (ii) Both the total number of
MSC, and the number of MSC in only the transmigrating or basal positions were compared on TNFactivated and resting endothelium for both hLMVEC and hCMVEC.
(C) MSC were incubated on resting or TNF-a activated hCMVEC for 60 min. In some cases, MSC were
incubated with 100 ng/ml of pertussis toxin (PTX) for 2 h prior to be added to endothelium. As in B, both
the total number of MSC, and the number of MSC in only the transmigrating positions were compared for
all conditions.
(D) MSC were incubated on resting, or TNF-a activated and/or IFN-y activated hCMVEC for 60 min. In
some cases, TNF-a activated endothelium was incubated with 20 gg/ml blocking antibodies against VCAM- 1
for 30 min prior to the addition of MSC. Samples were fixed, stained and imaged by fluorescent confocal
microscopy. As in B, both the total number of MSC, and the number of MSC in only the transmigrating or
basal positions were compared for all conditions.
For Bii, C and D, data were collected from at least 6 microscopic fields for each experimental condition.
Values represent mean ± s.e.m.. 1, 2, or 3 asterisks indicate 3 levels statistically significant differences (p<0.05,
p< 0 . 0 1, and p< 0 . 0 0 0 1 respectively). For B, this was assessed by a two-tailed, paired Student's t-test. For C
and D, this was assessed by a one-way ANOVA test with a Tukey post-hoc test.
61
Previous studies have implicated the integrin very late antigen-4 (VLA-4) and its ligand
VCAM-1 in MSC adherence to endothelium(153, 184). We compared MSC adhesion
and transmigration on MVEC activated TNF-a with versus IFN-y, which contrasting
TNF-a was ineffective at upregulating VCAM-1 (Fig. S3.1A), and found that only
TNF-L could promote MSC-MVEC interactions (Fig. 3.1 D). Similar studies with a rat
brain endothelial cell line (GPNT (246, 247)) in which both TNF-a and IFN-y failed to
significantly upregulate VCAM-1 (Fig. S3.1A) showed that both cytokines failed to
upregulate MSC interactions (Fig. S3.2B). We found that function-blocking antibodies
to VCAM-1 significantly blocked the TNF-a-mediated upregulation of MSC adhesion
and transmigration on MVEC (Fig.1D and S2C). Finally, function-blocking antibodies
to the VCAM-1 receptor VLA-4 (which we confirmed was expressed by MSC; Fig.
S3.2D) similarly block MSC-MVEC interactions (Fig. S3.2C).
3.4.2
MSC actively transmigrate both between and directly through endothelial cells in
association with 'transmigratory cups'
Previous studies with static imaging suggested that rather than transmigrating, MSC
'integrate' into the endothelial monolayer by causing endothelial cell retraction, and
spreading on the underlying matrix (94, 239, 240). This is in contrast to leukocytes
which transmigrate through discrete pores and gaps in the endothelium, and
progressively spread underneath endothelium (244). To determine if MSC integrate or
actively transmigrate across the endothelium in our model of inflamed MVEC, we
conducted detailed high-resolution confocal imaging analysis (Fig. 3.2). In samples fixed
after 1 hour co-incubation, we observed that some MSC indeed underwent integration.
However, we also largely encountered 5 distinct morphological arrangements consistent
with progressive stages of a discrete and active transmigration process.
Stage 1 - Adherence: Relatively spherical MSC adhered to the flat apical surface of a
continuous, intact endothelial monolayer (Fig. 3.2A). Stage 2 - Transmigratory Cup
Formation: Adherent MSC were partially 'embraced' by microvilli-like endothelial
projections that extended vertically and were enriched in actin and VCAM-1 (Fig. 3.2B,
white arrows, and Video 3.1) in similar fashion to transmigratory cups formed during
leukocyte diapedesis (244, 250, 256). Contrasting leukocytes (114, 172), apically
adherent MSC (i.e., Stage 1 and 2) did not exhibit significant spreading or polarization.
Stage 3 - Gap/Pore Formation: Transmigratory cup-associated MSC exhibited bulbous
basal protrusions that extended across discrete gaps or pores in the endothelium, which
were in direct contact with the underlying substrate (Fig. 3.2C, blue arrows). Stage 4 Subendothelial Spreading: MSC still remained partially above and spanning across the
endothelium, but showed increased amounts of membrane spread out beneath the
endothelium (Fig. 3.2D i-iv). Stage 5 - Transmigration Completed: MSC that had
completed transmigration were spread entirely underneath the endothelial monolayer
(Fig. 3.2E).
A Stage 1: Adherence
C Stage 3: Gap/Pore
B Stage 2: Transmigratory
Formation
Cup Formation
...
D
..
..
E Stage 5: Transmigration Completed
Stage 4: Subendothelial Spreading
sCgap
-MC leading edge
v Integrational
Spreading
*- - -- - - -- -
-- - -
--SCledngd
T%vo Routes of MSC Transmigration
F
i Paracellular
EC1
EC2
v Transcellular
Adherens
iunction
EC1ECC
AJ)/
Figure 3.2 The 5 stages and 2 routes of MSC transmigration.
Five distinct stages (A-E) of transmigration were consistently observed for MSC, based on previously
established leukocyte morphological analysis (244), presented as both schematics (Ai; Bi; Ci; Di, iv, v, vii; Ei;
Fi, v; see also Fig. SI) and confocal projections (Ali, Bii-iii, Cii, Dii, iii, vi; Eii-iv; Fii-iv, vi-viii). Confocal
projections include top (x-y) and orthogonal (x-z and y-z) cross-sections. (A) Stage 1: Adherence. A relatively
spherical MSC (CTx-B; green) is adherent to the apical surface of an intact GPNT monolayer as seen by
ICAM- 1 (EC surface; red) and VE-cadherin (EC junctions; blue) staining.
(B) Stage 2: Transmigratory Cup Formation. VCAM-1-enriched microvilli-like vertical projections (white
arrows) that extend up from hLMVEC endothelium (VCAM-1; red) and form a 'cup-like' structure around
the base of the MSC (CD90; green) at 60 min. Actin is stained in blue. 3D projections (rotated 00, 450 and
900 about y and z axes) are shown in (iii). See also Video 1.
(C) Stage 3: Gap/Pore Formation. A discrete hCMVEC endothelial discontinuity is occupied by the basal
portion of an MSC in contact with the substrate (blue arrows) indicating initiation of transmigration at 60
min. Sample stained as in B. Note blebs extending from the MSC surface (yellow arrows).
(D) Stage 4: Subendothelial Spreading. A representative MSC is shown spreading beneath intact hLMVEC
endothelium via a discrete gap. Orthogonal projections (ii) and a merged image (iii) is shown. This is in
contrast to integration (schematic,v; orthogonal projection, vi), where MSC displace endothelial cells by
spreading between adjacent EC. MSC leading edges and gaps in the EC are outlined in iv and vi to highlight
the distinct endothelial gaps which are typically formed during transmigration through endothelium versus
integration within an endothelial monolayer. Samples stained as in B.
(E) Stage 5: Transmigration Completed. Representative orthogonal views (ii) indicate an MSC completely
under the endothelium at 60 min. Top view projections, with (iii) or without (iv) MSC shown,
demonstrating intact endothelium.
(F) Two Routes of MSC Transmigration, paracellular and transcellular, are shown. MSC incubated on
GPNT ECs for 60 min were fixed and stained for VE-cadherin (green), CTx-B (MSC; red) and ICAM-1
(blue). Representative images of MSC at similar late stages in diapedesis migrating either through a
paracellular gap between two endothelial cells (i-iv) or through a transcellular pore across a single endothelial
cell (v-viii). Images are either top view projections of entire z-stacks (ii, vi) or single sections alone (iv, viii) or
together with orthogonal projections (iii and vii). The red MSC (CTx-B) signal was omitted for panels iv and
viii to enhance visualization of the transmigration passageway. Note that in both events, only a small rounded
portion of the MSC still remains above the endothelium. In ii-iv the MSC migrates through a small (-2 pm
in diameter) paracellular gap (iii, yellow arrows) between two cells where the adherens junction (AJ, white
arrows) has been disrupted. In vi-viii the MSC passes through a small (-1 pm in diameter) transcellular pore
(vi, yellow arrow) distinct from intact adherens junctions (white arrows).
Scale bars represent 20 pm.
64
As noted above, varying fractions of MSC (- 1% on GPNT, up to -50% on hCMVEC)
caused large-scale disruption of the endothelium, integrating into the monolayer rather
than migrating across it (Fig. 3.2D v-vii). Using dynamic live-cell imaging, we further
confirmed that MSC co-incubation could lead to progressive retraction of endothelium
coupled with MSC spreading on the substrate (data not shown). Although not quantified,
we observed that integration events were more frequent when a given endothelial
monolayer a priori exhibited relatively low confluency or showed signs or poor health
and defective integrity (i.e., pre-existing intercellular gaps). On our blood-brain-barrier
endothelial model (i.e., GPNT), which consistently provided an endothelial barrier of
exceptionally high integrity, MSC integration was only very rarely observed and
transmigration nearly always occurred through highly discrete gaps and pores (e.g., Fig.
3.2F).
Significantly, in the course of the above investigation, we noted that apart from
integration, MSC apparently could utilize two distinct pathways or 'routes' for crossing
the endothelial barrier like leukocytes (238). In the majority of diapedesis events the
MSC migrated across paracellular gaps via the local disruption of the adherens (Fig.
S3.3A) and tight (Fig. S3.3B) junctions. Interestingly, junctional adhesion molecule-1
(JAM-1; a tight junction marker (257)) also exhibited modest enrichment in
transmigratory cups (Fig. S3.3C). Less frequently (-20-30% of diapedesis events) MSC
migrated directly through individual endothelial cells via de novo formation of
transcellular pores in endothelial cells (Fig. 3.2F v-viii).
3.4.3
MSC undergo relatively slow transmigration in the absence of lateral migration
Next, to assess the kinetics of MSC transmigration, we incubated the MSC with the
activated hLMVEC for 30, 60 and 120 min, and then quantified the fraction of MSC
that were apical, transmigrating or basal to endothelium as in Fig. 3.1. These studies
showed that >90% of adherent MSC initiated transmigration within 30 minutes, while
about 50% completed the process only after 120 minutes (Fig. 3.3A).
A
u"
E
MSC Positions Relative
to Endothelium
0
0)8
0 V) 1.0
Apical
.2
Transmigrating
0.4
S
0mm
A TjB A T B
0 min 30 min
A T
60 min
Basal
A T 8 : MSC Position Relative to EC
120 min Time of MSC-EC Interaction
Figure 3.3 MSC transmigration kinetics and absence of lateral migration
(A) MSC were incubated on hLMVEC for 30, 60 or 120 min, then fixed, stained and imaged as in Fig. 3.2.
As in Fig. 1B, MSC were counted and classified according to their positions relative to endothelium: Apical,
Spanning or Basal. Values represent mean ± s.e.m.. Asterisks indicate a statistically significant difference
(p<0.05) as assessed by a one-way ANOVA test with a Tukey post-hoc test, n=3.
(B) MSC were subjected to live cell DIC (left panels) and fluorescence (middle panels) imaging during
interaction with activated memDsRed-transfected hLMVEC (red). Still frames from the video at 0, 15, 30
and 45 min are shown. Numbers identify 6 separate MSC. Blue and yellow arrows indicate 2 MSC (#1 and
#2) in the active process of transmigration as indicated in part by the expanding transmigration passageways
in the endothelium; White dashed lines (middle panels, bottom row) indicate intercellular junctions between
two ECs ('ECI' and 'EC2'), blue dashed line indicates a paracellular gap for migration of MSC #1, yellow
dashed line indicates a transcellular pore for transmigration of MSC #2. Pink and green dashed lines (left
frames; MSC #3 and #5) represent the location of 2 different apical MSC in the preceding panel (i.e., lines at
15 min panel show the MSC positions in 0 min panel, etc.) and highlight a lack of significant lateral
migration. Orange arrow, MSC #6 (15 min time point) indicates the protrusion of an MSC bleb against the
endothelial surface. See also Video 3.2.
Scale bars represent 20 pm.
67
To better integrate the stages of transmigration observed through fixed-cell studies (i.e.,
Fig. 3.2), we turned to live-cell microscopy. Consistent with the fixed-cell imaging
studies, adherent MSC (i.e., that had not yet transitioned to gap/pore formation)
retained a relatively spherical morphology. MSC also exhibited very limited net lateral
movement over the endothelial surface; though movement velocities averaged 3.08 ± 0.3
pm/min, total displacement over 30-60 minutes was usually only -1-3 pm (Fig. 3.3B
and Video 3.2, MSC #3-6). Additionally, live-cell imaging revealed that the formal phase
of transmigration (i.e., initial formation of a gap or pore until the completion of
diapedesis) is a relatively slow process. "hether migrating paracellularly or transcellularly,
MSC typically required at least 45 min for this phase of migration (Fig. 3.3B and Video
3.2, MSC #1 and #2). It should be noted, however, that such extended durations
precluded the visualization of complete transmigration events (i.e., Stages 1-5) for
individual MSC, due to technical challenges associated with such long-term imaging (e.g.,
cytotoxicity and photobleaching).
3.4.4
Transmigrating MSC exhibit extensive non-apoptotic membrane blebbing
The above findings (Fig. 3.2, 3.3 and Video 3.2) show an absence of polarization,
limited lateral migration and lack of characteristic protrusive structures (e.g., lamellipodia,
pseudopodia and invadosomes (114, 172)) associated with leukocyte diapedesis.
However, these initial live-cell imaging studies showed instead dynamic extension and
retraction of membrane bleb-like protrusions and (e.g., Video 3.2, MSC #5 and 6),
apparently related, more amorphous 'worm-like' protrusions with somewhat longer
lifetimes (e.g., Video 2, MSC #3 and #4). We had also noted apparent 'snap-shots' of
such protrusive activity in initial fixed-cell imaging (e.g., Fig. 3.2C, yellow arrows).
Further high-resolution imaging of this phenomenon clearly showed that blebs formed
over all surfaces of the MSC, including those in intimate contact with endothelium and
at sites of endothelial pore or gap formation (Fig. 3.4A and Video 3.3). Interestingly, we
observed that classic F-actin free cell surface membrane blebs (in which the membrane
had apparently detached from the underlying cortical actin layer; Fig. 3.4A, C, white
arrows, and Video 3.3) coexisted in individual MSC with morphologically similar blebs
that were strongly enriched in F-actin at the outer membrane (Fig. 4A,C, yellow arrows,
and Video 3.3). Qualitative (Video 3.4) and quantitative (Fig. 3.4B) analysis revealed
that the majority of MSC, whether on resting or activated endothelium, exhibited blebs,
whereas a minority exhibited filopodia instead. It is unknown if filopodia-possessing
MSC are a distinct subset from blebbing MSC, however, a small subset of MSC
expressed both filopodia and blebs (Fig. 3.4B), indicating that filopodia and blebs were
not necessarily mutually exclusive.
C
Ci
A
D
C
B
1o0-
*
080-
o
40-
>20-
0-%
Bieb
Filopodia
Bleb +
Filopodia
Elv
Ei
U
EC (alone)
EC (MSC-EC co-inc)
MSC (alone)
IMSC (MSC4C conc)
(alone +H20)
+
Non-
MSC-EC co-incubation
MSC alone + H202-induced Apoptosis
Early
apoptotic apoptosis
+
Late apuptosis
andnectosis
Figure 3.4 MSC exhibit extensive non-apoptotic blebbing on endothelium
(A) MSC were incubated for 60 min on activated hLMVEC, then fixed and stained for CD90 (green), VCAM-1 (red) and actin (blue). A representative
top view confocal projection of a MSC at an early stage of transcellular diapedesis is shown. Multiple highly rounded, bleb-like structures can be seen
protruding from the MSC surface, which are both negative (white arrows) and positive (yellow arrows) for cortical F-actin (blue). See also Video 3.
(B) MSC were incubated on resting or TNF-a activated hCMVEC for 60 min. At least 30 MSC were counted for each condition per experiment (n =3).
The fraction of MSC exhibiting either blebs, filopodia or both were quantified as shown. Values represent mean ± s.e.m., p<0.05, as assessed by paired
Student's t test. See also related Video 4.
(C) MSC were incubated for 60 min on activated hLMVEC and then fixed. To ascertain whether or not blebbing reflected MSC apoptosis, samples
stained for CD90 (green), actin (red) and nuclear morphology (ToPro3; blue). A representative example of early stage diapedesis is shown. Both single
top view (x-y plane) confocal sections (i), and top view projections/orthogonal cross-sections (ii) show clearly presents of F-actin negative (white arrows)
and positive (yellow arrows) and blebs over all MSC surfaces, including those in direct contact with the endothelium. The MSC nucleus (distinguished
from neighboring endothelial nuclei with an asterisk) shows normal intact morphology (rather than the canonical fragmented morphology seen during
apoptosis) as seen by confocal cross-section (i), orthogonal view (ii) and 3D volumetric rendering (iii).
(D) MSC were incubated for 30 min on GPNTs, fixed and then processed for, and imaged by, transmission electron microscopy. Micrograph depicts a
representative MSC on endothelium (EC, 10% opacity red overlay) with clearly evident micron-scale cell surface blebs (green arrows) and an intact
nucleus (highlighted with a 10% opacity blue overlay).
(E) (i-iii) MSC were either incubated on hLMVEC for 30 min or on tissue culture plastic in the presence of 5 mM hydrogen peroxide for 2 h, followed
by fixation and staining for CD90 (green), F-actin (red) and annexin V (blue). Representative images show confocal projections of annexin V-negative
blebbing MSC on hLMVEC (i) and annexin V-positive MSC exhibiting hydrogen peroxide-induced apoptosis (ii, iii). (iv) Flow cytometric analysis of
annexin V- and propidium iodide (PI)-stained EC (shades of green) and MSC (shades of blue) following separate culture (with or without 2 h treatment
with 5 mM hydrogen peroxide for MSC) or 1 h EC-MSC co-incubation. Percentage of cells in each condition that were non-apototic (annexin V and
PI negative), in early apoptosis (annexin V positive, PI negative) and late apoptosis/necrosis (annexin V and PI positive) are shown. Values are mean
s.e.m, n = 3.. Asterisks indicate a statistically significant difference as assessed by a one-way ANOVA test with a Tukey post-hoc test.
Scale bars represent 20 pm for A, C and E and 5 pm for D.
70
Blebbing is classically associated with apoptosis. However, some embryonic and tumor
cells have been shown to employ non-apoptotic migratory blebbing for motility and
invasion (241-243). To determine whether or not blebbing MSC were undergoing
apoptosis we stained the nuclei with ToPro3 and conducted high-resolution confocal
imaging and digital 3D-reconstruction. In all cases nuclei of blebbing MSC were healthy
and intact, showing none of the canonical nuclear fragmentation that is associated with
apoptosis (Fig. 3.4C, see asterisks in i-iii). This observation was confirmed by
transmission electron microscopy imaging of nuclei (Fig. 3.4D). Furthermore, MSC
cultured alone or co-incubated with EC showed a lack of detectable staining for Annexin
V or propidium-iodide, as assessed by microscopic (Fig. 3.4Ei-iii) and flow cytometric
analyses (Fig. 3.4Eiv).
3.4.5
MSC display non-apoptotic blebbing in association with early transmigration stages and
can exert forces on endothelium
To elucidate the dynamics of MSC blebbing during transmigration, we conducted livecell imaging on TNF-a activated endothelium. High temporal resolution DIC imaging
revealed repetitive cycles of rapid bleb expansion (average time of 15.22 ± 0.92 seconds
to reach maximal size of 1-5pm), followed by a significantly slower phase of retraction
(average time of 43.52 ± 2.40 seconds) (Video 3.4, 'Example 1'). These kinetics are
highly consistent with those of migratory blebs formed by some tumor and embryonic
cells (241-243).
As noted with the fixed-cell imaging studies, blebs protruded from all surfaces of the
MSC including those in direct contact with the endothelium. Blebs that formed against
the endothelium often were coupled with 'jerky' MSC movements suggesting that
significant intercellular forces were being developed (e.g., Video 3.2, MSC #3, #4 and #6
(note orange arrow) and Video 3.5, Examples 2-4). Next, we conducted studies using EC
transfected with soluble GFP, a previously developed to monitor local cytoplasmic
volume in EC as a readout for topological dynamics (252). We found that as MSC
protruded blebs against endothelium, spatially and temporally correlated regions of low
GFP intensity developed in the apposing EC (Fig. 3.5A). We interpreted this to signify
formation of cytoplasm-displacing endothelial invaginations caused by MSC blebs
driving the apical surface of the endothelium toward its basal surface. We confirmed this
interpretation with interference reflection microscopy (IRM), a modality that reveals
regions of close cell-substrate apposition as dark areas (251) (Fig. 3.5B and Video 3.5,
Example 2).
A
D
E
MSC on
hCMVEC
F
MSC on FNCoated Glass
C
£
-C
I..
U
.0
71
30-
G
Figure 3.5 MSC use non-apoptotic blebs to exert force on surroundings
(A) MSC were imaged live on TNF-a-activated hCMVEC transfected with soluble GFP (sGFP). We
previously established that sGFP serves as a sensitive readout for local cytoplasmic volume and, indirectly,
surface topology of endothelial cells (252). Images show sequential still frames of a single MSC on an sGFPexpressing hCMVEC at 30 sec intervals. By DIC blebs can be seen protruding from the basal surface of the
MSC against the endothelial cell surface (arrows). Note that at t = 0 sec one bleb (pink arrow) has formed that
corresponds to a decrease in local sGFP signal indicating an endothelial cell surface depression/invagination
and consequent displacement of cytoplasm. In the subsequent frame that bleb has partially retracted and the
endothelial depression has disappeared. At the same time a distinct bleb and endothelial depression (blue
arrow) form de novo.
(B) MSC were imaged live on TNF-a activated hCMVEC with both DIC (top row) and interference
reflection (bottom row; IRM) microscopy. Images are sequential still frames of a single MSC on hCMVEC at
30 sec intervals. At t = 0 sec one bleb (pink arrow) has generated a dark area in the corresponding IRM image
indicating that the basal surface of the endothelial cell has been locally depressed and forced into close
opposition with the underlying glass substrate. In the subsequent frame this bleb retracts and the endothelial
depression (i.e., IRM dark spot) disappears. At the same time a distinct bleb and endothelial cell depression
(blue arrow) form de novo. See also similar experiment in Video 3.5 'Example 2'.
(C) MSC were imaged live on TNF-a activated, mem-RFP transfected hLMVEC with both DIC (top row)
and fluorescence (bottom row) microscopy. Images are still frames separated by a -10 min interval. Left
panels show an MSC adherent over an intact intercellular junction (dashed line) formed between a positive
mem-RFP transfected ('EC1', red) and a non-transfected ('EC2', black) hLMVEC. Right panels show that
commensurate with the onset of blebbing, a large (-5 pm) rounded intercellular gap forms under the MSC.
See also corresponding Video 3.5, 'Example 4'.
(D) MSC were imaged live on mem-GFP transfected hLMVEC with both DIC (left) and fluorescence (right)
microscopy. Images are still frames of a single MSC migrating through a transcellular pore in a mem-GFP
positive endothelial cell. For this 'fried egg-shaped' MSC the peripheral blebbing regions of the MSC have
already spread beneath the endothelium (See Fig. S3.1, bottom, right 'multiple leading fronts'), where the
central 'yolk' region is spanning across and partially above the endothelium. Arrows indicate dynamic MSC
blebs expanding and apparently exerting force on the endothelium as seen by corresponding distortions in the
endothelial cell topology. See the corresponding dynamics in Video 3.5, 'Example 5'.
(E) The extent to which 'non-apoptotic migratory blebbing' was associated with MSC at different stages of
transmigration was quantified. MSC were incubated on TNF-a activated hCMVEC for 30, 60 or 120 min.
Individual MSC were classified according to their position (as in Fig. 3.1B) relative to endothelium and of the
percentage of blebbing MSC in each position is shown. Five independent experiments were performed, and a
total of 85, 133 and 45 apical, transmigrating and basal MSC, respectively were counted. Values represent
mean ± s.e.m.. p<0.05, as assessed by unpaired Student's t test.
(F) The association between MSC blebbing and avidity for a rigid substrate was explored. MSC were
incubated in either serum-free media ('Control'), or serum-free media containing 240 pg/ml of the achymotryptic fragment (cell attachment region) of fibronectin ('FN-Block') for 30 min, before being
transferred to a fibronectin-coated glass dish. Three consecutive 6 minute videos of MSC were captured for
each experimental condition, and the percentage of MSC which exhibited blebbing (described in Materials
and Methods) is shown. Values represent mean ± s.e.m. p<0.05, as assessed by paired Student's t test.
(G) GFP-actin (green; central and right panels) transfected MSC were imaged live during transmigration
across activated hLMVEC via both DIC and fluorescence microscopy. The depicted example shows a
relatively late stage diapedesis event (i.e., slightly advanced stage compared to Fig. 3.5D) in which the MCS is
advancing part of its membrane under the endothelium through cycles of bleb expansion and retraction.
Images are sequential still frames at 20 or 40 sec intervals. Consistent with the fixed cell imaging in Fig.
3.4A,C, blebs can be seen (via the DIC imaging; left and right panels) protruding from the MSC that are
both negative (white arrows) and positive (yellow arrows) for GFP-actin. Red dashed lines (right panels)
delineate the edge of MSC membrane during bleb formation, whereas blue dashed line indicates the 'edge'
GFP-actin signal. Note that cycles of actin-negative bleb formation, followed by actin recruitment to the bleb
and subsequent bleb retraction occur as the cell advances, features are highly similar to non-apoptotic
migratory blebbing activities exhibited by some tumor and embryonic cell types (241-243, 258). See also
Video 3.7.
Scale bars represent 20 pm.
73
Further studies, in which EC were transfected with plasma membrane markers (i.e.
mem-DsRed or mem-YFP), suggest that blebs continue to form and exert forces during
endothelial gap/pore formation (Fig. 3.5C and Video 3.5, Example 3, 4) and
subendothelial spreading (Fig. 3.5D and Video 3.5, Example 5). Toward the end of the
transmigration process, when MSC had formed significant contacts with the
subendothelial fibronectin, blebbing was progressively diminished and replaced by
radially spreading lamellipodia (Video 3.5, Example 5). Quantitative fixed-cell analysis
confirmed that the majority of apical or transmigrating MSC were associated with nonapoptotic migratory blebs, whereas those that were basal to endothelium had largely lost
their blebs (Fig. 3.5E).
Non-apoptotic migratory blebbing in general has been suggested to reflect a cell's
response to reduced substratum adhesion (241, 242, 259). We hypothesized that
modestly avid adhesion of MSC to endothelium may be permissive for blebbing, whereas
high avidity adhesion to subendothelial matrix is not. To test this idea MSC in
suspension were pre-incubated with or without the soluble cell-binding fragment of
fibronectin, and then seeded on fibronectin-coated substrate. As expected, control MSC
exhibited very limited blebbing and initiated lamellipodial spreading almost immediately
(Fig. 3.5F and Video 3.6, Part 1). However, when adhesion to the fibronectin-coated
substrate was blocked, spreading was blocked (not shown) and MSC blebbing was
preserved (Fig. 3.5F). Interestingly, when fibroblasts were seeded on activated
endothelium, no blebbing was observed demonstrating that the blebbing response is not
universal (Video 3.6, Part 2).
Finally, we performed live-cell imaging of MSC transfected with GFP-actin. These
studies show that individual MSC blebs formed during transendothelial migration
consistently exhibited cycles of rapid protrusion of actin-free blebs, followed shortly by
recruitment of actin to the bleb and finally a somewhat slower phase of bleb retraction
(Fig. 3.5G and Video 3.7). This was in agreement with our high-resolution confocal
imaging that showed co-existence of both cortical actin-free and F-actin-enriched MSC
blebs (Fig. 4A, C, white and yellow arrows, and Video 3). Importantly, as seen Fig. 3.5G
and Video 3.7, these cycles were coupled to the advancement of the subendothelial
leading edge of the transmigrating MSC. Overall, these features are highly consistent
with migratory blebbing mechanisms previously characterized in other cells (241, 242).
3.5 DISCUSSION
Exogenously infused and endogenous MSC are known to circulate and preferentially engraft at
sites of inflammation in vivo. However, the process by which they migrate across the endothelial
barrier to exit the circulation and engraft has remained incompletely understood. Here we
uncover a transmigratory process that combines leukocyte-like and unique mechanistic features
(Fig. 3.6).
The molecular mechanisms underpinning the specificity of MSC extravasation at sites of
inflammation likely includes activation of endothelium by pro-inflammatory cytokines. TNF-a
stimulates expression and presentation of a range of chemokines and adhesion molecules by
endothelial cells (172, 254). Consistent with previous reports (184, 240, 260, 261), we observed
that both MSC adhesion and transmigration increased upon activation of endothelium with
TNF-a. This in turn was mediated through Gui (and thus likely chemokine)- and VLA4/VCAM- 1 -dependent mechanisms. With respect to chemokines, two recent studies have
directly implicated roles for CXCL9, CXCL16, CCL20, and CCL25 (for which MSC express
cognate receptors) in augmenting transmigration (255, 260). It is likely that other surface
proteins and soluble factors, such as matrix metalloproteases (151, 262), are also involved that
remain to be further investigated.
The cellular basis for MSC transmigration has been much less well resolved. Previous reports
which attempted to morphologically characterize the process of MSC transmigration, albeit with
limited resolution, have described a process termed integration (94, 239, 240). In such studies,
large-scale retraction of endothelium coupled to MSC spreading on the substrate was inferred
from static images. In this study, we aimed to improve upon the current knowledge by
employing both high-resolution and dynamic imaging modalities in combination with specific
molecular markers. In this way, we confirm that MSC co-incubation can induce progressive
retraction of large regions of endothelium that accommodate MSC spreading and integrating. In
addition, we also demonstrated for the first time that MSC can also mediate two other types of
transmigration, namely, paracellular and transcellular diapedesis. Contrasting integration, the
endothelium remained largely intact during diapedesis and MSC actively squeezed through
discrete pores and gaps in the endothelium to enter the sub-endothelial space. The finding that
MSC can initiate transcellular diapedesis is particularly compelling evidence that MSC can
actively breach endothelial barriers as, contrasting paracellular gaps, transcellular endothelial
pores never form autonomously form in these settings (244, 252).
We also noticed that during diapedesis, the endothelium projected actin-, VCAM-1- and JAM1-rich finger-like protrusions from its surface that surrounds the MSC forming transmigratory
cups similar to those shown to guide leukocyte transmigration (244). This suggests that MSC
diapedesis is also a cooperative event between both MSC and endothelial cells. Whether JAM-1
localization to transmigratory cups is a result of engagement of a specific ligand on MSC or
occurs through some type of lateral association with VCAM-1 (263) remains an open question.
Leukocyte Adhesion Cascade
Single leading front:
Lamellipodia
Lamellipodia
Cup formation.
~?spm/mmn
Invadosomes
Rolling
Activation
Firm
Adhesion
Lateral
Migration
Diapedesis
10-20min
Proposed Mesenchymal Stem Cell Adhesion Cascade
Beb..,
Rolling
Activation ?
Firm
Adhesion
No Lateral
Cup formation.
Multiple leading fronts
Diapedesis
Migration
60-1 20min
Figure 3.6. Comparison between the leukocyte transmigration cascade and the proposed MSC transmigration cascade
Discrete steps in the leukocyte adhesion cascade (top panel) and the proposed MSC adhesion cascade (bottom panel). Labels in red indicate key
differences between the 2 processes, while labels in black indicate similarities. Leukocytes (light green) roll on activated endothelium (red) via selectins,
which are upregulated on the endothelial surface during inflammation. MSC (dark green) also roll on endothelium (153). Rolling brings leukocytes in
closer proximity to the endothelial surface where chemokines (red asterisks) are presented. GPCR receptors on the leukocyte (top left inset) recognize
the chemokines, leading to conformational rearrangement of leukocyte surface integrins adhesion receptors that are coupled increased ligand binding
affinity. This allows high affinity binding to complementary ligands such as ICAM-1 and VCAM-1 on the endothelial cell surface endothelial surface
thereby inducing firm adhesion of the leukocyte. Although firm adhesion of MSC occurs (153) it is currently unknown if this occurs through a similar
activation step (bottom left inset). For leukocytes, adhesion is followed by an important phase of polarization and lateral migration, during which they
employ actin-dependent protrusions, including lamellipodia, pseudopodia and invadosomes, for motility (top middle inset) and migratory pathfinding
(top middle and right inset). In contrast MSC do not exhibit significant polarization or lateral migration on the apical surface of the endothelium.
Moreover, there is no evidence that MSC utilize lamellipodia, pseudopodia or invadosomes during initiation of diapedesis. Intriguingly, however, they
do display distinct and highly dynamics non-apoptotic blebbing protrusions. These form initially without cortical actin (bottom right inset, yellow line),
but subsequently become enriched in actin (dashed yellow line), which is followed by bleb retraction. In some tumor and embryonic cell types such
non-apoptotic blebbing serves as mechanistic basis for motility and invasion (241-243, 258). Blebs are proposed here as putative mechanisms by which
MSC exert force on the endothelial surface (bottom right inset, black arrow), or search for adhesion points and sites permissive for transmigration.
Though they appear to initiate transmigration through different protrusive activities, leukocytes and MSC both trigger proactive endothelial extension
of microvilli-like, actin, ICAM-1 and VCAM-1 endothelial projections that form 'transmigratory cups', which are thought to facilitate diapedesis.
Additionally, both cell types exhibit the ability to employ transcellular (directly through an endothelial cell) and paracellular (between endothelial cells)
routes of transmigration. However, leukocytes invade the subendothelial space typically with a single lamellipodial leading edge and complete the entire
transmigration process in several minutes, while MSC initially spread beneath the endothelium in a starburst fashion with multiple leading fronts and
require one to two hours to completely transmigrate.
77
While technical improvements in imaging may partly account for why diapedesis was observed
for the first time in the current study, it is also likely that the quality of endothelial monolayers
used affects the fraction of diapedesis versus integration events observed. Although endothelial
monolayers cultured in vitro are generally regarded to be an acceptable model for endothelium,
many aspects of physiologic endothelium that promote junctional stability are absent or aberrant
in vitro (264). For example, endothelium is usually plated on non-physiologically rigid substrates
in vitro, which inclines them toward a hypercontractile phenotype (265) that is prone to
intercellular gap formation and retraction (266), (267). Other physiologic barrier-promoting or
'anti-contractility' stimuli, such as steady-state laminar fluid shear flow, contacts with mural cells
(e.g., pericytes) and exposure to circulating sphingosine-1 phosphate are also absent in most in
vitro models. Thus, in vitro endothelia seem significantly biased toward less stable and more
contractile phenotypes that may favor integration over to diapedesis. Consistent with this, we
found that when poor/unhealthy EC monolayers were used MSC integration increased, whereas
well-formed healthy monolayers exhibited less integration. Our in vitro EC model that retained
the most physiologic and robust barrier properties (i.e., GPNT) allowed for almost negligible
MSC integration. Thus, whereas we cannot rule out a role for integration as a physiologic mode
of extravasation (as shown for some metastatic tumor cells (268, 269)), our observations suggest
that it may often be overestimated in in vitro.
An important contrast between MSC and leukocyte diapedesis is that it occurred over a much
longer timeframe (30-120 min versus 3-6 min (244)) and in the absence of significant
polarization, directed lateral migration and formation of lamellipodia or invadosomes. Our
studies were performed under static conditions. A recent study showed that application of
physiologic shear flow promoted slow lateral migration on the endothelium (-20 mm over -2
hours), although the MSC similarly failed to spread or polarize and required similar durations
before spreading on the subendothelial matrix (260).
Unexpectedly, we found that MSC display extensive non-apoptotic membrane blebbing during
transmigration. Non-apoptotic blebbing is a recently appreciated behavior employed by some
embryonic and tumor cells for motility and invasion (241-243). We showed that dynamic
features of MSC blebbing was similar those described for other cells. Such blebbing has been
shown to be a response of cells to a loss of substrate adhesion (241, 242), (259). We noted that
MSC blebbing was predominant in early stages of transmigration, in which MSC were primarily
contacting endothelium and rounded, but was lost at late stages of when MSC mediated
extensive adhesions with and spread on the subendothelial matrix. Our data support the
hypothesis that relatively low avidity interaction between endothelium and MSC is permissive
for MSC blebbing, whereas the high avidity interactions that form upon contact with the
subendothelial matrix quench blebbing in favor a lamellipodial mode of migration.
Significantly, we also show here for the first time that MSC blebs can exert forces on
endothelium. Although it remains to be determined if such forces function to breach the
endothelial barrier and initiate transmigration, blebbing activity was well associated with
gap/pore formation, and the initial phase of subendothelial spreading. Thus, it is possible that
non-apoptotic blebbing by MSC may function as an alternate to the actin-rich protrusive
structures (e.g. lamellipodia, pseudopodia and invadosomes) that leukocytes employ to breach
the endothelium. Two recent in vivo (270) and in ex vivo organ culture (240) studies provide
support for the physiological relevance of this hypothesis. Specifically, MSC were found to
initiate extravasation by extending 'plasmic podia' across the endothelium (240, 270). Though
not characterized in any detail, the fact that these plasmic podia were of identical scale and
morphology as the non-apoptotic membrane blebs described herein, leads us to speculate that
these two structures are one in the same. Finally, it is interestingly, to note that tumor cell blebs
have also been observed in models of tumor extravasation, though their dynamics and functional
roles remain to be characterized (258, 271).
In summary, we have performed novel and high-resolution morphological and dynamic
characterization of MSC transmigration. In this way, we provide new insights for the cellular
processes that mediate MSC transmigration (Fig. 3.6). Specifically, we show for the first time
that in addition to integration, MSC can also transmigrate through discrete gaps and pores by
paracellular and transcellular diapedesis processes, partially similar to those used by leukocytes.
Additionally, MSC transmigration was strongly associated with non-apoptotic membrane
blebbing. This is the first demonstration, to our knowledge, of blebbing by a physiologic cell
type during diapedesis.
As discussed above, the in vitro models used in the current study are inherently limited with
respect to their ability to fully recapitulate the physiologic settings of MSC extravasation.
Additionally, our study models a generic inflammatory condition and cannot account for all of
the heterogeneity that arises in distinct tissues/vascular beds and the diverse setting for
inflammation, such as ischemic injury, tissue trauma and infection. Thus, future studies are
needed to critically evaluate and extend the current findings in diverse in vivo models.
Elucidating the mechanistic underpinning for MSC diapedesis will be critical to understand
MSC recruitment to sites of inflammation in physiological, pathological and clinical settings.
79
Bi
A
Vo
8
c
IFN-y
TNF-a and
IFN-y
TNF-o
Resting
20-
40-
60-
w0
100-
g2~;
A VA
hVCAM-1
q;
**
~
**
N
2]
hLMVEC
hLMVEC
le
4:
41.b
f
0
A3jJ
hICAM-1
Bli
.j
.4 2
IA
A
hVCAM-1
.
hCMVEC
hICAM-1
BWl
N.
N
A
rVCAM-1
rVAM1
GN
N
ICM-
IL IN
I
ILN
A
rICAM-1
z
t-11
Figure S3.1 Analysis of endothelial adhesion molecule expression and MSC senescence
(A) Flow cytometric analyses of VCAM- 1 and ICAM- 1 expression is shown for resting hLMVEC and
hCMVEC monolayers and monolayers treated with TNF-a alone, IFN-y alone, or both TNF-a and IFN-y.
Similarly, FACS analyses of rat VCAM- 1 and ICAM- 1 expression is shown for GPNT monolayers.
(B) The percentage of $-galactosidase positive (i.e. senescent) MSC were quantified for P3, P5 and P7 MSC,
and a positive control of P 13 MSC treated with etoposide (i). Asterisks indicate statistically significant
differences as assessed by a one-way ANOVA test with a Tukey post-hoc test, n=5.Two representative images
of (ii) non-senescent P3 MSC and (iii) senescent P13 MSC are shown.
A
B
Assesment of Cytotoxicity of PTX
M MSC
EM MSC,
Effect of Cytokine Pretreatment of GPNT EC
on MSC Adhesion &Transmigration
100ng/ml PTX
H202
60-
M MSC, 1mM
100-
A
40-
80
E
YN
60
C
201
V)
40-
I
AnnV
Pi
~~Ma
Ma i
fig a
C
+
l
-
Nonapoptotic
Early
apoptosis
N
E
TNF-
0., .
a -
IFN-y
-
+
-
-
+
+
Transmigrating
and Basal
MSC Only
All MSC
D
Integrin Subunit Expression on MSC
a4 (7.2R)
a4 (HP2/1)
a5
2
2
f
05
*
21q
f
I
1
0.2-
p0
0
z
TNF-a
Antia4
Anti VCAM-1
-
Late apoptosis
and necrosis
**
0.6,
0.u0.
.
1.
+
+
+
+
+
L
Blockade of MSC Adhesion to EC
0.81
0
i
%
20-
,
,
.
I
.
+
-
-
-
-
-
Kr']
I
+
+
-
-I-
-
+
-
+
I'
~I i\
j
J
.4
"I
.1 .7
Figure S3.2 Impact of PTX on MSC viability and role of cytokines, VCAM-1 and integrins MSC on
adhesion and transmigration
(A) Control MSC, MSC treated with 100 ng/ml of PTX or MSC treated with 1mM hydrogen peroxide
(H 20 2) for 2 h were stained positive for annexin V and propidium iodide (PI) and analyzed by flow
cytometry. Percentage of cells in each condition that were non-apototic (annexin V and PI negative), in early
apoptosis (annexin V positive, PI negative) and late apoptosis/necrosis (annexin V and PI positive) are shown.
Values are mean + s.e.m, n = 3. Asterisks indicate a statistically significant differences as assessed by a one-way
ANOVA test with a Tukey post-hoc test. No significant change in the frequency of apoptotic cells was
observed in PTX-treated MSC.
(B) MSC were incubated on resting, or TNF- activated and/or IFN-y activated GPNT for 60 min. Samples
were fixed, stained and imaged by fluorescent confocal microscopy. Both the total number of MSC, and the
number of MSC in only the transmigrating or basal positions were compared for all conditions. Data were
collected from at least 6 microscopic fields for each experimental condition. Values represent mean ± s.e.m.
(C) BCECF-loaded MSC were pre-treated with mIgG isotype control or blocking antibody toward a4
integrin (HP2/1) and co-incubated with either resting or TNF-ct-activated hCMVEC that were pre-treated
with sheep IgG isotype control or blocking antibody toward VCAM- 1 for 10 min followed by washing and
analysis. Results show the fluorescence signal of adherent MSC (i.e., post-wash fluorescence) as a fraction of
the total input MSC fluorescence (pre-wash fluorescence; Normalized Fluorescence). Values are mean +
s.e.m., n = 5. Asterisks indicate statistically significant differences as assessed by a one-way ANOVA test with
a Newman-Keuls post-hoc test.
(D) Representative flow cytometric analysis (from three separate stainings) of MSC expression of a4 (7.2R),
a4 (HP2/1; blocking antibody), a, p1, 32 and P5 integrin subunits is shown.
A
Bi
Ci
Cii
I
Fig. S3.3 Expression of tight and adherens junctional molecules at site of paracellular migration
(A) MSC incubated on hLMVEC for 30 min were fixed and stained for beta-catenin (blue), VE-cadherin
(red) and CD90 (MSC; green). A representative fluorescent confocal image (single z-section) of an MSC at
early-stage of paracellular transmigration is shown. Arrows highlight a discrete endothelial gap in the
endothelium and breach of the adherens junction.
(B) Samples as in A were stained for CD90 (green), VE-cadherin (red) and the tight junction marker occludin
(blue). (i) A representative fluorescent confocal image (single z-section) of an MSC in an early/mid-stage of
paracellular diapedesis through an expanded endothelial gap formed discretely at site of MSC diapedesis is
shown. (ii) An orthogonal z-stack projection of the same MSC in (i). Arrows highlight a discrete breach of the
adherens and tight junctions.
(C) Samples as in A were stained for CD90 (green), VCAM-1 (red) and tight junction marker JAM-1 (red). A
(i) confocal projection and (ii) orthogonal z-stack projection of a representative MSC in the process of
paracellular transmigration is shown. Note that JAM-1 is note restricted to th junctions as previously
described 27 and that it shows co-enrichment with VCAM-1 the transmigratory cup structure (ii, white
arrowheads) that surrounds the MSC. Scale bars represent 20 pm.
3.7 SUPPLEMENTAL VIDEOS
Video 3.1 MSC induce transmigratory cup formation on endothelial surface
Video depicts an MSC interacting with TNF-ca activated hLMVEC and corresponds to Fig.
3.2B. Samples were stained for CD90 (green, top left panel), VCAM-1 (red, top right panel),
and actin (blue, bottom left; merge of all three channels shown in lower right panel), imaged by
serial section confocal microscopy and rendered as a series of 3D projections rotated
progressively about the y axis for a total of 3600. Note the formation of a cup-like structure
formed by VCAM- 1 enriched finger-like projections, which extend from the apical surface of the
endothelium up the side of, and seemingly embracing, the MSC.
Video 3.2 MSC transmigrate across the endothelium in the absence of lateral migration
Video depicts dynamic live-cell DIC (right and left panels) and fluorescence (middle and left
panels, red) imaging of six MSC on memDsRed-transfected, TNF-u activated hLMVEC and
corresponds to Fig. 3.3B. Numbers in first video frame identify 6 separate MSC. MSC #1 and
#2 are in the process of paracellular and transcellular diapedesis, respectively. Note that for MSC
#2 the transmigration pore gradually expands from -1 mm to nearly 20 mm (see red channel) as
it progressively spreads its membrane in the subendothelial space in a starburst-like pattern as
seen in the DIC channel (see outline in paused frame at 20:31 time point). MSC #3-6 are
apically adherent and have not yet initiated transmigration. Notably, these cells do not display
any significant spreading, polarization or net lateral migration over a 45 minute duration.
However, these do exhibit sporadic 'jerky' motions that seem to correlate with bursts of bleb-like
protrusions against the endothelial surface (e.g. orange arrow in paused frame 15:31; see also
Videos 3-5). Scale bar represents 20 pm.
Video 3.3 MSC exhibit multiple actin-negative and actin positive blebs on their surface
Movie depicts serial confocal section (played in series) of a MSC initiating transcellular
diapedesis across TNF-ca activated hLMVEC and corresponds to Fig. 4A. Samples were stained
for CD90 (green, top left panel), VCAM-1 (red, top right panel), and actin (blue, bottom left;
merge of all three channels shown in lower right panel). Note multiple highly rounded, bleb-like
structures (green; one to several mm in diameter) can be seen protruding from the MCS surface,
which are both negative and positive for cortical F-actin (blue, see merged panel, bottom, right).
Also note that, in addition to blebs on relatively more apical surfaces, blebs can clearly be seen at
the MSC-EC interface, including at and just beneath the transcellular pore (green arrows).
Video 3.4 MSC exhibit similar blebbing and absence of lateral migration on resting and
activated endothelium
Left and right panel shows time-lapse DIC imaging of MSC added to resting and TNF-u
activated hCMVEC, respectively. No significant difference in blebbing or lateral migration of
the MSC is evident. Scale bar represents 50 pm.
Video 3.5 MSC blebbing may facilitate transendothelial migration
Forceful membrane blebbing is associated with early stages of MSC adherence, transendothelial
gap/pore formation, and subendothelial spreading as shown in a mosaic movie composed of 5
example videos representing progressive phases in the transmigration process.
Example 1: An MSC apically adherent to hCMVEC imaged by high spatial and temporal (10
frames/minute) DIC imaging. Repetitive cycles of large (1 to nearly 10 mm) blebs formation and
retraction over all surfaced of the MSC are seen. Individual blebs protruded rapidly, reaching
their maximum diameter within an average of 18 seconds and then somewhat more slowly
(average duration of retraction phase of 51 s).
Example 2: An MSC (DIC, left panel) apically adherent to a memRFP-transfected hCMVEC
(red; third panel from left). Note that a large pre-existing paracellular gap is present near, but
independent of, the MSC). Interference-contrast reflection microscopy (IRM) is shown in the
second panel from the left. IRM reports regions of extremely close contact between cells (i.e., the
endothelium) with the underling substrate (i.e., the coverglass) as darkened regions. It was
observed that as the MSC formed bleb protrusions against the apical surface of the endothelium
dynamic dark spots (with bleb-like spatial and temporal scale) in IRM (e.g., see yellow dashed
line in paused frame 1:57). See additional example in Fig. 3.5B. This provides evidence that
MSC blebs can exert a force on the endothelium sufficient to locally drive it into closer contact
with the underlying basal substrate.
Example 3: An MSC (DIC, left panel) apically adherent near the intercellular junction (see faint
vertical line of enriched red fluorescence) of two adjacent memRFP-transfected hCMVECs (red).
Note that blebbing activity is associated with initial formation of small paracellular gaps.
Example 4: An MSC (DIC, left panel) apically adherent near an activated GPNT EC
intercellular junction formed between a positive memRFP transfected (red signaling in middle
panel) and neighboring non-transfected GPNT ECs (black areas in middle panel) in a confluent
monolayer. Note that in this example blebs seem to drive a dramatic expansion of a paracellular
gap that becomes further distorted and expanded as the MSC begins to migrate further into the
subendothelial space. See also Fig. 3.5C.
Example 5: An MSC (DIC, left panel) in late stages of transcellular diapedesis across memYFPtransfected hLMVEC. Over the course of the video MSC progresses from a state of being -50%
below the endothelium, to being nearly completely spread in the subendothelial space (though
the pore has not yet closed over the MSG). Critically, this transition is associated with extensive
and dynamic membrane blebbing activity both in the apical and subendothelial portions of the
MCS. It is noteworthy, that these blebs clearly exert force against the endothelium as evidenced
by the induced distortion of the endothelial membrane (green). Indeed, subendothelial blebs
protrusion is seen to give rise to transient bright green rings as the push against the basal surface
of the endothelium. During the final -10 min of the video, blebbing gradually ceases as the
MSC transition to spreading radially in a more lamellipodia-like fashion. Scale bar represents 10
pm. See also Fig. 3.5D.
Video 3.6 Blebbing is specific to MSC interactions with endothelium
Movie consists of two distinct segments. In the first segment GFP-actin-transfected MSC were
settled on fibronectin-coated glass. DIC is shown in top and bottom panels. GFP (green) is
shown in middle and bottom panels. Note that on this substrate MSC display a combination of
86
filopodia and lamellipodia membrane extensions. Although the MSC on the right initially
demonstrates some blebbing activity, it quickly switches to the lamellipodial-mediated spreading.
In the second segment aortic adventitial fibroblasts have been added to the surface of activated
hCMVEC. Note that these cells do not display blebbing activity on endothelium but rather
undergo gradual spreading that is coupled to filopodia- or microspike-like membrane
protrusions. Scale bars represent 50 pm.
Video 3.7 MSC exhibit canonical non-apoptotic migratory blebbing dynamics
Movie depicts dynamic live-cell DIC (left and right panels) and fluorescence (green, middle and
right panels) imaging of an actin-GFP-transfected (green) MSC transmigrating through TNF-u
activated hLMVEC and corresponds to Fig. 3.3.
5G. The shown example is of a relatively late stage diapedesis event in which the MCS is
advancing part of its membrane under the endothelium. Note that MSC blebs can be seen (via
the DIC imaging) protruding from the MSC that are initially are negative for GFP-actin (green),
into which GFP-actin is subsequently recruited followed by the bleb finally retraction in a
fashion identical to cycles exhibited by some tumor and embryonic cell undergoing nonapoptotic migratory blebbing. These cycles of membrane protrusion and retraction seem to be
coupled to the overall advancement of the MSC laterally (migrating from bottom to top in the
video frame) under the endothelium. Scale bar represents 10 pm.
87
CHAPTER FOUR
AN INTRAVITAL STUDY OF MESENCHYMAL STEM CELL TRAFFICKING IN A
MURINE MODEL OF DERMAL INFLAMMATION
4.1 PREFACE
Early events of MSC adhesion to and transmigration through the vascular wall following
systemic infusion are important for MSC trafficking to sites of inflammation, yet are poorly
characterized in vivo. In this study, we used intravital confocal imaging to determine the acute
extravasation kinetics and distribution of culture-expanded MSC (2-6 hours post-infusion) in a
murine model of dermal inflammation. By 2 h post-infusion, among the MSC that arrested
within the inflamed ear dermis, 47.8±8.2% of MSC had either initiated or completed
transmigration into the extravascular space. Arrested and transmigrating MSC were rarely
observed in arterioles, but rather were found equally distributed within small capillaries and
larger venules. This suggested existence of an active adhesion mechanism (as apposed to simple
mechanical trapping), since the venule diameters were greater than those of the MSC.
Heterotypic intravascular interactions between distinct blood cell types have been reported to
facilitate the arrest and extravasation of leukocytes and circulating tumor cells. We found that
the distribution of MSC and leukocytes/platelets were correlated in the inflamed ear. Indeed,
42.8±24.8% of intravascular MSC were in contact with neutrophil-platelet clusters. A role for
platelets in MSC trafficking was confirmed by platelet depletion, which significantly reduced the
preferential homing of MSC to the inflamed ear, though the total percentage of MSC in contact
with neutrophils was maintained. Interestingly, although platelet depletion increased vascular
permeability in the inflamed ear, there was decreased MSC accumulation. This suggests that
increased vascular permeability is not necessary for MSC trafficking to inflamed sites as
previously proposed. These findings represent the first glimpse into MSC extravasation kinetics
and microvascular distribution in vivo, and further clarify the roles of passive trapping versus
active adhesion, and the roles of the intravascular cellular environment and vascular permeability
in MSC trafficking.
4.2 INTRODUCTION
The therapeutic potential of systemically infused mesenchymal stem/stromal cells (MSC) has
been associated with their ability to accumulate at sites of inflammation. This ability is also being
exploited as a cellular drug delivery system for multiple applications(272). Unfortunately, efforts
to increase MSC homing to sites of inflammation have been limited by a poor understanding of
their mechanism of trafficking(235, 273, 274).
Several studies have indicated that increased MSC accumulation at a site of inflammation is
associated with enhanced therapeutic benefit. In a model of myocardial infarction, augmenting
MSC adhesiveness (by eliminating reactive oxygen species) increased MSC engraftment in the
heart 3 days after transplantation, and was associated with improved therapeutic outcome(70).
Similarly, in another study, MSC therapeutic effect in a model of Sjbgren disease was reduced
after CXCR4 blockade, which decreased MSC engraftment in the salivary gland(71). Hence,
efforts are being made to enhance MSC therapeutic effect by increasing MSC trafficking to
target tissues, such as increasing MSC expression of adhesion molecules that bind to
endothelium(144, 245, 261, 275).
Our current understanding of MSC trafficking behavior mostly derives from in vitro studies,
based on the classical model of leukocyte homing(235, 276, 277), which emphasizes interactions
with endothelium. The leukocyte model comprises tethering, rolling, and firm adhesion on
activated endothelium, followed by transmigration across the endothelium, These events are
mediated by complementary receptor-ligand pairs on the leukocytes and endothelium(172).
MSC have been reported to roll, adhere and transmigrate on endothelium in vitro(94, 153, 184,
255, 278, 279). Though MSC exhibit heterogeneous receptor expression(278), integrins and
chemokines/chemokine receptors have been reported to influence MSC adhesion and
transmigration(153, 255, 279).
However, MSC trafficking in vivo likely depends on additional factors besides MSC-endothelial
interactions. Firstly, trapping of MSC in vessels of smaller diameter, as opposed to specific
adhesive mechanisms, may partially account for the intravascular arrest of MSC. Secondly, the
intravascular environment of sites of inflammation comprises non-endothelial cell types. In
particular, platelets and leukocytes at sites of inflammation can act as a bridge between
circulating cells and endothelium( 119). Thirdly, vascular permeability, which increases at sites of
inflammation, has been proposed to facilitate MSC transmigration and accumulation(235).
Furthermore, the kinetics of MSC adhesion and extravasation at sites of inflammation is
unknown. This is important for some MSC therapeutic strategies (e.g. targeted drug
delivery(72)), which may be most beneficial when MSC have extravasated into interstitial tissue,
instead of being adhered intravascularly in the circulation. Critically, the quantitative analysis of
the acute events following MSC infusion and prior to their extravasation has not been
performed.
In this study, we used high-resolution intravital confocal microscopy to examine the adhesion
and transmigration of MSC in a murine model of LPS-induced dermal inflammation. We
observed that about half of MSC that arrest at the inflamed ear are extravascular by 6 h postinfusion. Further, MSC were equally distributed between capillaries and venules. Since MSC
diameter (10-20tm) was smaller than venule diameters (>20ptm), this indicated that trapping is
not the only potential mechanism of MSC arrest in the inflamed ear. Notably, there was a strong
association between the spatial distribution of MSC and leukocytes/platelets at the site of
inflammation, and >40% of intravascular MSC were in contact with both neutrophils and
89
platelets. Though platelet depletion significantly decreased the preferential trafficking of MSC to
the inflamed ear, the extravasation rate of MSC and percentage of MSC in contact with
neutrophils was unaffected. This suggests that platelets impact MSC arrest intravascularly, but
not the mechanism mediating MSC contact with neutrophils following arrest. Finally, vascular
permeability was increased following platelet depletion. Since preferential accumulation of MSC
in the inflamed ear decreased after platelet depletion, this suggests that increased vascular
permeability alone does not facilitate MSC extravasation or accumulation at sites of
inflammation.
4.3 MATERIALS AND METHODS
4.3.1
MSC culture
Primary human MSC were obtained isolated from the iliac crest of the hip bone of
healthy consenting donors from the Texas A&M Health Science Center, College of
Medicine, Institute for Regenerative Medicine at Scott & White Hospital (Temple, TX).
Donors were normal, healthy adults, at least 18 years of age, with a normal body mass
index and free of infectious diseases (as determined by blood sample screening performed
1 week before bone marrow donation). In these studies, MSC from three different
donors (Donor numbers 7081, 7083, 8004) were used. MSC were maintained in
StemPro MSC serum free media (Invitrogen, Carlsbad, CA), at 37*C, 5% C02, and
media were changed every 2-3 days. Cells were cultured to 90% confluence before
passaging. MSC between passages 3-6 were used.
4.3.2
Murine model of dermal inflammation
All animals were used in accordance with NIH guidelines for care and use of animals
under approval of the Institutional Animal Care and Use Committee of Massachusetts
General Hospital and Harvard Medical School. C57/B16 wild-type mice (Charles River
Laboratories) were used for all in vivo studies. Immediately prior to LPS injection, mice
were anesthetized with an intraperitoneal injection of 2 0-30pl of ketamine/xylazine
solution. Lipopolysaccharide (LPS) from Escherichia coli (Sigma-Aldrich, St. Louis,
MO) was reconstituted in saline to make a 10mg/ml stock solution. The stock solution
was diluted in saline to make a working solution of 1mg/ml, and 30ptl of the working
solution was injected beneath the dermis of the left ear of mice. 30p1 of saline was
injected beneath the dermis of the control, contralateral ear. Mice were used 24 h
following LPS and saline injection.
4.3.3
Platelet depletion
To deplete platelets from mice prior to MSC infusion, animals were weighed and
injected with 2mg/kg of polyclonal anti-GPIb3 antibody, unconjugated (Emfret
Analytics, Eibelstadt, Germany). Control animals were weighed and injected with
2mg/kg of polyclonal non-immune rat immunoglobulins (Emfret Analytics, Eibelstadt,
90
Germany). The platelet-depleting and control antibodies were injected
infusion.
4.3.4
1h prior to MSC
Preparation of MSC for systemic infusion
Prior to infusion, MSC were trypsinized with 0.05% Trypsin/EDTA, and resuspended
in 1 OpM DiI, DiO, DiD or DiR solutions. MSC solutions were incubated for 15 min at
room temperature in the dark, then washed twice in 1 Oml PBS before being resuspended
at 200,000 or 500,000 cells/100pl. In kinetics experiments, 3 differently labeled groups
of 200,000 MSC were injected retro-orbitally 6 h, 4 h and 2 h before imaging (i.e. a total
of 600,000 MSC were injected). In experiments determining the MSC association with
neutrophils and platelets, 500,000 MSC were injected 3 h prior to imaging. In all other
experiments involving MSC visualization, 500,000 MSC were injected 6 h prior to
imaging.
4.3.5
Visualization of endogenous vasculature and cells in the murine ear
To visualize the vasculature of the murine ear, 50pl of a 10mg/ml FITC-conjugated
dextran (MW = 2,000,000) solution or 50p1 of a 2mg/ml Rhodamine-conjugated
dextran (MW = 70,000) solution was injected retro-orbitally into mice 15 min prior to
imaging. To visualize immune cells in the murine ear, 2 0pl of a 0.5mg/ml
Rhodamine6G solution was injected retro-orbitally into mice 15 min prior to imaging.
To visualize neutrophils at the site of inflammation, 1 Opg of an anti-Ly6G antibody,
clone 1A8, conjugated to AlexaFluor555 or AlexaFluor647 was injected retro-orbitally
into mice 15 min prior to imaging.
To visualize platelets at the site of inflammation, 5ptg of an anti-GPIb antibody
conjugated to DyLight649 (Emfret Analytics, Eibelstadt, Germany) was injected retroorbitally into mice 15 min prior to imaging.
4.3.6
Intravital imaging
Mice were anesthetized with isoflurane throughout the imaging procedure. Cells and
vasculature in the mouse ear were imaged non-invasively (in real time) using a custom
built video-rate laser-scanning confocal microscope designed specifically for live animal
imaging(280) using a 60x water-immersion objective. Acquired images were averages of
10 frames. Microscopic fields were typically 474x488ptm for quantifying the number of
MSC in the LPS or saline treated ear. In experiments to determine MSC association with
neutrophils and platelets, 2x and 3.2x zoom was employed, resulting in smaller
microscopic fields but greater pixel resolution.
91
4.3.7
In vivo MSC trafficking experiments
In most experiments, MSC were infused retro-orbitally into mice 24 h following LPS
and saline treatment of the mouse ears. Mice were then imaged at various timepoints
after MSC infusion (up to 24 h post-infusion). In kinetics experiments, MSC were
labeled with either DiI, DiD or DiR, and infused 2h apart. Imaging was performed 2h
after the third group of MSC had been infused. In time-lapse imaging experiments,
imaging was performed between 4 h and 6 h post-MSC infusion. Fields containing
intravascular MSC were chosen and imaged every 5 minutes. In leukocyte-MSC
correlation experiments, imaging was performed 6 h post-MSC infusion. In experiments
determining MSC association with neutrophils and platelets, imaging was performed 3 h
post-MSC infusion. In platelet depletion experiments, platelet-depleting antibodies were
infused 1 h prior to MSC infusion. Imaging was performed 6 h and 24 h post-MSC
infusion.
To quantify the number of MSC and immune cells (leukocytes and platelets)
accumulating in the ear, 20 random microscopic fields of 4 74 x4889m were imaged in
the region of LPS and saline injection in each experiment. To quantify the number of
MSC in contact with neutrophils or platelets in the ear, at least 30 random MSC were
imaged in each experiment.
4.3.8
Image analysis
Image analysis was performed using the open source software ImageJ and VAA3D
(www.vaa3d.org). ImageJ was used for cell enumeration and measurement of vessel
diameters. VAA3D was used to perform three-dimensional reconstructions of confocal
image stacks to classify MSC positions as being (i) intravascular (completely within a
vessel), (ii) transmigrating (partly within and partly outside a vessel) or (iii) extravascular
(completely outside a vessel), and to determine which vessels they were associated with.
4.3.9
Permeability assays
To assess vascular permeability in mouse ears, anesthetized mice were infused with 2001
of Evans Blue (Sigma-Aldrich, St. Louis, MO) via the inferior vena cava. 30 min later, a
needle was inserted into the right ventricle of the mouse, and the vasculature of the
mouse was flushed with 20ml of an ice-cold solution of 10OU/ml heparin (SigmaAldrich, St. Louis, MO) in phosphate buffered saline. The region of LPS or saline
injections in the mouse ears were isolated and minced. The tissue was then weighed and
incubated in a volume of formamide (Sigma-Aldrich, St. Louis, MO) proportional to the
mass of the tissue overnight at 56'C to extract Evans Blue. The amount of Evans Blue
was then measured, by measuring the absorbance of the formamide containing the tissue
at 620nm using a UV spectrophotometer.
92
4.3.10 Isolation of neutrophils
4ml of whole blood was drawn from healthy consenting donors into Vacutainers
containing K2EDTA as anticoagulant (Becton-Dickinson, Franklin Lakes, NJ). Blood
was carefully added on top of a prepared Percoll gradient at room temperature,
consisting of a bottom layer of 4ml 75% Percoll, and a top layer of 4ml 62% Percoll.
75% Percoll comprised 3.75 ml Percoll, added to 0.75 ml sterile water and 0.5 ml 10x
PBS; 62% Percoll comprised 3.1 ml Percoll, added to 1.4 ml sterile water and 0.5 ml 10x
4 0
PBS. The gradient was spun at 2 0 0 g for 25 min, then 0 g for 15 min. The neutrophil
band was then carefully isolated and transferred to a separate tube, and washed once
using HBSS-/-. The neutrophil pellet was resuspended at the desired concentration in
HBSS with 1% HEPES and 0.1% human serum albumin.
4.3.11 In vitro neutrophil extracellular trap (NET) adhesion assay and imaging
Neutrophils were suspended in 1:100 DiD solutions for 15 min at room temperature in
the dark. After being washed in HBSS-/- once, neutrophils were plated on 12mm glass
cover slips in a 24 well plate. NETs were generated in vitro by treating neutrophils with
0
phorbol 12-myristate 13-acetate (PMA), and incubating at 37 C for 4 hours. We then
incubated Dil-labeled MSC for 5 min with the NETs, and removed non-adherent MSC,
before imaging them with both epi-fluorescence and confocal microscopy(3).
4.3.12 In vivo NET detection
Sytox Green (5pM) was systemically infused into mice 24h after LPS- and saline
treatment, and 15 min before ears were imaged.
4.3.13 Statistical analysis
For comparisons between 2 groups, Student's t tests were used. Comparisons between
multiple groups (>2) were performed with one-way analysis of variance with Tukey's
post-hoc test, or with two-way analysis of variance with Bonferroni's post-hoc test.
Pearson analysis was used to test for correlations. Results were presented as mean ±
standard deviation for n>3. Asterisks indicate statistically significant differences of
p<0.05 (*), p<0.01 (**) and p<0.001 (***).
93
4.4 RESULTS
4.4.1
MSC arrest and extravasate within 2 hours post-infusion in both capillaries and venules
The kinetics of systemically infused MSC arrest and extravasation at sites of
inflammation have not been explored. Thus, we designed studies to infuse fluorescent
MSC and image their recruitment to inflamed skin at time points of 0.5, 2, 4 and 6 h
post-infusion by intravital confocal microscopy. Our preliminary experiment showed
that few MSC were evident in the inflamed skin 0.5 h following infusion, but significant
quantities of MSC accumulated by 2 h (not shown). We therefore focused subsequent
quantitation and analyses on the 2, 4 and 6 h time points. First, we determined the
location of MSC with respect to the blood vessel wall (delineated by circulating
fluorescent dextran) through serial-section 3-dimensional imaging. MSC were thus
classified as being (i) arrested intravascularly, (ii) transmigrating (i.e., spanning both
intra- and extra-vascular space) or (iii) in the extravascular space (Fig. 4.1A and Video
4.1-4.3) and quantified the fraction of each class at 2, 4 and 6 hours post-infusion (Fig
4.1B). By 2h post-infusion, 47.8±8.2% of MSC were observed transmigrating or
extravasated. The percentage of extravasated MSC doubled from 22.2±2.1% at 2 h, to
43.9±6.5% at 6 h.
Through time-lapse imaging, we also observed extravasation time for an individual MSC
to be as short as 15 min (Fig. S4.1A). Interestingly, this is -3 times shorter than what we
observed previously for MSC in vitro (279). Further, the MSC extravasation time is
about 3-5 times longer than for leukocytes, but similar to what has been observed for
tumor cells in an in vitro microvascular network platform(28 1).
We next examined the type of vessels that support MSC arrest and extravasation.
Leukocytes preferentially arrest and extravasate in venules, which are larger than
capillaries yet have higher levels of adhesion molecule expression and greater permeability
compared to capillaries and arterioles(97). Since MSC do not express many adhesion
molecules employed by leukocytes during homing, they have been proposed to arrest in
capillaries as a result of their large size (typically 10-20um in diameter in
suspension) (87).
A
B
80
**
**
60
*M intravascular
80
C
EM Transmigrating
Extravascular
20-
-s.
6
400
8
40o
0
20
0_"_
0."
Figure 4.1 Extravasation kinetics and distribution of MSC in the inflamed ear
Systemically infused MSC (green) were imaged 2, 4 and 6 h post-infusion in the inflamed ear using intravital
confocal microscopy. Blood vessels (red) were visualized using fluorescent dextrans. (A): MSC were classified
according to intravascular, transmigrating and extravascular positions. Representative images of MSC in each
position are shown as z-projections and orthogonal projections. (B): The percentages of MSC in each position
at different time points post-infusion were quantified. Two-way ANOVA with Bonferroni's post-hoc test was
used (n=4). (C): The percentages of MSC associated with capillaries (vessel diameter <20pm), arterioles and
venules were quantified (n=4 ). Arterioles and venules were differentiated based on blood flow rate and
tortuosity of vessels. One-way ANOVA with Tukey's post-hoc test was used (n=4). Values are mean±SD.
Asterisks represent p<0.05(*), p<0.01(**) and p<0.001(***); n.s. = not significant.
We quantified the fraction of MSC associated with vessels <20ptm or 20pim in diameter
in the inflamed ear. Further, the larger vessels ( 20prm in diameter) were identified as
arterioles or venules based on morphology, and blood flow direction and speed. To note,
the smaller vessels (<20pm in diameter) include capillaries and possibly also postcapillary venules. The use of permeability measurements(101, 102) and adhesion
molecule expression(97) is required to properly differentiate between capillaries and postcapillary venules (observed to be as small as 8-14gm(282), and as large as 20-40ptm(99,
283)). However, since our goal was to determine the potential for MSC trapping in
smaller vessels versus their adhesion in larger vessels, we chose 20pm, the upper limit of
MSC diameter, as the cut-off between smaller and larger vessels. The smaller vessels
(<20pm in diameter) are henceforth referred to as capillaries for convenience.
Interestingly, MSC were rarely found associated with arterioles but equally distributed
between capillaries and venules, (Fig. 4.1 C). The significant portion of MSC observed to
be associated with venules of diameters greater than that of MSC, strongly suggested that
an active adhesive mechanism exists between the MSC and blood vessel wall (Fig S4. 1B).
Despite the equal distribution of cells in capillaries and venules, we also found that there
were significantly more transmigrating and extravascular MSC associated with capillaries
than in venules (Fig. S4. 1 C). (Extravascular MSC were not included in the analysis when
the vessel they were associated with was not obvious.) This is similar to tumor cells,
which preferentially extravasate in smaller versus larger vessels in an in vitro
microvascular network platform (281).
4.4.2
MSC and leukocytes exhibit a similar distribution in the inflamed ear
The presence of MSC in venules of diameter larger than the MSC further supported the
possibility that a subset of MSC might arrest at the site of inflammation through secondary
interactions with leukocytes, which preferentially arrest and extravasate in venules(97). To
elucidate if a relationship exists between MSC and leukocyte homing to sites of inflammation, we
labeled endogenous, intravascular leukocytes and platelets in the mouse with Rhodamine 6G
(R6G; Fig. 4.2A). As expected, most Rhodamine6G+ cells arrested in venules, with fewer in
capillaries and arterioles (Supp. Fig 2A). We further observed that fields with many R6G-positive
cells often had many MSC as well. Indeed, when we plotted the number of MSC against the
number of arrested intravascular R6G+ cells in each 4 74x488im microscopic field, there was
consistently a strong correlation (Fig. 4.2B and Fig. S4.2B; R2 ranged from 0.700-0.924).
Further, to determine if there was a physical association between MSC and leukocytes/platelets,
we quantified the percentage of MSC and R6G+ cells in contact with each other (Fig. 4.2A). In
this manner, we found that 39.5±20.1% of MSC were in contact with leukocytes/platelets across
all vessels, with a greater percentage in vessels of diameter >20 ptm compared to smaller vessels
(Fig. 4.2C; p=0.218). This latter observation is likely because leukocytes were more commonly
found in venules.
Ai
All
Bli
Bi
-800
=
R2=0.800 (***)
60-
*
.
R2 =O.924
0
0
C
*
56
80-
C.)
o
20-
6
~0
6
-
10
Z
15
20
V
0
25
10
No. of MSC
20
30
40
40
60
No. of MSC
80
No. of MSC
0
200"
30
2
C 150-
A
0
20-
~~:s
5
Bill 0+
(***)
R
=O.812
(***)
0
20
E
0
'
.~.
50-
0
0
UC
e0,>
6
z
0i
0
20
40
60
80
0
No. of MSC
20
80
70
o
60
t
50
L8 40
- 30
20
10
0
ITI
- All vessels
*<20pm vessels
" Post-capillary
venules
Figure 4.2 MSC and leukocyte distribution in the inflamed ear is correlated
Systemically infused MSC (blue) were imaged 6 h post-infusion in the inflamed ear using intravital confocal
microscopy. Blood vessels (red) were visualized using fluorescent dextrans, and endogenous intravascular
leukocytes and platelets were visualized using Rhodamine 6G (green). (A): MSC were often observed in
proximity to Rhodamine6G+ cells, and could be classified as being in contact or not in contact with
Rhodamine6G+ cells. Insets (white boxes) in Ai and Aui show representative images of MSC (white
arrowheads) not in contact or in contact with Rhodamine6G+ cells respectively. See also Supp. Fig. 2A. (B):
The numbers of MSC and Rhodamine6G+ cells found in each microscopic field were quantified for at least
15 microscopic field in each of 4 independent experiments. The numbers of MSC and Rhodamine6G+ cells
for each field were plotted against each other. Pearson's correlation was used. (C): The percentages of MSC
interacting with leukocytes in all vessels, only capillaries (vessel diameter <20gm) and only venules were
quantified. One-way ANOVA with Tukey's post-hoc test was used (n=4). Values are mean±SD. Asterisks
represent p<0.05(*), p<0.01(**) and p<0.001(***); n.s. = not significant.
Three possibilities might account for the strong correlation between MSC and
leukocyte/platelet distribution. First, related signals regulate both MSC and
leukocyte/platelet accumulation in the inflamed ear. Second, leukocytes/platelet facilitate
MSC accumulation in the inflamed ear. Third, MSC facilitate leukocyte/platelet
accumulation in the inflamed ear. Based on our observations that the majority of MSC
were apparently in direct contact with leukocytes/platelets and that there were many
localized leukocytes not in contact with MSC, we decided to explore the second
possibility.
4.4.3
MSC are found in contact with, or in close proximity to, neutrophil-platelet clusters
To facilitate our investigation of the role of leukocytes/platelets in facilitating MSC
homing, we decided to focus specifically on neutrophils and platelets.
We chose these two circulating cell types for several reasons. First, neutrophils and
platelets are typically the first responders during acute inflammation, and are found
abundantly at the site of inflammation(284). Second, platelets have previously been
implicated in MSC accumulation at sites of inflammation(93, 94). Third, we observed
intravascular neutrophil-platelet clusters to exist at baseline (i.e. LPS-induced
inflammation without MSC infusion) using antibodies toward the neutrophil-specific
Ly6G antigen and platelet-specific GPI lb antigen (Fig. 4.3A).
When we systemically infused MSC, we found 42.8±24.8% of intravascular MSC in
contact with these neutrophil-platelet clusters (Fig. 4.3B and Fig. 4.5A). Of the
remaining intravascular MSC, 15.0±6.8% were found with platelets only (Fig. 4.3C),
4.36±2.70% were found in association with neutrophils only (Fig. 4.3D), and the
remaining 37.8±25.3% were neither in contact with neutrophils nor platelets (Fig. 4.3E).
We also frequently observed lone MSC near, but not in contact with the neutrophilplatelet clusters (Fig. 4.3Eii,iii). The percentage of MSC found in contact with
neutrophils here (47.2±26.5%) is similar to the percentage of MSC previously found in
contact with R6G+ cells (39.5±20.1%).
MSC-Platelet-Neutronhil
MSC-Platelet
MSC only
'Adhered'in
venule
Ei
MSC-NeutroDhil
r
'Adhered' near neutrophil-platelet clusters
ii
Me
iii Meg
Figure 4.3 Large fraction of intravascular MSC found in contact with neutrophils and platelets
Systemically infused MSC (green) were imaged 3 h post-infusion in the inflamed ear using intravital confocal microscopy. Endogenous, intravascular
neutrophils (N; blue) and platelets (P; red) were labeled using antibodies toward murine Ly6G and murine GPI1b, respectively. Blood vessels were
visualized using fluorescent dextrans (red in A, white in all other panels). (A): Representative images of intravascular P-N clusters (white arrowheads)
found in the inflamed ear at baseline, without MSC infusion. (B-D): Representative images of intravascular MSC found in contact with P-N clusters
(B). with P only (C). or with N only (D. (E): Renresentative imapes of intravascilar MSC (white arrowheads) not in contact with P or N. could be
4.4.4
Platelet depletion decreases MSC trafficking to the inflamed ear
Since more than half of intravascular MSC were associated with platelets, we quantified
MSC trafficking to the inflamed ear following platelet depletion. Preferential MSC
trafficking to the inflamed ear remained after platelet depletion at both 6h and 24h (Fig.
4.4A). To further understand how preferential MSC trafficking to the inflamed ear was
affected after platelet depletion, we compared the ratio of MSC that accumulated in the
LPS-treated ear to the control (saline-treated) ear of the same animal. We found the ratio
of MSC numbers in the LPS- versus saline-treated ears of each mouse was significantly
decreased by more than 50% at both 6h and 24h following infusion (Fig. 4.4B; At 6h,
5.29±0.63 decreased to 2.36±0.98; At 24h, 7.98±0.67 decreased to 3.67±1.31). This
suggested that platelet depletion affected a mechanism that facilitates enhanced MSC
trafficking to the inflamed ear.
We further determined that the extravasation capacity of the MSC was not affected by
platelet depletion by quantifying the percentage of MSC in the (i) intravascular, (ii)
transmigrating and (iii) extravascular position (Fig. 4.4C). There was no significant
difference between the percentage of MSC in each stage under both control and platelet
depleted conditions suggesting that platelet depletion affects events upstream of MSC
extravasation, i.e. MSC arrest. Similarly, the distribution of MSC in capillaries and
venules within the inflamed ear was not affected (Fig. 4.4D).
4.4.5
MSC-neutrophil contact following MSC arrest is independent of platelets
Since previous studies suggested that platelets could act as a bridge between circulating
tumor cells and neutrophils, we aimed to determine how platelet depletion affected MSC
contact with neutrophils. We quantified the percentages of intravascular MSC, which
were (i) not in contact with neutrophils or platelets ("MSC only"), (ii) in contact with
either platelets or neutrophils only ("MSC-P" and "MSC-N"), or (iii) in contact with
both neutrophils and platelets ("MSC-P-N") in the LPS-treated ear of control and
platelet depleted mice (Fig. 4.5A). As expected, the total percentage of MSC in contact
with platelets (MSC-P and MSC-P-N) decreased by more than seven-fold following
platelet depletion (Fig. 4.5B). Surprisingly though, the percentage of MSC in contact
with neutrophils (MSC-N and MSC-P-N) was maintained (Fig. 5C). With our findings
that platelet depletion decreased MSC accumulation in the inflamed ear, this shows that
platelets impact the number, but not percentage, of intravascular MSC in contact with
neutrophils. Hence, platelets impact MSC arrest (which may potentially be due to MSCneutrophil contact), but likely not the mechanism maintaining MSC-neutrophil contact
following arrest.
24 h
6h
*p=0.046
p 20
1
25-
6
4o. **p=0.07
C3 Saline
Ca)
Control
Control
Plateletdepleted
E Control
M Plateletdepleted
a6-
0M Control
80
S
CD
2
60
40
40
-
s
U Plateletdepleted
20
2-
100
80'
S60
0
C
0
-
0
Plateletdepleted
80
10C
**p=003
40
134
o 0
0
Saline
M LPS
15-
I
CM
p=0.140 0 LPS
C3 Control
n.
M Plateletdepleted
40
20
0;g
Figure 4.4 Platelet depletion decreased preferential trafficking of MSC to inflamed ear
To determine if platelets facilitate MSC homing, platelets were depleted prior to MSC infusion. Random
microscopic fields of both the inflamed, LPS-treated ear, and contralateral, saline-treated ear were imaged at 6
h and 24 h post-infusion, and the average numbers of MSC per field were quantified for both. (A): The
absolute number of MSC per microscopic field in the LPS-treated and saline-treated ear of both control and
platelet-depleted animals were compared. Paired student's t-test was used to compare both groups at each
time point (n=4). (B): The ratios of number of MSC in the LPS-treated ear versus the saline-treated ear were
compared for control and platelet-depleted animals. Paired student's t-test was used to compare both groups
at each time point (n=4). (C): The extravasation rate of arrested MSC in the inflamed ear was compared for
control and platelet-depleted animals, by quantifying the percentages of MSC in intravascular, transmigrating
and extravascular positions. Paired student's t-test was used to compare both groups for each position (n=4 ).
(D): The distribution of MSC between capillaries (vessel diameter <20pm) and venules in the inflamed ear at
6 h post-infusion was compared for control and platelet-depleted animals. Paired student's t-test was used to
compare both groups at each time point in A, each position in B or for each vessel type in C (n=4). Values
represent mean±SD. Asterisks represent p<0.05(*), p<0.01(**) and p<0.001(***); n.s. = not significant.
One possible indirect mechanism of MSC-neutrophil adhesion is via newly described
neutrophil extracellular traps (NETs). During certain types of inflammation and
immune reactions (including LPS-induced inflammation) neutrophils have been shown
to extrude their nuclear DNA into the extracellular environment forming an adhesive
meshwork of material, a process termed 'NETosis'(128, 129). These NETs can be found
intravascularly, where they can trap bacteria and circulating tumor cells(126, 132).
Significantly, platelet-neutrophil adhesion has been shown to be important for NET
formation(125-127), hence one would expect fewer NETs after platelet depletion, which
would potentially provide fewer sites for MSC arrest.
We indeed found that MSC adhered to thick webs of NETs in vitro (Fig. S4.3). Though
NETs typically comprise thin DNA strands not visible at the resolution of epifluorescence microscopy, their fragility causes the thin strands to coalesce into thick webs
of NETs during the washing and removal of non-adherent MSC. In certain instances, we
observed MSC solely in contact with the NETs, without any contact with neutrophils.
These MSC were suspended in bridge-like strands of NETs, strongly suggesting that that
MSC can adhere directly to NETs.
However, we did not find any evidence for the presence of NETs in our in vivo model.
We systemically infused Sytox Green, a DNA-labeling dye, into mice but found that
almost all Sytox Green-labeled structures in the LPS-treated ear were extravascular
(Video 4.1). This suggests that while MSC may be able to adhere to NETs, NETs are
not a mechanism of intravascular adhesion in our model.
4.4.6
Increased vascular permeability associated with reduced MSC trafficking
Of note, platelets are known to affect vascular permeability under both physiological and
pathological states(285-287). As it has been previously proposed that MSC arrest or
extravasation occurs as result of increased vascular permeability at sites of inflammation,
we determined if permeability changed after platelet depletion in our model. To do so,
we systemically infused Evans Blue into both control and platelet-depleted mice, and
measured the ratio of Evans Blue leakage in the LPS-treated ear versus the control ear.
Consistent with published studies, we found that platelet-depletion indeed significantly
increased vascular permeability in the inflamed mouse ears of mice, which was
surprisingly coupled to a decreased MSC accumulation in parallel (Fig. 4.6). This
strongly suggests that increased vascular permeability on its own cannot account for the
increased MSC accumulation at sites of inflammation.
A
OControl
Plateletdepleted
o08
40.
n
0
fl
of40
0
s
(D
3
P
C
~16
.0
0 a_
M)
MSC-P and MSC-P-N
B5
1001
MSC-N and MSC-P-N
p=0.07
1
C
0
0 Z
x
2
C61
0
6o
OC,
CPO
Figure 4.5 Fraction of intravascular MSC in contact with neutrophils is maintained after
platelet depletion
To determine how platelets affected MSC contact with neutrophils, we imaged at least 30
random intravascular MSC in the inflamed ear of control and platelet-depleted MSC. Platelets
(P) and neutrophils (N) were visualized using antibodies towards murine Ly6G and murine
GPIlb, respectively. (A): The percentages of MSC not found in contact with P or N ("MSC
only"), found in contact with P only ("MSC-P"), found in contact with neutrophils only
("MSC-N") and found in contact with both P and N ("MSC-N-P"), was compared for
control and platelet-depleted animals. Two-way ANOVA with Bonferroni's post-hoc test was
used (n=3). (B, C): The total percentages of MSC found in contact with P (B; sum of MSC-P
and MSC-P-N) and N (C; sum of MSC-N and MSC-P-N) were compared for control and
platelet-depleted animals. Paired student's t-test was used (n=3). Values represent mean±SD.
Asterisks represent p<0.05(*), p<0.01(**) and p<0.001(***); n.s. = not significant.
Figure 4.6 Vascular permeability in inflamed
ear increases after platelet depletion
To determine how platelet depletion affected
vascular permeability in the inflamed ear, Evans
Blue leakage in the ear was measured. The ratio
of Evans Blue absorbance in the inflamed, LPStreated ear versus the control, saline-treated ear
was compared for control and platelet-depleted
animals. Paired student's t-test was used (n=4).
Values represent mean±SD. Asterisks represent
p<0.05(*), p<0.01(**) and p<0.001(***).
4.5 DISCUSSION
In this study, we have investigated the trafficking of MSC in a model of dermal inflammation
following systemic infusion. Though the term 'MSC' is controversially used to represent
different populations of cells(4, 5), we chose to explore the trafficking of culture-expanded,
human bone marrow-derived MSC defined by standards described by the International Society
of Cellular Therapy(3). We chose this population of cells because they are widely used
experimentally and in clinical trials. Importantly, MSC defined in this way represent a highly
heterogeneous population of cells (in size, surface marker expression, differentiation potential,
clonogenicity etc.), hence it is unlikely that a single mechanism can account for the
accumulation of all MSC at sites of inflammation in vivo.
To our knowledge this is the first study that has employed in vivo confocal microscopy to
quantitatively examine the adhesion and extravasation dynamics of systemically infused MSC at
a site of inflammation. This study was performed as a follow up to our previous study where we
imaged the cellular processes mediating MSC transmigration through endothelium in
vitro(279). Unlike in vitro experiments where endothelial monolayers are a limited approximate
to the inner lining of blood vessels, here we were able to quantify the dynamics of MSC
extravasation through the vascular wall at a site of inflammation. We found that more than 20%
of MSC were extravasated as early as 2 h following infusion, and that this percentage more than
doubles by 6 h. The kinetics of extravasation is relevant to current MSC studies for several
reasons.
First, numerous studies that have examined MSC trafficking to tissues and organs focus on late
time points, typically 24 h post-infusion or later. Since MSC can adhere and extravasate much
earlier than 24 h, it is unclear if such studies are actually measuring an effect on adhesion and
extravasation capacity, or the survival of extravasated MSC within interstitial tissue.
Second, a significant debate within the MSC field is whether MSC exert their
immunosuppressive effects via a systemic or local mechanism. While this is a complex topic, a
better understanding of the timing of MSC extravasation at the site of inflammation (when they
can exert local effects) compared to the initial observation of a functional immunosuppressive
effect can be helpful to address this question. For example, in one study, the migration of
activated dendritic cells to the lymph node (a pro-inflammatory) effect, was reduced within 10
minutes of systemic infusion of MSC(67). Based on our data, it is unlikely that a local
immunosuppressive effect was exerted by MSC in this model.
Third, MSC are being explored as local drug delivery carriers due to their ability to preferentially
traffic to sites of inflammation, including tumors(72, 288, 289). An understanding of the
kinetics of MSC arrival and extravasation at the site of inflammation, versus the kinetics of drug
release by MSC will be important to avoid unwanted systemic side effects.
The majority of systemically infused MSC are sequestered in the small capillaries in the lung
immediately post-infusion, a phenomenon common to many infused cell types, including stem
Several studies have implicated adhesive interactions in
cells and neutrophils(87, 290).
mediating this sequestration. For example, a deficiency of L-selectin did not prevent lung
sequestration post-infusion, but did reduce the duration for which neutrophils were
sequestered(290). Similarly, pretreating MSC with a blocking antibody to the a4 integrin also
reduced their duration of sequestration in the lung(87). Our analysis showed that MSC were
equally distributed between capillaries and venules in the inflamed ear. Their presence in vessels
of diameter larger that that of MSC, helps to confirm the role of an active adhesive mechanism
for the arrest of at least a subset of the MSC. This is consistent with a previous study where MSC
were observed to adhere directly to the injured arterial lumen within 5 minutes of infusion in a
model of carotid artery ligation(94). The factors that determine MSC arrest in a capillary or
venule require further study. Additionally, MSC populations are known to comprise subsets of
cells with heterogeneous size(291) and surface molecule expression(154). It is conceivable that
larger MSC may arrest in capillaries, while smaller MSC with greater adhesion molecule
expression arrest in venules.
Care should be taken when extending our results to MSC distribution in other microvascular
beds, however, as blood vessels are a highly heterogenous anatomic compartment(106). Sitespecific endothelial characteristics and intravascular cell traffic likely influence the distribution of
MSC in each tissue bed. For example, we have found that significant MSC extravasation and
engraftment occurs in the calvarial bone marrow regardless of inflammation(275), while few
MSC traffic to the non-inflamed ear in our study.
Interestingly, we found that the majority of intravascular MSC could be found in contact with
platelets or neutrophils in the inflamed ear. Previously, the MSC integrin av3 3, and platelet
surface molecules P-selectin and GPIIb/IIIa, have been shown to mediate adhesion of activated
platelets, but not resting platelets, to MSC in vitro(93, 94). To note, a significant minority of
intravascular MSC (37.8±25.3%) could also be found neither in contact with platelets nor
neutrophils. Since images of each region in the inflamed ear were acquired at a single time-point,
it is difficult to tell if this subset of MSC were in contact with platelets or neutrophils at some
point during their intravascular arrest. Further, the heterogeneity of MSC raises the possibility
that different subsets of MSC have varying affinity for platelets and neutrophils, due to variable
surface marker expression.
Nonetheless, a role for platelets in MSC trafficking, for at least a subset of MSC, was confirmed
by our finding that platelet depletion decreased preferential homing of MSC to the inflamed ear.
A previous study showed that platelet depletion decreased MSC adhesion to a site of arterial
ligation(94). While endothelium is denuded to expose subendothelial extracellular matrix during
arterial ligation, in our model endothelium is intact, hence the mechanisms of MSC arrest in the
two studies are expected to be different. Furthermore, platelet depletion was initiated 16 h prior
to arterial injury and MSC infusion, which allowed an extended time for multiple downstream
inflammatory processes (e.g. levels of circulating platelet secreted factors) to be affected. To
decrease impact of platelet depletion on other inflammatory processes, we initiated platelet
depletion after induction of inflammation and just 1 h prior to MSC infusion and found that a
105
decrease in MSC adhesion was still observed. This suggests that direct MSC-platelet interactions
are responsible for MSC arrest on intact endothelium at the inflamed site.
The mechanism by which platelet depletion decreases MSC accumulation at inflamed sites is still
unclear and will be addressed in future work. Previous in vitro experiments suggest that platelets
may facilitate MSC disruption of the endothelial barrier(94). This contradicts our finding that
MSC extravasation rate is unaffected by platelet depletion. Based on our findings, platelet
depletion likely affects events upstream of MSC extravasation. These events can be categorized
into two main groups affecting: (i) The availability of MSC in the circulation, and (ii) adhesive
interactions between the MSC and endothelial wall. Platelets might affect the availability of
MSC in circulation by protecting MSC from natural killer cell lysis as previously shown for
tumor cells(91). However, it is unlikely that the availability of MSC accounted for the decrease
in MSC accumulation in our model, since not only absolute numbers of MSC, but also the
preferential accumulation of MSC in the inflamed ear were decreased.
Compared to the role of platelets in affecting MSC availability in circulation, the role for
platelets in mediating direct or indirect adhesive interactions between MSC and the endothelial
wall would seem more likely. Such a role is supported by a previous study that found that
blocking MSC-platelet adhesion via the platelet receptor, glycoprotein IIb/IIIa, decreased MSC
accumulation in a model of lung injury(93). Conceivably, intravascular platelets adhered at the
inflamed site may act as a bridge for MSC to adhere to endothelium, as has been proposed for
tumor cells( 119). Alternatively, platelet microparticles have been known to bind to
hematopoietic stem cells, and increase their engraftment(124). The role of platelet microparticles
in MSC trafficking has not been explored.
Interestingly, we found that the platelet depletion did not affect the percentage of intravascular
MSC in contact with neutrophils, although the number of MSC in contact with neutrophils
decreased. This result requires further investigation to determine if MSC-neutrophil interaction
is a result of random interactions or platelet-associated adhesive mechanisms. Minimal evidence
exists for direct MSC-neutrophil adhesion. However, MSC expression of ICAM-1 and VCAM-1
has been observed(65). Since neutrophils also adhere to endothelium at inflamed sites via
endothelial ICAM-1 and VCAM- 1 expression, it is reasonable to conceive that neutrophils
might similarly adhere to MSC. Future studies blocking neutrophil trafficking to sites of
inflammation may help to elucidate the role for neutrophils in facilitating MSC trafficking.
Another role for platelets that we considered in our experiments was their function in
maintaining endothelial permeability. Platelet depletion has been shown to both increase and
decrease endothelial permeability in different studies, in both physiological and pathological
states(285-287). This is significant as MSC trafficking to inflamed sites has been thought to be
facilitated by increased endothelial permeability, e.g. MSC may take advantage of intercellular
endothelial gaps to directly invade interstitial tissue(235). Indeed, although leukocyte
extravasation is a much better understood process, the role of endothelial permeability in
leukocyte extravasation is still controversial(103, 292-294). To our surprise, we found that the
increased endothelial permeability in our experiments (following platelet depletion) was
106
associated with decreased MSC accumulation at the site of inflammation. Furthermore, the
extravasation rate of MSC in the inflamed ear following platelet depletion was unchanged,
suggesting that MSC extravasation at inflamed sites is not dependent on endothelial gaps or
permeability. This is consistent with our previous study where we demonstrated that MSC can
transmigrate transcellularly (i.e. directly through an endothelial cell), and does not require preexisting endothelial gaps(279).
In conclusion, we have explored several factors in vivo that can influence MSC trafficking. Our
results strongly support the existence of an active adhesive mechanism for MSC arrest, for at least
a population of MSC, at the inflamed site in contrast to passive mechanical trapping in small
diameter vessels. Further, by visualizing the intravascular cellular environment of the MSC, we
found that platelets, and possibly also neutrophils, play a significant role in regulating MSC
trafficking perhaps via secondary adhesive interactions. Finally, we demonstrated that endothelial
permeability does not appear to facilitate MSC accumulation and extravasation. This advances
our knowledge of MSC trafficking, which has largely been restricted to MSC-endothelial
interactions. Due to the inherent heterogeneity of vascular beds between tissues, future studies
are needed to critically evaluate and extend the current findings for other inflammatory contexts,
e.g. sterile wounds, autoimmune diseases, in which MSC are being used as a cell therapy. A
better understanding of how MSC interact with vascular beds from different tissues will inform
strategies to engineer MSC trafficking for therapeutic purposes.
107
4.6 SUPPLEMENTAL FIGURES
MSC/Blood vessels
A
-4
B
Intravascular
Ci
IWO
nsn.s.
Transmigrating
Extravascular
100
*8o
80
6
l)
0
~601
80
6
600
20
2
0
2
0
N\
*c0
-0
**
Figure S4.1 Extravasation kinetics and distribution of MSC in the inflamed ear
Systemically infused MSC (green) were imaged 2, 4 and 6 h post-infusion in the inflamed ear using intravital
confocal microscopy. Blood vessels (red) were visualized using fluorescent dextrans. (A): The extravasation of
an individual MSC was captured using time-lapse imaging (1 confocal stack/5 min). The stack has been
rotated such that the direction of extravasation is parallel to the plane being viewed. Images shown are
projections of the stack in the region of interest (blue box). (B): MSC could be seen in capillaries of diameter
cell diameter. One of the cells (1) is intravascular, while the other cell (2) is transmigrating. (C): The
percentages of intravascular, transmigrating and extravascular MSC associated with capillaries (vessel diameter
<20ptm), arterioles and venules were quantified (n=4 ). Arterioles and venules were differentiated based on
4
blood flow rate and tortuosity of vessels. One-way ANOVA with Tukey's post-hoc test was used (n= ).
Values are mean±SD. Asterisks represent p<0. 0 5(*), p<0.01(**) and p<0.001(***); n.s. = not significant.
i
ii
Figure S4.2 MSC and leukocyte distribution in the inflamed ear is correlated
Systemically infused MSC (green) were imaged 6 h post-infusion in the inflamed ear using intravital confocal microscopy. Blood vessels (red) were
visualized using fluorescent dextrans, and endogenous intravascular leukocytes and platelets were visualized using Rhodamine 6G. (A): Representative
projections of confocal stacks acquired are shown. Intravascular densities of Rhodamine6G+ cells had a wide range (compare i to ii). Rhodamine6G+
cells were found mainly in venules (v), not arterioles (a) or capillaries (c). Non-adherent leukocytes rolling along arterioles could be seen occasionally
(white boxes). (B): The numbers of MSC and Rhodamine6G+ cells found in each microscopic field were quantified for at least 15 microscopic field in
each of 4 independent experiments. The numbers of MSC and Rhodamine6G+ cells for each field were plotted against each other. Each plot shown is
one independent experiment; see also Fig 4.2B for other plots. Pearson's correlation was used. Asterisks represent p<0.05(*), p<0.01(**) and
p<0.001(***); n.s. = not significant.
Ai
ii
B
112
Figure S4.3 MSC adhere to neutrophil extracellular traps
Neutrophils (blue) were treated with phorbol 12-myristate 13-acetate (PMA) to generate neutrophil
extracellular traps (NETs; green). MSC (red) were incubated with NETs for 5 min, and non-adherent MSC
were gently removed before imaging. (A): Representative epifluorescent inverted microscopy images of MSC
(white arrowheads) directly adhered to NETs, but not neutrophils. The effect of shear force on NETs often
formed NET 'bridges' which suspended MSC in solution. Cells in the planes below the MSC can be seen out
of focus. (B): Representative confocal image of an MSC (white arrowhead) with a strand of DNA apparently
adhered to its surface.
4.7 SUPPLEMENTAL VIDEOS
Video 4.1 Detection of NETs in the inflamed ear
Sytox Green (green) was used to detect NETs in the inflamed ear using intravital confocal
microscopy. Blood vessels (red) and neutrophils (blue) were visualized using fluorescent dextrans,
and an antibody against murine Ly6G, respectively. A representative confocal image stack is
shown. Most Sytox-Green structures seemed to be extravascular, not associated with
intravascular neutrophils.
CHAPTER FIVE
CONCLUSIONS
This thesis has made multiple contributions to the fields of MSC biology and cellular
trafficking.
First, we found that MSC are capable of transmigrating across endothelium and that this
ability is enhanced in inflammation. The ability to breach the endothelial barrier is a key
component of the trafficking process. Although MSC had previously been shown to roll on
and adhere to endothelium, the subsequent transendothelial migration step had not been
well elucidated.
Second, we found that suspended MSC displayed non-apoptotic migratory blebbing, which
could exert forces on underlying endothelium. Although blebbing is increasingly recognized
as a mode of motility, this is the first time that it had been implicated in trafficking, and
specifically, transendothelial migration.
Third, we performed the first intravital imaging study of acute MSC trafficking to a site of
inflammation following infusion. We were able to thus determine the kinetics of MSC arrest
and extravasation in vivo.
Fourth, we found significant evidence that adhesive interactions mediate MSC arrest at the
site of inflammation as opposed to simple mechanical trapping. We inferred this from
observing that about half of all arrested MSC were associated with vessels with diameters
larger than that of the MSC.
Fifth, we found significant evidence implicating platelets and neutrophils, a significant
component of the intravascular compartment at the inflamed site, in facilitating MSC
trafficking. The majority of intravascular MSC were associated with both platelets and
neutrophils, and platelet depletion significantly decreased preferential MSC trafficking to the
site of inflammation.
Sixth, we found that vascular permeability (or the existence of intercellular endothelial gaps)
cannot be the sole factor, and is unlikely a major factor, in determining the efficiency of
MSC trafficking and extravasation. An increase in relative permeability at the inflamed site
was associated with decreased MSC accumulation at the inflamed site, and did not change
MSC extravasation rate.
115
Finally, in the course of our studies, a couple of themes emerged which have implications for
future studies.
5.1 USING MICROSCOPY TO STUDY CELL TRAFFICKING
Microscopy was a key technique used in the research performed described in this thesis.
In vitro work was mainly performed with high-resolution confocal microscopy, and
dynamic live-cell imaging while in vivo work was performed with intravital confocal
microscopy.
Technical challenges in microscopy abound. Fluorescent-bound labels must be chosen
for their avidity to the cell or structure of interest, specificity, brightness and
photostability. The wavelengths used to excite the labels should preferably also avoid
inducing autofluorescence in the surroundings, and should excite other fluorescent labels
being used in parallel to a very limited extent. Optical resolution, largely determined by
the microscope parameters used for imaging, must be chosen based on the scale of the
events or structures of interest. The limited depth of tissue that can be imaged in
intravital microscopy further limits non-invasive microscopy to a subset of easily
accessible anatomical locations. For example, two-photon optical microscopy can image
up to a millimeter in depth, which is superior to most other intravital imaging
techniques(295). Long-term imaging of sites which require surgical access are often
subject to scarring and fibrosis over time, and hinder imaging while inherently modifying
the tissue environment.
Additionally, there were challenges unique to imaging adhesion and extravasation.
Firstly, capturing the relatively transient events of adhesion and extravasation in vivo
required careful timing. Since systemically infused MSC are initially trapped in the lungs
upon systemic infusion before gradually redistributing to other parts of the body,
relatively few cells are adhered and extravasating per microscopic field at the site of
infusion at any given moment post-infusion.
As a result, to quantify a sufficient number of cells to characterize their behavior, we had
to image numerous fields per animal. Hence, we were restricted in having to capture
static (as opposed to timelapse) images of each field. Thus the typical tradeoff in in vivo
imaging was between imaging suitably large numbers of cells for quantitation and
imaging information-rich, dynamic behaviors.
A general conclusion that can be drawn from the two challenges discussed above is that
microscopy is not suitable for examining dynamic events that are sparsely distributed
across numerous microscopic fields. A possible compromise is to automate the
microscope stage to capture specific microscopic fields sequentially and repeatedly.
However, this still requires that the duration of one imaging cycle (i.e. time between
imaging the first and last field of each cycle) is less than the desired duration between
consecutive images of each field.
116
A technique that enables us to track adhesion and extravasation dynamically in vivo
without requiring visual confirmation would thus be desirable. For example, this would
require a change in some signal when a cell exits the intravascular space. Or perhaps
more ambitiously, a change in some signal when a cell is actively traversing the
endothelial layer. The significant challenge regardless of the type of signal used, would be
the amplification or sensitive detection of the signal changes.
Another challenge was to understand how cells changed during flow. It is currently near
impossible to track a single cell from its site of infusion to the target site through the
circulation, and similarly difficult to determine if the population of cells that arrives at a
target site is a representative selection of the population of cells initially infused. This is a
significant challenge as understanding how cells change or are sequestered in places other
than the target site during their journey from the site of infusion to the target site would
help us to better engineer cells to arrive at their target site. Cells might change in protein
expression, size, or membrane integrity, all of which are factors influencing their ability
to traffic to the target size efficiently.
To generalize the challenge described further, it is typically difficult to image cells at
different length scales simultaneously. For example, detecting cellular features like
blebbing or podosomes requires relatively high resolution imaging, which is hard to
achieve when imaging numerous, relatively large microscopic fields to quantify sufficient
numbers of cells. One way to get around this would be capture the desired regions of the
image (e.g labeled cells) with high resolution, while capturing other regions of the image
with low resolution. However, this would require user-defined regions prior to image
acquisition, preferably through automated image segmentation to limit the time required
for imaging.
5.2 A HEMATOPOIETIC VERSUS MESENCHYMAL MODEL OF TRAFFICKING
The framework provided by the leukocyte homing cascade has predominated the field's
approach toward understanding how MSC arrive at sites of inflammation. However, we
found that MSC differed from leukocytes in multiple aspects of trafficking and
interactions with endothelium, and instead shared more characteristics with other
mesenchymal cell types. Specifically, the behavior of MSC in suspension (a model for
circulation) and on endothelium was similar to that observed for fibroblasts and
adheentcancer cells. Hence, we propose here a mesenchymal mode of trafficking (utilized
by MSC and other mesenchymal cell types) in contrast to a hematopoietic mode of
trafficking (utilized by leukocytes). These two modes of trafficking might be
differentiated in the following ways.
First, mesenchymal cell trafficking seems to be a highly inefficient process. For
exogenously infused culture-expanded MSC, less than 1% of the total infused population
eventually arrives at the inflamed site. Similarly, metastasis has long been recognized to
117
be an inefficient process. Large numbers of cancer cells are shed from the primary tumor
into the circulation, of which only a tiny percentage eventually form metastases. In
contrast, our immune system relies on leukocytes to be efficiently recruited from the
circulation within minutes of the onset of inflammation.
Second, while leukocytes are naturally adapted to circulate for prolonged durations,
mesenchymal cells are typically adherent cells and are significantly more susceptible to
anoikis. The half lives of circulating neutrophils and monocytes are 7 h(296) and 3
days(297, 298), respectively. Once released from the bone marrow, they spend most of
their lives in circulation before being cleared in the reticuloendothelial system under
physiological conditions. However, MSC and adherent cancer cell types are susceptible
to anoikis(89, 299, 300), i.e. the induction of apoptosis through loss of adhesive
contacts(301). Hence, the inefficiency of MSC and cancer cell trafficking may be
partially due to their inability to survive in the circulation.
Third, we found that MSC, like adherent cancer cells, exhibit blebbing upon loss of
adhesion and may use blebbing as a mode of motility(242, 259, 302, 303). Specifically,
we observed MSC blebbing both in suspension and on endothelium, apparently due to
MSC lack of avidity on endothelium. MSC lack many of the adhesion molecules which
leukocytes use to roll on, adhere to and laterally migrate on endothelium(144, 213, 275).
Instead of blebbing, leukocytes form actin-rich protrusive structures like lamellipodia,
invadosomes and podosomes to apparently crawl on, and probe their endothelial
environment(238). Blebbing has thus been proposed as an alternative to such structures
to probe the cellular environment when there is a minimal cell adhesion(241). Hence, it
can be expected that MSC and cancer cells that lack leukocyte adhesion molecules might
bleb in circulation and on endothelium.
Fourth, MSC and most adherent cell types have been found to cause retraction of
endothelial monolayers in vitro and integrate into the monolayers over long periods of
time (94, 239, 240, 304). In contrast, leukocytes tend to transmigrate quickly across
endothelium, which reseals over the transmigrated leukocytes. Integration of leukocytes
into endothelium is rarely, if ever, observed, likely because leukocytes have lesser affinity
for the subendothelial extracellular matrix than MSC and other adherent cell types(305).
Fifth, mesenchymal cells are more likely to form multicellular homotypic clusters in
circulation than hematopoetic cells. MSC are prone to forming aggregates in
culture(306), and particularly in suspension(307-309). Similarly, metastasizing cancer
cells have been observed to exist as multicellular clusters in the circulation(3 10, 311). In
contrast, leukocytes rarely form aggregates under physiological conditions.
Sixth, cancer cells have been observed to form intravascular heterotypic aggregates with
platelets and leukocytes. In our study, we also found the majority of intravascular MSC
in contact with neutrophils and platelets. Furthermore, we found that the addition of
MSC to platelet suspensions in vitro led to the rapid formation of visible MSC-platelet
118
'plugs', or a single large MSC-platelet complex (data not shown). This is consistent with
previous observations that MSC have procoagulation properties(3 12), a characteristic
shared with cancer cells(313). Interestingly, heterotypic leukocyte aggregates can also
form under inflammatory conditions such as cancer or myocardial infarction(314).
Specifically, platelets tend to cluster with other nucleated leukocytes, including
neutrophils(315, 316) and monocytes(314, 317). Such complexes have been proposed to
serve as biomarkers for inflammatory pathologies(314). It is unclear if similar
mechanisms mediate leukocyte-platelet and tumor-platelet aggregation, or if unique
adhesion molecules on leukocytes and tumors are mediating their formation.
One way to conceive of hematopoietic trafficking is as "professional" trafficking and
mesenchymal trafficking as "semi-professional" trafficking, due to their differences in
efficiency. Further, mesenchymal trafficking seems to be carried out by cell types that are
typically adherent and rarely found in circulation, and are thus not as well adapted for
trafficking as hematopoietic cells. This conceptualization of a hematopoietic and
mesenchymal mode of trafficking is similar to the concepts of amoeboid and
mesenchymal modes of migration, described for cellular motility in extracellular
matrix(305) and summarized in Table 5.1 and 5.2. Leukocytes tend to utilize amoeboid
modes of migration, while adherent mesenchymal cell types utilize the mesenchymal
mode of migration. Briefly, the amoeboid mode of migration commonly refers to "the
movement of rounded or ellipsoid cells that lack mature focal adhesions and stress
fibers", while mesenchymal migration "involves focalized cell-matrix interactions and
movement in a fibroblast-like manner"(305). It is conceivable that cells that employ
mesenchymal migration on extracellular matrix, also exhibit the characteristics of
mesenchymal trafficking.
While this concept of hematopoietic versus mesenchymal trafficking may be a crude
distinction between two ends of a spectrum of trafficking phenotypes, it will hopefully
serve as an initial framework through which we can approach cellular trafficking of
diverse cell types, and help to organize an otherwise complex literature. Future studies
will be needed to better elucidate the molecular and environmental determinants of
hematopoietic and mesenchymal trafficking to engineer better cell delivery techniques.
119
Table 5.1 Characteristics of hematopoietic versus mesenchymal trafficking
Hematopoietic
"Professional"intravascular trafficking
Majority of time in suspension
No blebbing in suspension
Lateral migration on endothelium using
lamellipodia, invadopodia and podosomes
Does not cause endothelial retraction
Migrate on, through, or below
endothelium in vitro; Rarely integrates
with endothelium
Single cells in suspension
Rarely form heterotypic aggregates with
platelets, except in inflammation
Mesenchymal
"Semi-professional" intravascular
trafficking
Susceptible to anoikis
Blebbing in suspension
No lateral migration; Blebbing on
endothelium
Causes endothelial retraction
Integrates with endothelium in vitro;
Rarely migrates on or below endothelium,
and occasionally migrates through
endothelium
Tend to form homotypic multicellular
clusters in suspension
Forms heterotypic aggregates with
platelets; Procoagulation
Table 5.2 Characteristics of amoeboid versus mesenchymal migration
Amoeboid
Less adherent migration on ECM
Mesenchymal
Strongly adherent migration on ECM
Rounded, amoeboid
Less contractile
Blebs or filopodia with poorly defined,
weak adhesive interactions with
extracellular matrix
Higher speeds of 1-10 pim/min
Non-proteolytic
Minimal cell-cell adhesion (cadherins)
Flat, fibroblastic
Highly contractile
Moderate to high adhesive focal
interactions with extracellular matrix
Lower speeds of 0.1-1 ptm/min
Proteolytic
Significant cell-cell adhesion (cadherins)
120
5.3 FACTORS TO CONSIDER IN CHOOSING CELLS FOR THERAPIES REQUIRING
THEIR TRAFFICKING
Our understanding of these differences between the migratory modes of mesenchymal and
hematopoietic cells begs the question of whether a difference in trafficking efficiency also exists.
In other words, for cell-based therapies where systemically infused cells are desired to target
specific sites, do mesenchymal or hematopoietic cells reach the target site with greater efficiency?
For MSC, multiple studies have found that less than 1% of infused MSC ultimately reach the
target site (Table 2.1). In comparison, leukocytes have been shown to similarly low levels of
engraftment in the target site in some studies. For example, engineered human T cells
intravenously infused into tumor-bearing mice in a model of adoptive immunotherapy were
found to display limited penetration into the tumors, though the actual percentage was not
quantified(3 18). In contrast, a greater percentage of leukocytes have been found to reach their
target sites in other studies. For example, up to 23.5% of intra-nasally delivered dendritic cells
have been found to reach lymph nodes that drain the lungs and nasal mucosa(319). Multiple
variables in each of these studies could account for the observed differences in trafficking
efficiency, as discussed in Chapter 2. Unfortunately, parallel studies that would provide the
requisite comparison of trafficking efficiency between cell types are lacking.
Perhaps the most important question to be asked prior to optimizing trafficking efficiency, is the
number of cells which actually need to arrive at the target site for the desired therapeutic effect to
be achieved. It is still unclear if the anti-inflammatory effects of MSC are exerted locally (at the
site of inflammation) or systemically. No strong link has been made between the number of
MSC that arrive at the site of inflammation, and the strength of their therapeutic effect.
Currently, only a couple of studies have observed an association between the number of MSC
specifically at the site of inflammation and the extent of their anti-inflammatory effects(70, 71).
Unfortunately, these studies did not document the systemic localization of the MSC (e.g. the
number of MSC in the lungs, spleen or liver over time), hence it is impossible make conclusions
regarding the importance of MSC at the site of inflammation. Indeed, anti-inflammatory
proteins like TSG-6 released by MSC embolized in the lungs have been shown to be at least
partially responsible for MSC therapeutic effects(57). Future work is required needed to discern
the local versus systemic effects of MSC.
Other factors besides trafficking efficiency should be considered when choosing a cell type for
therapy. Practically speaking, the cells should preferably be easily isolated, expanded and
maintained in culture. This would allow their practical application in the clinic, where therapies
might need to be deployed at any time, preferably from a stock of available cells in storage. MSC
are easily isolated from bone marrow or adipose tissue, and expanded in vitro, which is ideal for
treatments that require weekly treatments of hundreds of millions of cells, e.g. Osiris' MSC
treatments for Crohn's Disease(320). On the other hand, hematopoietic stem cells are difficult
to maintain and expand in culture, though efforts are underway to address this limitation(321).
Further, the native immunomodulatory effects of the cell types should be considered with
respect to goal of the cell therapy and disease process being treated. Different subsets of
leukocytes (e.g. T cells, B cells, neutrophils, macrophages) have distinct functions. MSC have
been shown to regulate excessive inflammation(322), and their anti-inflammatory effects have
been observed in multiple animal models of disease (Table 2.1). They have, however, been
observed to have pro-inflammatory, pro-tumorigenic effects following long-term engraftment in
tumors(323, 324). Hence, careful consideration is required to ensure that the any native
immunomodulatory effects of the cells are complementary to the goals of the therapy being
designed.
Additionally, some therapies may require the persistence of cell types at the target site subsequent
to their arrival, for example for long-term release of drugs. Typically, the persistence of MSC
dramatically decreases between 24-72 h post-infusion, leading to the 'hit-and-run' description of
the mechanism by which MSC exert their therapeutic effects(325). This relatively rapid
clearance of transplanted allogeneic MSC, which are more practical then autologous MSC for
clinical applications that require a ready supply of MSC, is apparently due to endogenous
immune reactions(325) and does not make them suitable for therapies requiring their long-term
persistence.
Finally, particle-based therapies, which are beyond the scope of this thesis, are also being
explored thoroughly for their use in delivering drugs to sites of inflammation. Many such
therapies load drugs into the particles, which are systemically infused and can accumulate in
inflammatory sites apparently through fenestrated endothelium. Particles include nanoparticles
(which have different trafficking efficiencies depending on size and shapes), liposomes and
carbon nanotubes. Although these particles can only exhibit 'passive' trafficking (i.e. leaking out
through fenestrated endothelium) versus 'active' trafficking that describes the specific protein
interactions between leukocyte and endothelium at target sites, a great compromise may have
been found in particles coated with cell membranes. 'Leukolike vectors', silicon nanoparticles
functionalized with cell membranes purified from leukocytes, were found to transport and
release their drug payload across inflamed endothelium and accumulated in tumors with greater
efficiency than uncoated particles(326). Again, parallel studies are greatly needed to understand
the relative utility of particle versus cell-based technologies for therapies involving trafficking.
5.4 THE INTRAVASCULAR COMPARTMENT AS A SITE OF MSC
IMMUNOMODULATION
Multiple mechanisms of MSC immunomodulation have been elucidated, but the site of
immunomodulation is unclear. Here, we propose that the intravascular compartment may be a
major site of immunomodulation for systemically infused MSC.
Firstly, the intravascular compartment contains a large population of immune cells that MSC
can directly interact with. One such obvious group of immune cells is the circulating cells. These
circulating cells may play a role in the progression of inflammatory pathology, as seen from the
correlation of circulating heterotypic leukocyte aggregate formation with inflammatory
pathologies, e.g. atherosclerosis. In addition, however, MSC may also directly interact with
marginating immune cells, and resident 'patrol' immune cells in the intravascular space.
Marginating immune cells are commonly found in liver, spleen, bone marrow and lungs(8 1).
122
Importantly, these tissues are also where MSC swiftly accumulate following infusion, particularly
lung and liver(195). Further, resident 'patrol' immune cells that seem to engage in long-range
lateral migration on the intraluminal surface of vessels have also been recently found in other
tissues like mesentery, skin and central nervous system(327, 328). However, perhaps most
interesting is that we have found MSC in contact with neutrophils and platelets in the
intravascular compartment of a site of inflammation. Hence, it possible that MSC might not
even need to breach the endothelial barrier to engage directly with immune cells at the site of
inflammation and exert immunomodulatory effects.
Secondly, the functional consequences of MSC adherence on and transmigration through
endothelium at sites of inflammation have not been explored. Rich information exchange
between leukocytes and endothelium during trafficking has been increasingly recognized(329),
but not so for MSC. One exception is a recent report that described how co-incubation of MSC
with endothelium for 20 h led to dose-dependent decrease in neutrophil adhesion to
endothelium(330), raising the possibility that MSC may exert immunomodulatory effects
through interactions with endothelium. Other than acting as a signaling beacon for leukocyte
recruitment from the circulation, endothelium can also present antigen that trigger leukocyte
responses(331) and 'prime' transmigrating leukocytes through leukocyte acquisition of new
adhesion/signaling receptors(329). Hence, MSC may indirectly exert immunomodulatory effects
on immune cells their modulation of endothelial phenotypes during trafficking.
In conclusion, we have sought to elucidate the mechanisms of MSC trafficking to sites of
inflammation following systemic infusion. In the course of our studies, we have investigated the
interaction of MSC with endothelium and other immune cells in the intravascular compartment,
which may account for their trafficking. While the heterogeneity of culture-expanded MSC
likely precludes the elucidation of a single well-defined trafficking mechanism, we discovered
and addressed multiple migratory mechanisms including integrin-mediated adhesion, low-avidity
induced blebbing, mechanical trapping in small vessels, secondary interactions with neutrophils
and platelets, and vascular permeability. In addition, these mechanisms were similar to those
observed for adherent cancer cell types, and provoked the concept of a mesenchymal trafficking
model, as opposed to a hematopoietic model used by leukocytes. Further, the extensive
intravascular interactions between MSC, endothelium and immune cells begs the question of
whether the intravascular compartment represents a major site of immunomodulation for
systemically infused MSC. Future work to extend our findings and address these questions can
add to our understanding of cellular trafficking and MSC biology and refine cellular delivery
strategies for clinical translation.
- END -
123
REFERENCES
1.
2.
Friedenstein A ed (1990) Osteogenic stem cells in the bone marrow), Vol 7, pp 243-272.
Caplan A (1991) Mesenchymal stem cells. Journalof orthopaedicresearch : officia!publicationofthe
OrthopaedicResearch Society 9(5):641-650.
3.
4.
5.
6.
7.
8.
Dominici M, et al. (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The
International Society for Cellular Therapy position statement. Cytotherapy 8(4):315-317.
Bianco P, Robey P, & Simmons P (2008) Mesenchymal stem cells: revisiting history, concepts, and
assays. Cellstem cell 2(4):313-319.
Bianco P, et al (2013) The meaning, the sense and the significance: translating the science of
mesenchymal stem cells into medicine. Nature medicine 19(1):35-42.
da Silva Meirelles L, Chagastelles P, & Nardi N (2006) Mesenchymal stem cells reside in virtually all
post-natal organs and tissues. Journalofcell science 1 19(Pt 11):2204-2213.
Beltrami A, et al. (2007) Multipotent cells can be generated in vitro from several adult human organs
(heart, liver, and bone marrow). Blood 110(9):3438-3446.
Tondreau T, et al. (2004) Bone marrow-derived mesenchymal stem cells already express specific
neural proteins before any differentiation. Differentiation;research in biologicaldiversity 72(7):319-
326.
9.
10.
11.
12.
13.
14.
15.
Brittan M, et al. (2005) A regenerative role for bone marrow following experimental colitis:
contribution to neovasculogenesis and myofibroblasts. Gastroenterology 128(7):1984-1995.
Caplan A (2005) Review: mesenchymal stem cells: cell-based reconstructive therapy in orthopedics.
Tissue engineering 11(7-8):1198-1211.
Schofield R (1978) The relationship between the spleen colony-forming cell and the haemopoietic
stem cell. Blood cells 4(1-2):7-25.
Frenette P, Pinho S, Lucas D, & Scheiermann C (2013) Mesenchymal stem cell: keystone of the
hematopoietic stem cell niche and a stepping-stone for regenerative medicine. Annual review of
immunology 31:285-316.
Sacchetti B, et al. (2007) Self-renewing osteoprogenitors in bone marrow sinusoids can organize a
hematopoietic microenvironment. Cell 131(2):324-336.
Mendez-Ferrer S, et al. (2010) Mesenchymal and haematopoietic stem cells form a unique bone
marrow niche. Nature 466(7308):829-834.
Sugiyama T, Kohara H, Noda M, & Nagasawa T (2006) Maintenance of the hematopoietic stem cell
pool by CXCL12-CXCR4 chemokine signaling in bone marrow stromal cell niches. Immunity
25(6):977-988.
16.
17.
Zhang J, et al. (2003) Identification of the haematopoietic stem cell niche and control of the niche
size. Nature 425(6960):836-841.
Ding L, Saunders T, Enikolopov G, & Morrison S (2012) Endothelial and perivascular cells
maintain haematopoietic stem cells. Nature 481(7382):457-462.
124
18.
da Silva Meirelles L, Caplan A, & Nardi N (2008) In search of the in vivo identity of mesenchymal
stem cells. Stem cells (Dayton, Ohio) 26(9):2287-2299.
19.
20.
Caplan Al (2008) All MSCs are pericytes? Cell Stem Cell 3(3):229-230.
Crisan M, et al. (2008) A perivascular origin for mesenchymal stem cells in multiple human organs.
21.
Crisan M, et al. (2009) Perivascular multipotent progenitor cells in human organs. Annals ofthe New
22.
Paul G, et al. (2012) The adult human brain harbors multipotent perivascular mesenchymal stem
Cell Stem Cell 3(3):301-313.
York Academy ofSciences 1176:118-123.
cells. PloS one 7(4).
23.
24.
25.
26.
27.
James A, et al. (2012) Perivascular stem cells: a prospectively purified mesenchymal stem cell
population for bone tissue engineering. Stem cells translationalmedicine 1(6):510-519.
Duffy G, Ahsan T, O'Brien T, Barry F, & Nerem R (2009) Bone marrow-derived mesenchymal
stem cells promote angiogenic processes in a time- and dose-dependent manner in vitro. Tissue
engineering.PartA 15(9):2459-2470.
Au P, Tam J, Fukumura D, & Jain R (2008) Bone marrow-derived mesenchymal stem cells facilitate
engineering of long-lasting functional vasculature. Blood 11 1(9):4551-4558.
Tang J, Xie Q, Pan G, Wang J, & Wang M (2006) Mesenchymal stem cells participate in
angiogenesis and improve heart function in rat model of myocardial ischemia with reperfusion.
Europeanjournal of cardio-thoracicsurgery : officialjournal of the European Associationfor Cardiothoracic Surgery 30(2):353-361.
Nagaya N, et al. (2004) Intravenous administration of mestnchymal stem cells improves cardiac
function in rats with acute myocardial infarction through angiogenesis and myogenesis. Am J Physiol
Heart Circ Physiol 287(6):H2670-2676.
28.
Huang WH, et al. (2013) Mesenchymal stem cells promote growth and angiogenesis of tumors in
mice. Oncogene 32(37):4343-4354.
29.
30.
31.
32.
33.
34.
Zhang T, et al. (2013) Bone marrow-derived mesenchymal stem cells promote growth and
angiogenesis of breast and prostate tumors. Stem cell research & therapy 4(3):70.
Dore-Duffy P (2008) Pericytes: pluripotent cells of the blood brain barrier. Currentpharmaceutical
design 14(16):1581-1593.
Brighton C, et al.(1992) The pericyte as a possible osteoblast progenitor cell. Clinicalorthopaedics
and related research (275):287-299.
Schor A, Canfield A, Sloan P, & Schor S (1991) Differentiation of pericytes in culture is
accompanied by changes in the extracellular matrix. In vitro cellular& developmental biology : journal
ofthe Tissue Culture Association 27A(8):651-659.
Canfield A, Sutton A, Hoyland J, & Schor A (1996) Association of thrombospondin-1 with
osteogenic differentiation of retinal pericytes in vitro. Journalofcell science 109 ( Pt 2):343-353.
Wang C-H, et al (2008) Late-Outgrowth Endothelial Cells Attenuate Intimal Hyperplasia
Contributed by Mesenchymal Stem Cells After Vascular Injury. Arteriosclerosis, Thrombosis and
VasularBiology 28:54-60.
35.
36.
37.
Ikoma T, et al. (2009) Bone marrow-derived cells from male donors can compose endometrial glands
in female transplant recipients. American journal of obstetrics andgynecology 201(6):6080-6088.
Taylor HS (2004) Endometrial cells derived from donor stem cells in bone marrow transplant
recipients. JAMA : the journalof the American Medical Association 292(1):81-85.
Du H & Taylor HS (2007) Contribution of bone marrow-derived stem cells to endometrium and
endometriosis. Stem cells (Dayton, Ohio) 25(8):2082-2086.
38.
39.
Quante M, et al (2011) Bone Marrow-Derived Myofibroblasts Contribute to the Mesenchymal
Stem Cell Niche and Promote Tumor Growth. Cancer cell 19(2):257-272.
Uccelli A, Moretta L, & Pistoia V (2008) Mesenchymal stem cells in health and disease. Nature
reviews. Immunology 8(9):726-736.
125
40.
41.
Hiroshi Y, et al. (2010) Mesenchymal Stem Cells: Mechanisms of Immunomodulation and Homing.
Cell Transplantation 19.
English K (2013) Mechanisms of mesenchymal stromal cell immunomodulation. Immunolog and
cell biology 91(1):19-26.
42.
43.
Le Blanc K & Ringden 0 (2007) Immunomodulation by mesenchymal stem cells and clinical
experience. Journalofinternalmedicine 262(5):509-525.
Nauta A & Fibbe W (2007) Immunomodulatory properties of mesenchymal stromal cells. Blood
110(10):3499-3506.
44.
45.
46.
47.
48.
Augello A, et al. (2005) Bone marrow mesenchymal progenitor cells inhibit lymphocyte proliferation
by activation of the programmed death 1 pathway. Europeanjournal ofimmunology 35(5):1482-1490.
Zappia E, et al. (2005) Mesenchymal stem cells ameliorate experimental autoimmune
encephalomyelitis inducing T-cell anergy. Blood 106(5):1755-1761.
Selmani Z, et al. (2008) Human leukocyte antigen-G5 secretion by human mesenchymal stem cells is
required to suppress T lymphocyte and natural killer function and to induce
CD4+CD25highFOXP3+ regulatory T cells. Stem cells (Dayton, Ohio) 26(1):212-222.
Deng W, et al. (2005) Effects of allogeneic bone marrow-derived mesenchymal stem cells on T and B
lymphocytes from BXSB mice. DNA and cell biolog 24(7):458-463.
Corcione A, et al. (2006) Human mesenchymal stem cells modulate B-cell functions. Blood
107(1):367-372.
49.
Nauta A, Kruisselbrink A, Lurvink E, Willemze R, & Fibbe W (2006) Mesenchymal stem cells
inhibit generation and function of both CD34+-derived and monocyte-derived dendritic cells.
Journalofimmunolog (Baltimore,Md. : 1950) 177(4):2080-2087.
50.
51.
52.
53.
54.
Jiang X-X, et al. (2005) Human mesenchymal stem cells inhibit differentiation and function of
monocyte-derived dendritic cells. Blood 105(10):4120-4126.
Zhang W, et al. (2004) Effects of mesenchymal stem cells on differentiation, maturation, and
function of human monocyte-derived dendritic cells. Stem cells and development 13(3):263-271.
Sotiropoulou P, Perez S, Gritzapis A, Baxevanis C, & Papamichail M (2006) Interactions between
human mesenchymal stem cells and natural killer cells. Stem cells (Dayton, Ohio) 24(1):74-85.
Li L, et al. (2008) Mesenchymal stem cell transplantation attenuates cardiac fibrosis associated with
isoproterenol-induced global heart failure. Transplant international:officialjournalofthe European
Societyfor Organ Transplantation21(12):1181-1189.
Semedo P, et al. (2009) Mesenchymal stem cells attenuate renal fibrosis through immune modulation
and remodeling properties in a rat remnant kidney model. Stem cells (Dayton, Ohio) 27(12):3063-
3073.
55.
56.
57.
Silva G, et al. (2005) Mesenchymal stem cells differentiate into an endothelial phenotype, enhance
vascular density, and improve heart function in a canine chronic ischemia model. Circulation
111(2):150-156.
Amado L, et al. (2005) Cardiac repair with intramyocardial injection of allogeneic mesenchymal stem
cells after myocardial infarction. Proceedingsof the NationalAcademy of Sciences of the United States of
America 102(32):11474-11479.
Lee RH, et al. (2009) Intravenous hMSCs Improve Myocardial Infarction in Mice because Cells
Embolized in Lung Are Activated to Secrete the Anti-inflammatory Protein TSG-6. Cell Stem Cell
5(1):54-63.
58.
59.
60.
Ren G, et al. (2008) Mesenchymal stem cell-mediated immunosuppression occurs via concerted
action of chemokines and nitric oxide. Cell stem cell 2(2):141-150.
Ryan J, Barry F, Murphy J, & Mahon B (2005) Mesenchymal stem cells avoid allogeneic rejection.
Journalof inflammation (London, England) 2:8.
Groh M, Maitra B, Szekely E, & Koq 0 (2005) Human mesenchymal stem cells require monocytemediated activation to suppress alloreactive T cells. Experimentalhematolog 33(8):928-934.
126
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
Liu W-h, et al. (2013) Novel mechanism of inhibition of dendritic cells maturation by mesenchymal
stem cells via interleukin-10 and the JAK1/STAT3 signaling pathway. PloS one 8(1).
Aggarwal S & Pittenger M (2005) Human mesenchymal stem cells modulate allogeneic immune cell
responses. Blood 105(4):1815-1822.
Timmers L, et al. (2007) Reduction of myocardial infarct size by human mesenchymal stem cell
conditioned medium. Stem cell research 1(2):129-137.
Gnecchi M, et al. (2005) Paracrine action accounts for marked protection of ischemic heart by Aktmodified mesenchymal stem cells. Nature medicine 11(4):367-368.
Ren G, et al. (2010) Inflammatory cytokine-induced intercellular adhesion molecule-I and vascular
cell adhesion molecule-I in mesenchymal stem cells are critical for immunosuppression. Journalof
immunology 184(5):2321-2328.
Zhang B, et al. (2009) Mesenchymal stem cells induce mature dendritic cells into a novel Jagged-2dependent regulatory dendritic cell population. Blood 113(1):46-57.
Chiesa S, et al. (2011) Mesenchymal stem cells impair in vivo T-cell priming by dendritic cells.
Proceedingsofthe NationalAcademy of Sciences of the United States ofAmerica 108(42):17384-17389.
Mutlu G & Factor P (2008) Alveolar epithelial beta2-adrenergic receptors.American journal of
respiratorycell and molecular biology 38(2):127-134.
M6ndez-Ferrer S, Lucas D, Battista M, & Frenette P (2008) Haematopoietic stem cell release is
regulated by circadian oscillations. Nature 452(7186):442-447.
Song H, et al. (2010) Reactive oxygen species inhibit adhesion of mesenchymal stem cells implanted
into ischemic myocardium via interference of focal adhesion complex. Stem cells (Dayton, Ohio)
28(3):555-563.
71.
72.
Xu J, et al. (2012) Allogeneic mesenchymal stem cell treatment alleviates experimental and clinical
Sj6gren syndrome. Blood 120(15):3142-3151.
Sarkar D, Ankrum J, Teo G, Carman C, & Karp J (2011) Cellular and extracellular programming of
cell fate through engineered intracrine-, paracrine-, and endocrine-like mechanisms. Biomaterials
32(11):3053-3061.
73.
74.
75.
76.
77.
78.
79.
Menon L, Kelly K, Yang H, Kim S, & Black... P (2009) Human Bone Marrow-Derived
Mesenchymal Stromal Cells Expressing S-TRAIL as a Cellular Delivery Vehicle for Human Glioma
Therapy. Stem ....
Loebinger M, Eddaoudi A, Davies D, & Janes S (2009) Mesenchymal stem cell delivery of TRAIL
can eliminate metastatic cancer. Cancer research 69(10):4134-4142.
Sun Z, et al. (2013) Scaffold-based delivery of autologous mesenchymal stem cells for mandibular
distraction osteogenesis: preliminary studies in a porcine model. PloS one 8(9).
Dashnyam K, et al. (2013) Hybrid scaffolds of gelatin-siloxane releasing stromal derived factor-I
effective for cell recruitment. Journalof biomedical materials research. PartA.
van de Kamp J, Jahnen-Dechent W, Rath B, Knuechel R, & Neuss S (2013) Hepatocyte growth
factor-loaded biomaterials for mesenchymal stem cell recruitment. Stem cells international
2013:892065.
Phipps M, Xu Y, & Bellis S (2012) Delivery of platelet-derived growth factor as a chemotactic factor
for mesenchymal stem cells by bone-mimetic electrospun scaffolds. PloS one 7(7).
Nedergaard M (2013) Neuroscience. Garbage truck of the brain. Science (New York, N.Y)
340(6140):1529-1530.
80.
81.
Iliff J, et al (2012) A paravascular pathway facilitates CSF flow through the brain parenchyma and
the clearance of interstitial solutes, including amyloid P. Science translationalmedicine 4(147).
Summers C, et al. (2010) Neutrophil kinetics in health and disease. Trends in immunology 31(8):318-
324.
82.
Kalluri R & Weinberg R (2009) The basics of epithelial-mesenchymal transition. The Journalof
clinical investigation 119(6):1420-1428.
127
83.
84.
Hernandez P, et al. (2003) Mutations in the chemokine receptor gene CXCR4 are associated with
WHIM syndrome, a combined immunodeficiency disease. Naturegenetics 34(1):70-74.
Ma Q, Jones D, & Springer T (1999) The chemokine receptor CXCR4 is required for the retention
of B lineage and granulocytic precursors within the bone marrow microenvironment. Immunity
10(4):463-471.
85.
Petty J, Lenox C, Weiss D, Poynter M, & Suratt B (2009) Crosstalk between CXCR4/stromal
derived factor-1 and VLA-4/VCAM- 1 pathways regulates neutrophil retention in the bone marrow.
Journalofimmunology (Baltimore,Md. : 1950) 182(1):604-612.
86.
Athens J, et al. (1961) Leukokinetic studies. IV. The total blood, circulating and marginal
granulocyte pools and the granulocyte turnover rate in normal subjects. The Journalofclinical
investigation 40:989-995.
87.
88.
89.
90.
Fischer U, et al. (2009) Pulmonary passage is a major obstacle for intravenous stem cell delivery: the
pulmonary first-pass effect. Stem cells and development 18(5):683-692.
Weiss L, Dimitrov D, & Angelova M (1985) The hemodynamic destruction of intravascular cancer
cells in relation to myocardial metastasis. Proceedingsof the NationalAcademy of Sciences ofthe United
States ofAmerica 82(17):5737-5741.
Liotta L & Kohn E (2004) Anoikis: cancer and the homeless cell. Nature 430(7003):973-974.
Overholtzer M, et al. (2007) A nonapoptotic cell death process, entosis, that occurs by cell-in-cell
invasion. Cell 131(5):966-979.
91.
92.
93.
94.
95.
96.
Nieswandt B, Hafner M, Echtenacher B, & Minnel D (1999) Lysis of tumor cells by natural killer
cells in mice is impeded by platelets. Cancer research 59(6):1295-1300.
Palumbo J, et al. (2005) Platelets and fibrin(ogen) increase metastatic potential by impeding natural
killer cell-mediated elimination of tumor cells. Blood 105(1):178-185.
Jiang L, et al. (2012) Platelet-mediated Mesenchymal Stem Cells Homing to the Lung Reduces
Monocrotalineinduced Rat Pulmonary Hypertension. Cell transplantation.
Langer HF, et al. (2009) Platelet derived bFGF mediates vascular integrative mechanisms of
mesenchymal stem cells in vitro. Journalof molecular and cellular cardiolog 47(2):315-325.
Iigo Y, et al. (1997) Constitutive expression of ICAM- 1 in rat microvascular systems analyzed by laser
confocal microscopy. The American journalofphysiology 273(1 Pt 2):47.
Watanabe K, et al. (1992) Effect of rat CINC/gro, a member of the interleukin-8 family, on
leukocytes in microcirculation of the rat mesentery. Experimentaland molecularpathology 56(1):60-
69.
97.
98.
99.
100.
101.
Granger D & Senchenkova E (2010) Leukocyte-Endothelial Cell Adhesion. Inflammation and the
Microcirculation, (Morgan & Claypool Life Sciences).
Perry M & Granger D (1991) Role of CD11/CD 18 in shear rate-dependent leukocyte-endothelial
cell interactions in cat mesenteric venules. The Journalof clinical investigation 87(5):1798-1804.
Bienvenu K, Russell J, & Granger D (1992) Leukotriene B4 mediates shear rate-dependent leukocyte
adhesion in mesenteric venules. Circulation research71(4):906-911.
Nazziola E & House S (1992) Effects of hydrodynamics and leukocyte-endothelium specificity on
leukocyte-endothelium interactions.Microvascularresearch44(2):127-142.
Majno G & Palade G (1961) Studies on inflammation. 1. The effect of histamine and serotonin on
vascular permeability: an electron microscopic study. The Journalof biophysicaland biochemical
cytology 11:571-605.
102.
103.
Egawa G, et al. (2013) Intravital analysis of vascular permeability in mice using two-photon
microscopy. Scientific reports 3:1932.
Vestweber D (2012) Relevance of endothelial junctions in leukocyte extravasation and vascular
permeability. Annals ofthe New York Academy of Sciences 1257:184-192.
128
104.
Doerschuk C, Winn R, Coxson H, & Harlan J (1990) CD 18-dependent and -independent
mechanisms of neutrophil emigration in the pulmonary and systemic microcirculation of rabbits.
Journalof immunolog (Baltimore,Md. : 1950) 144(6):2327-2333.
105.
106.
107.
Doerschuk C (2001) Mechanisms of leukocyte sequestration in inflamed lungs. Microcirculation
(New York, N.Y : 1994) 8(2):71-88.
Aird W (2007) Phenotypic heterogeneity of the endothelium: II. Representative vascular beds.
Circulation research 100(2):174-190.
Lee W-Y & Kubes P (2008) Leukocyte adhesion in the liver: distinct adhesion paradigm from other
organs. Journalof hepatology 48(3):504-5 12.
108.
109.
110.
111.
112.
113.
Liu L & Kubes P (2003) Molecular mechanisms of leukocyte recruitment: organ-specific mechanisms
of action. Thrombosis and haemostasis89(2):213-220.
Engelhardt B (2006) Molecular mechanisms involved in T cell migration across the blood-brain
barrier. Journalof neural transmission (Vienna, Austria : 1996) 113(4):477-485.
Alon R, Hammer D, & Springer T (1995) Lifetime of the P-selectin-carbohydrate bond and its
response to tensile force in hydrodynamic flow. Nature 374(6522):539-542.
Springer T (1995) Traffic signals on endothelium for lymphocyte recirculation and leukocyte
emigration. Annual review ofphysiology 57:827-872.
Schenkel AR, Mamdouh Z, & Muller WA (2004) Locomotion of monocytes on endothelium is a
critical step during extravasation. Nat Immunol 5(4):393-400.
Phillipson M, et al. (2006) Intraluminal crawling of neutrophils to emigration sites: a molecularly
distinct process from adhesion in the recruitment cascade. The Journalofexperimental medicine
203(12):2569-2575.
114.
115.
Carman CV (2009) Mechanisms for transcellular diapedesis: probing and pathfinding by
'invadosome-like protrusions'. J Cell Sci 122(17):3025-3035.
Carman C & Springer T (2008) Trans-cellular migration: cell-cell contacts get intimate. Current
opinion in cell biolog 20(5):533-540.
116.
117.
Sage P & Carman C (2009) Settings and mechanisms for trans-cellular diapedesis. Frontiersin
bioscience (Landmark edition) 14:5066-5083.
Lossinsky A & Shivers R (2004) Structural pathways for macromolecular and cellular transport across
the blood-brain barrier during inflammatory conditions. Review. Histology and histopathology
19(2):535-564.
118.
119.
120.
121.
Rubin L & Staddon J (1999) The cell biology of the blood-brain barrier. Annual review of
neuroscience 22:11-28.
Labelle M & Hynes R (2012) The Initial Hours of Metastasis: The Importance of Cooperative HostTumor Cell Interactions during Hematogenous Dissemination. Cancerdiscovery 2(12):1091-1099.
Kornerup K, Salmon G, Pitchford S, Liu W, & Page C (2010) Circulating platelet-neutrophil
complexes are important for subsequent neutrophil activation and migration. Journalofapplied
physiology (Bethesda, Md. : 1985) 109(3):758-767.
Wang J, et al. (2007) Elevated levels of platelet-monocyte aggregates and related circulating
biomarkers in patients with acute coronary syndrome. Internationaljournalofcardiology 115(3):361 -
365.
122.
McCabe D, et al. (2004) Platelet degranulation and monocyte-platelet complex formation are
increased in the acute and convalescent phases after ischaemic stroke or transient ischaemic attack.
Britishjournal of haematology 125(6):777-787.
123.
124.
Huo Y, et al. (2003) Circulating activated platelets exacerbate atherosclerosis in mice deficient in
apolipoprotein E. Nature medicine 9(1):61-67.
Janowska-Wieczorek A, et al. (2001) Platelet-derived microparticles bind to hematopoietic
stem/progenitor cells and enhance their engraftment. Blood 98(10):3143-3149.
129
125.
126.
127.
128.
129.
130.
131.
132.
133.
134.
135.
136.
137.
138.
139.
140.
141.
142.
143.
144.
145.
146.
147.
Caudrillier A, et al. (2012) Platelets induce neutrophil extracellular traps in transfusion-related acute
lung injury. The Journalof clinicalinvestigation 122(7):2661-2671.
McDonald B, Urrutia R, Yipp B, Jenne C, & Kubes P (2012) Intravascular neutrophil extracellular
traps capture bacteria from the bloodstream during sepsis. Cellhost 6-microbe 12(3):324-333.
Clark S, et al. (2007) Platelet TLR4 activates neutrophil extracellular traps to ensnare bacteria in
septic blood. Nature medicine 13(4):463-469.
Brinkmann V & Zychlinsky A (2012) Neutrophil extracellular traps: is immunity the second
function of chromatin? The Journalof cell biology 198(5):773-783.
Demers M & Wagner D (2013) Neutrophil extracellular traps: A new link to cancer-associated
thrombosis and potential implications for tumor progression. Oncoimmunology 2(2).
Brinkmann V, et al. (2004) Neutrophil extracellular traps kill bacteria. Science (New York, N.Y)
303(5663):1532-1535.
Urban C, et al. (2009) Neutrophil extracellular traps contain calprotectin, a cytosolic protein
complex involved in host defense against Candida albicans. PLoSpathogens 5(10).
Cools-Lartigue J, et al (2013) Neutrophil extracellular traps sequester circulating tumor cells and
promote metastasis. The Journalof clinicalinvestigation.
Glinskii 0, et al. (2005) Mechanical entrapment is insufficient and intercellular adhesion is essential
for metastatic cell arrest in distant organs. Neoplasia (New York, N. Y) 7(5):522-527.
Chambers A, Groom A, & MacDonald I (2002) Dissemination and growth of cancer cells in
metastatic sites. Nature reviews. Cancer 2(8):563-572.
Toma C, Pittenger MF, Cahill KS, Byrne BJ, & Kessler PD (2002) Human Mesenchymal Stem Cells
Differentiate to a Cardiomyocyte Phenotype in the Adult Murine Heart. Circulation 105(1):93-98.
Sasaki M, et al. (2008) Mesenchymal stem cells are recruited into wounded skin and contribute to
wound repair by transdifferentiation into multiple skin cell type. Journalof immunology (Baltimore,
Md. : 1950) 180(4):2581-2587.
Zhang M, et al. (2007) SDF- 1 expression by mesenchymal stem cells results in trophic support of
cardiac myocytes after myocardial infarction. FASEBJ 21(12):3197-3207.
Martens TP, et al. (2006) Mesenchymal lineage precursor cells induce vascular network formation in
ischemic myocardium. Nature ClinicalPracticeCardiovascularMedicine 3:S 18-S22.
Nauta AJ & Fibbe WE (2007) Immunomodulatory properties of mesenchymal stromal cells. Blood
110(10):3499-3506.
Phinney DG & Prockop DJ (2007) Concise Review: Mesenchymal Stem/Multipotent Stromal Cells:
The State of Transdifferentiation and Modes of Tissue Repair Current Views. Stem Cells
25(11):2896-2902.
Petite H, et al. (2000) Tissue-engineered bone regeneration. Nature biotechnology 18(9):959-963.
Bantubungi K, et al. (2008) Stem cell factor and mesenchymal and neural stem cell transplantation in
a rat model of Huntington's disease. Molecularand cellular neurosciences 37(3):454-470.
Lee P, et al. (2008) Autologous mesenchymal stem cell therapy delays the progression of neurological
deficits in patients with multiple system atrophy. Clinicalpharmacologyand therapeutics 83(5):723730.
Sackstein R, et al. (2008) Ex vivo glycan engineering of CD44 programs human multipotent
mesenchymal stromal cell trafficking to bone. Nat Med 14(2):181-187.
Kuznetsov SA, et al. (2001) Circulating Skeletal Stem Cells. J Cell Biol. 153(5):1133-1140.
He Q, Wan C, & Li G (2007) Concise review: multipotent mesenchymal stromal cells in blood.
Stem cells 25(1):69-77.
Meirelles LdS, Chagastelles PC, & Nardi NB (2006) Mesenchymal stem cells reside in virtually all
post-natal organs and tissues. J Cell Sci 119(11):2204-2213.
130
148.
149.
150.
Tondreau T, et al. (2005) Mesenchymal Stem Cells Derived from CD 133-Positive Cells in
Mobilized Peripheral Blood and Cord Blood: Proliferation, Oct4 Expression, and Plasticity. Stem
Cells 23(8):1105-1112.
Rochefort GY, et al. (2006) Multipotential Mesenchymal Stem Cells Are Mobilized into Peripheral
Blood by Hypoxia. Stem Cells 24(10):2202-2208.
Wang C-H, et al. (2008) Late-Outgrowth Endothelial Cells Attenuate Intimal Hyperplasia
Contributed by Mesenchymal Stem Cells After Vascular Injury. Arterioscler Thromb Vasc Biol
28(1):54-60.
151.
152.
153.
154.
155.
156.
157.
158.
De Becker A, et al. (2007) Migration of culture-expanded human mesenchymal stem cells through
bone marrow endothelium is regulated by matrix metalloproteinase-2 and tissue inhibitor of
metalloproteinase-3. Haematologica 92(4):440-449.
Rombouts WJ & Ploemacher RE (2003) Primary murine MSC show highly efficient homing to the
bone marrow but lose homing ability following culture. Leukemia 17(1):160-170.
Ruster B, et al. (2006) Mesenchymal stem cells display coordinated rolling and adhesion behavior on
endothelial cells. Blood 108(12):3938-3944.
Wynn RF, et al (2004) A small proportion of mesenchymal stem cells strongly expresses functionally
active CXCR4 receptor capable of promoting migration to bone marrow. Blood 104(9):2643-2645.
Shi M, et al. (2007) Regulation of CXCR4 expression in human mesenchymal stem cells by cytokine
treatment: role in homing efficiency in NOD/SCID mice. Haematologica92(7):897-904.
Annabi B, et al. (2003) Hypoxia Promotes Murine Bone-Marrow-Derived Stromal Cell Migration
and Tube Formation. Stem Cells 21(3):337-347.
Rosova I, Dao M, Capoccia B, Link D, & Nolta JA (2008) Hypoxic Preconditioning Results in
Increased Motility and Improved Therapeutic Potential of Human Mesenchymal Stem Cells. Stem
Cells 26(8):2173-2182.
Sordi V, et al. (2005) Bone marrow mesenchymal stem cells express a restricted set of functionally
active chemokine receptors capable of promoting migration to pancreatic islets. Blood 106(2):419-
427.
159.
160.
161.
162.
163.
164.
165.
166.
167.
168.
Jones EA, et al. (2002) Isolation and characterization of bone marrow multipotential mesenchymal
progenitor cells. Arthritisand rheumatism 46(12):3349-3360.
Simmons PJ & Torok-Storb B (1991) Identification of stromal cell precursors in human bone
marrow by a novel monoclonal antibody, STRO-1. Blood 78(1):55-62.
Chen J, et al (2001) Therapeutic Benefit of Intravenous Administration of Bone Marrow Stromal
Cells After Cerebral Ischemia in Rats. Stroke 32(4):1005-1011.
Schenk S, et al. (2007) Monocyte Chemotactic Protein-3 is a Myocardial MSC Homing Factor. Stem
Cells 25:245-25 1.
Wu J, et al (2008) Intravenously Administered Bone Marrow Cells Migrate to Damaged Brain
Tissue and Improve Neural Function in Ischemic Rats. Cell Transplantation16:993-1005.
Omori Y, et al. (2008) Optimization of a therapeutic protocol for intravenous injection of human
mesenchymal stem cells after cerebral ischemia in adult rats. Brain Research 1236:30-38.
Freyman T, et al. (2006) A quantitative, randomized study evaluating three methods of mesenchymal
stem cell delivery following myocardial infarction. Eur HeartJ 27(9):1114-1122.
Barbash IM, et al. (2003) Systemic Delivery of Bone Marrow-Derived Mesenchymal Stem Cells to
the Infarcted Myocardium: Feasibility, Cell Migration, and Body Distribution. Circulation
108(7):863-868.
Walczak P, et al. (2008) Dual-Modality Monitoring of Targeted Intraarterial Delivery of
Mesenchymal Stem Cells After Transient Ischemia. Stroke 39(5):1569-1574.
Kraitchman DL, et al. (2005) Dynamic Imaging of Allogeneic Mesenchymal Stem Cells Trafficking
to Myocardial Infarction. Circulation 112(10):1451-1461.
131
169.
Chan J, et al. (2007) Widespread Distribution and Muscle Differentiation of Human Fetal
Mesenchymal Stem Cells After Intrauterine Transplantation in Dystrophic mdx Mouse. Stem Cells
25(4):875-884.
170.
171.
172.
173.
174.
Beggs KJ, et al. (2006) Immunologic Consequences of Multiple, High-Dose Administration of
Allogeneic Mesenchymal Stem Cells to Baboons. Cell Transplantation15:711-721.
Muschler GF, Nakamoto C, & Griffith LG (2004) Engineering principles of clinical cell-based tissue
engineering. J Bone Joint Surg Am 86-A(7):1541-1558.
Ley K, Laudanna C, Cybulsky MI, & Nourshargh S (2007) Getting to the site of inflammation: the
leukocyte adhesion cascade updated. Nat Rev Immunol 7(9):678-689.
Chavakis E, Urbich C, & Dimmeler S (2008) Homing and Engraftment of Progenitor Cells: A
prerequisite for cell therapy. JournalofMolecular and Cellular Cardiology In press.
Vajkoczy P, et al. (2003) Multistep Nature of Microvascular Recruitment of Ex Vivo-expanded
Embryonic Endothelial Progenitor Cells during Tumor Angiogenesis. J. Exp. Med. 197(12):1755-
1765.
175.
176.
Diacovo TG, Roth SJ, Buccola JM, Bainton DF, & Springer TA (1996) Neutrophil rolling, arrest,
and transmigration across activated, surface-adherent platelets via sequential action of P-selectin and
the beta 2-integrin CD11 b/CD 18. Blood 88(1):146-157.
von Andrian UH (1997) A massage for the journey: Keeping leukocytes soft andaf%osilent.
Proceedingsofthe NationalAcademy ofSciences of the UnitedStates ofAmerica 94(10):4825-4827.
177.
178.
179.
Francois S, et al. (2006) Local Irradiation Not Only Induces Homing of Human Mesenchymal Stem
Cells at Exposed Sites but Promotes Their Widespread Engraftment to Multiple Organs: A Study of
Their Quantitative Distribution After Irradiation Damage. Stem Cells 24(4):1020-1029.
Mazo IB, Quackenbush EJ, Lowe JB, & von Andrian UH (2002) Total body irradiation causes
profound changes in endothelial traffic molecules for hematopoietic progenitor cell recruitment to
bone marrow. Blood 99(11):4182-4191.
Eder V, et al. (2004) Gamma irradiation induces acetylcholine-evoked, endothelium-independent
relaxation and activatesk-channels of isolated pulmonary artery of rats InternationalJournal
of
Radiation Oncology *Biology*Physics 60(5):1530-1537.
180.
Freas W, Hart JL, Golightly D, McClure H, & Muldoon SM (1989) Contractile properties of
isolated vascular smooth muscle after photoradiation. Am JPhysiolHeart Circ Physiol 256(3):H655-
664.
181.
182.
183.
184.
185.
186.
187.
188.
Ip JE, et al. (2007) Mesenchymal Stem Cells Use Integrin P31 Not CXC Chemokine Receptor 4 for
Myocardial Migration and Engraftment. MolecularBiology ofthe Cell 18:2873-2882.
Goetz DJ, el-Sabban ME, Pauli BU, & Hammer DA (1994) Dynamics of neutrophil rolling over
stimulated endothelium in vitro. Biophys. J. 66(6):2202-2209.
Hong S, et al. (2007) Covalent Immobilization of P-Selectin Enhances Cell Rolling. Langmuir
23(24):12261-12268.
Segers VFM, et al. (2006) Mesenchymal stem cell adhesion to cardiac microvascular endothelium:
activators and mechanisms. Am JPhysiolHeart CircPhysiol 290(4):H 1370-1377.
Sigal A, et al. (2000) The LFA-1 integrin supports rolling adhesions on ICAM-1 under physiological
shear flow in a permissive cellular environment.JImmunol 165(l):442-452.
Alon R, et al. (1995) The integrin VLA-4 supports tethering and rolling in flow on VCAM- 1. J Cell
Biol 128(6):1243-1253.
Salas A, Shimaoka M, Chen S, Carman CV, & Springer T (2002) Transition from rolling to firm
adhesion is regulated by the conformation of the I domain of the integrin lymphocyte functionassociated antigen-1. The Journalof biologicalchemistry 277(52):5025 5-50262.
Steingen C, et al. (2008) Characterization of key mechanisms in transmigration and invasion of
mesenchymal stem cells. JournalofMolecularand Cellular Cardiology In press.
132
189.
190.
191.
192.
193.
194.
195.
196.
197.
198.
199.
200.
201.
202.
203.
204.
205.
206.
207.
Belema-Bedada F, Uchida S, Martire A, Kostin S, & Braun T (2008) Efficient Homing of
Multipotent Adult MSCs Depends on FROUNT-Mediated Clustering of CCR2. Cell Stem Cell
2:566-575.
Hordijk P (2003) Endothelial signaling in leukocyte transmigration. Cell biochemistry and biophysics
38(3):305-322.
Ponte AL, et al. (2007) The in vitro migration capacity of human bone marrow mesenchymal stem
cells: comparison of chemokine and growth factor chemotactic activities. Stem cells (Dayton, Ohio)
25(7):1737-1745.
Stamatovic SM, Keep RF, Kunkel SL, & Andjelkovic AV (2003) Potential role of MCP-1 in
endothelial cell tight junction 'opening': signaling via Rho and Rho kinase. J Cell Sci. 116(22):46154628.
Ries C, et al. (2007) MMP-2, MTI-MMP, and TIMP-2 are essential for the invasive capacity of
human mesenchymal stem cells: differential regulation by inflammatory cytokines. Blood
109(9):4055-4063.
Kim D, et al. (2008) In vivo tracking of human mesenchymal stem cells in experimental stroke. Cell
Transplantation16:1007-1012.
Gao J, Dennis JE, Muzic RF, Lundberg M, & Caplan Al (2001) The dynamic in vivo distribution of
bone marrow-derived mesenchymal stem cells after infusion. Cells Tissues Organs 169:12-20.
Kawada H, et al. (2004) Nonhematopoietic mesenchymal stem cells can be mobilized and
differentiate into cardiomyocytes after myocardial infarction. Blood 104(12):3581-3587.
Devine SM, et al. (2001) Mesenchymal stem cells are capable of homing to the bone marrow of nonhuman primates following systemic infusion. ExperimentalHematology 29:244-255.
Jiang W, et al. (2006) Intravenous transplantation of mesenchymal stem cells improves cardiac
performance after acute myocardial ischemia in female rats. TransplantInternational19(7):570-580.
Pereira RF, et al. (1998) Marrow stomal cells as a source of progenitor cells for nonhemtapoietic
tissues in transgenic mice with a phenotype of osteogenesis imperfecta. Proceedingsof the National
Academy ofSciences 95:1142-1147.
Kumar S & Ponnazhagan S (2007) Bone homing of mesenchymal stem cells by ectopic {alpha}4
integrin expression. FASEBJ. 21(14):3917-3927.
Ortiz LA, et al. (2003) Mesenchymal stem cell engraftment in lung is enhanced in response to
bleomycin exposure and ameliorates its fibrotic effects. Proceedingsof the NationalAcademy ofSciences
100(14):8407-8411.
Wu GD, et al. (2003) Migration of mesenchymal stem cells to heart allografts during chronic
injection. Immunobiolog 75(5):679-685.
Bensidhoum M, et al. (2004) Homing of in vitro expanded Stro-1- or Stro-1+ human mesenchymal
stem cells into the NOD/SCID mouse and their role in supporting human CD34 cell engraftment.
Blood 103(9):3313-3319.
Devine SM, Cobbs C, Jennings M, Bartholomew A, & Hoffman R (2003) Mesenchymal stem cells
distribute to a wide range of tissues following systemic infusion into nonhuman primates. Blood
101:2999.
Hsiao JK, et al. (2007) Magnetic nanoparticle labeling of mesenchymal stem cells without
transfection agent: cellular behavior and capability of detection with clinical 1.5 T magnetic
resonance at the single cell level. Magn Reson Med 58(4):717-724.
Song YS & Ku JH (2007) Monitoring transplanted human mesenchymal stem cells in rat and rabbit
bladders using molecular magnetic resonance imaging. Neurourol Urodyn 26(4):584-593.
Shah BS, Clark PA, Moioli EK, Stroscio MA, & Mao JJ (2007) Labeling of mesenchymal stem cells
by bioconjugated quantum dots. Nano Lett 7(10):3071-3079.
133
208.
Jiang W, et al. (2006) Homing and Differentiation of Mesenchymal Stem Cells Delivered
Intravenously to Ischemic Myocardium in vivo: A Time Series-Study. EuropeanJournalofPhysiology
453:43-52.
209.
210.
Guo J, et al. (2008) Insulin-like growth factor 1 improves the efficacy of mesenchymal stem cells
transplantation in a rat model of myocardial infarction. JournalofBiomedical Science 15(1):89-97.
Mahmood A, Lu D, Qu C, Goussev A, & Chopp M (2005) Human Marrow Stromal Cell
Treatment Provides Long-Lasting Benefit After Traumatic Brain Injury in Rats. Neurosurgery
57(5):1026-1031.
211.
212.
213.
214.
215.
Horita Y, et al. (2006) Intravenous administration of glial cell line-derived neurotrophic factor genemodified human mesenchymal stem cells protects against injury in a cerebral ischemia model in the
adult rat. JournalofNeuroscience Research 84(7):1495-1504.
Khakoo AY, et al. (2006) Human mesenchymal stem cells exert potent antitumorigenic effects in a
model of Kaposi's sarcoma. J. Exp. Med. 203(5):1235-1247.
Rombouts WJC & Ploemacher RE (2003) Primary murine MSC show highly efficient homing to
the bone marrow but lose homing ability following culture. Leukemia 17(1):160-170.
Gao J, Dennis JE, Muzic RF, Lundberg M, & Caplan AI (2001) The dynamic in vivo distribution of
bone marrow-derived mesenchymal stem cells after infusion. Cells, tissues, organs 169(1):12-20.
Spees JL, et al. (2003) Differentiation, cell fusion, and nuclear fusion during ex vivo repair of
epithelium by human adult stem cells from bone marrow stroma. Proc NatlAcad Sci USA
100(5):2397-2402.
216.
217.
218.
219.
Keating A, et al. (1982) Donor origin of the in vitro haematopoietic microenvironment after marrow
transplantation in man. Nature 298(5871):280-283.
Simmons PJ, Przepiorka D, Thomas ED, & Torok-Storb B (1987) Host origin of marrow stromal
cells following allogeneic bone marrow transplantation. Nature 328(6129):429-432.
Cilloni D, et al. (2000) Limited engraftment capacity of bone marrow-derived mesenchymal cells
following T-cell-depleted hematopoietic stem cell transplantation. Blood 96(10):3637-3643.
Tanaka J, et al. (1994) Evaluation of mixed chimaerism and origin of bone marrow derived
fibroblastoid cells after allogeneic bone marrow transplantation. BritishJournalofHaematology
86(2):436-438.
220.
221.
222.
223.
224.
225.
226.
227.
228.
Svennilson J (2005) Novel approaches in GVHD therapy. Bone Marrow Transplant35(S 1):S65-S67.
Koc ON & Lazarus HM (2001) Mesenchymal stem cells: Heading into the clinic. Bone Marrow
Transplant27(3):235-239.
Dominici M, et al. (2006) Minimal criteria for defining multipotent mesenchymal stromal cells. The
International Society for Cellular Therapy position statement. Cytotherapy 8(4):315-317.
Zhang J, Gong J-F, Zhang W, Zhu W-M, & Li J-S (2008) Effects of transplanted bone marrow
mesenchymal stem cells on the irradiated intestine of mice. JournalofBiomedical Science 15:585-594.
Brenner S, et al. (2004) CXCR4-transgene expression significantly improves marrow engraftment of
cultured hematopoietic stem cells. Stem Cells 22(7):1128-1133.
Zhang D, et al. (2008) Over-expression of CXCR4 on mesenchymal stem cells augments
myoangiogenesis in the infarcted myocardium. JMol Cell Cardiol44(2):281-292.
Cheng Z, et al. (2008) Targeted Migration of Mesenchymal Stem Cells Modified With CXCR4
Gene to Infarcted Myocardium Improves Cardiac Performance. Mol Ther 16(3):571-579.
Butcher EC (1991) Leukocyte-endothelial cell recognition: three (or more) steps to specificity and
diversity. Cell 67(6):1033-1036.
Xia L, McDaniel JM, Yago T, Doeden A, & McEver RP (2004) Surface fucosylation of human cord
blood cells augments binding to P-selectin and E-selectin and enhances engraftment in bone marrow.
Blood 104(10):3091-3096.
229.
Lee RJ, et al. (2007) Antibody Targeting of Stem Cells to Infarcted Myocardium. Stem Cells
25(3):712-717.
134
230.
231.
232.
233.
234.
235.
236.
237.
238.
239.
240.
241.
242.
243.
244.
245.
246.
247.
248.
249.
250.
Dennis JE, Cohen N, Goldberg VM, & Caplan Al (2004) Targeted delivery of progenitor cells for
cartilage repair. Journalof OrthopaedicResearch 22(4):735-741.
Sarkar D, et al. (2008) Chemical Engineering of Mesenchymal Stem Cells to Induce a Cell Rolling
Response. Bioconjug Chem.
Potapova IA, Brink PR, Cohen IS, & Doronin SV (2008) Culturing of Human Mesenchymal Stem
Cells as Three-dimensional Aggregates Induces Functional Expression of CXCR4 That Regulates
Adhesion to Endothelial Cells. J. Biol. Chem. 283(19):13100-13107.
NIH (2008) Evaluation of PROCHYMALTM Adult Human Stem Cells for Treatment-Resistant
Moderate-to-Severe Crohn's Disease. ed Health USNIo (ClinicalTrials.gov).
Ankrum J & Karp JM (2009) Mesenchymal stem cell therapy: Two steps forward, one step back.
Trends in MolecularMedicine 16(5):203-209.
Karp JM & Teo GSL (2009) Mesenchymal stem cell homing: the devil is in the details. Cellstem cell
4(3):206-216.
Taylor HS (2004) Endometrial Cells Derived From Donor Stem Cells in Bone Marrow Transplant
Recipients. JAMA: The Journalof the American Medical Association 292(1):8 1-85.
Du H & Taylor HS (2007) Contribution of Bone Marrow-Derived Stem Cells to Endometrium and
Endometriosis. Stem Cells 25(8):2082-2086.
Carman CV (2009) Transmigratory Cups and Invadosome-Like Protrusions: New Aspects of
Diapedesis. In: K Ley, editor. Source: LEUKOCYTE ADHESION Book Series: CURRENT
TOPICS IN MEMBRANES Volume: 64 Pages: 297-333. Amsterdam: Elsevier. 2009.
Schmidt A, et al. (2006) Mesenchymal stem cells transmigrate over the endothelial barrier. European
Journalof Cell Biology 85(11):1179-1188.
Steingen C, et al. (2008) Characterization of key mechanisms in transmigration and invasion of
mesenchymal stem cells. Journalof Molecularand Cellular Cardiology 44(6):1072-1084.
Charras G & Paluch E (2008) Blebs lead the way: how to migrate without lamellipodia. Nat Rev Mol
Cell Biol 9(9):730-736.
Fackler OT & Grosse R (2008) Cell motility though plasma membrane blebbing. Journalof Cell
Biology 181(6):879-884.
Sahai E & Marshall CJ (2003) Differing modes of tumour cell invasion have distinct requirements
for Rho/ROCK signalling and extracellular proteolysis. Nature Cell Biolog 5(8):711-719.
Carman CV & Springer TA (2004) A transmigratory cup in leukocyte diapedesis both through
individual vascular endothelial cells and between them. J. Cell Biol. 167(2):377-388.
Sarkar D, et al. (2008) Chemical Engineering of Mesenchymal Stem Cells to Induce a Cell Rolling
Response. Bioconjugate Chemistry 19(11):2105-2109.
Roux F & Couraud P-O (2003) Rat Brain Endothelial Cell Lines for the Study of Blood-Brain
Barrier Permeability and Transport Functions. Cellularand MolecularNeurobiolog 25(1):41-47.
Romero IA, et al. (2000) Interactions between Brain Endothelial Cells and Human T-Cell Leukemia
Virus Type 1-Infected Lymphocytes: Mechanisms of Viral Entry into the Central Nervous System. J.
Virol. 74(13):6021-6030.
Bernas MJ, et al. (Establishment of primary cultures of human brain microvascular endothelial cells
to provide an in vitro cellular model of the blood-brain barrier. Nat. Protocols 5(7):1265-1272.
Balda MS, et al (1996) Functional dissociation of paracellular permeability and transepithelial
electrical resistance and disruption of the apical-basolateral intramembrane diffusion barrier by
expression of a mutant tight junction membrane protein. The Journalof Cell Biolog 134(4):10311049.
Carman CV, Jun C-D, Salas A, & Springer TA (2003) Endothelial Cells Proactively Form
Microvilli-Like Membrane Projections upon Intercellular Adhesion Molecule 1 Engagement of
6 44
6
Leukocyte LFA-1. J Immunol 171(11): 135- 1 .
135
251.
252.
253.
254.
255.
256.
257.
258.
259.
260.
261.
262.
263.
264.
265.
266.
267.
268.
269.
270.
271.
Barr VA & Bunnell SC (2009) Interference reflection microscopy. Currentprotocols in cell biology /
editorialboard,Juan S. Bonifacino ... fet al Chapter 4:Unit 4 23.
Carman CV, et al. (2007) Transcellular Diapedesis Is Initiated by Invasive Podosomes Immunity
26(6):784-797.
Wagner W, et al. (2008) Replicative Senescence of Mesenchymal Stem Cells: A Continuous and
Organized Process. PLoS ONE 3(5):e2213.
Abel S, et al. (2004) The Transmembrane CXC-Chemokine Ligand 16 Is Induced by IFN-Gamma
and TNF-Alpha and Shed by the Activity of the Disintegrin-Like Metalloproteinase ADAM 10. The
JournalofImmunology 172(10):6362-6372.
Smith H, Whittal C, Weksler B, & Middleton J (2011) Chemokines stimulate bi-directional
migration of human mesenchymal stem cells across bone marrow endothelial cells. Stem Cells and
Development.
Barreiro 0, et al. (2002) Dynamic interaction of VCAM-1 and ICAM-1 with moesin and ezrin in a
novel endothelial docking structure for adherent leukocytes. J Cell Biol 157(7):1233-1245.
Niessen CM (Tight Junctions/Adherens Junctions: Basic Structure and Function. Journalof
Investigative Dermatology 127(11):2525-2532.
Voura EB, Sandig M, & Siu C-H (1998) Cell-cell interactions during transendothelial migration of
tumor cells. Microscopy Research and Technique 43(3):265-275.
Maloney JM, et al. (2010) Mesenchymal stem cell mechanics from the attached to the suspended
state. Biophysicaljournal 99(8):2479-2487.
Chamberlain G, Smith H, Rainger GE, & Middleton J (2011) Mesenchymal Stem Cells Exhibit
Firm Adhesion, Crawling, Spreading and Transmigration across Aortic Endothelial Cells: Effects of
Chemokines and Shear. PLoS ONE 6(9):e25663.
Thankamony SP & Sackstein R (2011) Enforced hematopoietic cell E- and L-selectin ligand
(HCELL) expression primes transendothelial migration of human mesenchymal stem cells.
Proceedingsofthe NationalAcademy of Sciences.
Lozito TP & Tuan RS (2011) Mesenchymal stem cells inhibit both endogenous and exogenous
MMPs via secreted TIMPs. Journalof Cellular Physiology 226(2):385-396.
Barreiro 0, et al. (2008) Endothelial adhesion receptors are recruited to adherent leukocytes by
inclusion in preformed tetraspanin nanoplatforms. The Journalof Cell Biology 183(3):527-542.
Carman CV (2007) The Endothelial Cytoskeleton. EndothelialBiomedicine, ed Aird WC
(Cambridge University Press, Cambridge), pp 696-706.
Byfield FJ, Reen RK, Shentu T-P, Levitan I, & Gooch KJ (2009) Endothelial actin and cell stiffness
is modulated by substrate stiffness in 2D and 3D. Journal ofBiomechanics 42(8):1114-1119.
Krishnan R, et al. (2010) Substrate stiffening promotes endothelial monolayer disruption through
enhanced physical forces. American JournalofPhysiology - Cell Physiolog 300(1):C 146-C 154.
Stroka KM & Aranda-Espinoza H (2011) Endothelial cell substrate stiffness influences neutrophil
transmigration via myosin light chain kinase-dependent cell contraction. Blood 118(6):1632-1640.
Lapis K, Paku S, & Liotta LA (1988) Endothelialization of embolized tumor cells during metastasis
formation. Clinicaland ExperimentalMetastasis 6(1):73-89.
Crissman JD HJ, Schaldenbrand M, Sloane BF, Honn KV (1985) Arrest and extravasation of B16
amelanotic melanoma in murine lungs. A light and electron microscopic study. Laboratory
Investigation 53(4):470-478.
Ghanem A, et al. (2009) Focused ultrasound-induced stimulation of microbubbles augments sitetargeted engraftment of mesenchymal stem cells after acute myocardial infarction. Journalof
Molecular and Cellular Cardiology47(3):411-418.
Estecha A, et al. (2009) Moesin orchestrates cortical polarity of melanoma tumour cells to initiate 3D
invasion. Journalof Cell Science 122(19):3492-3501.
136
272.
273.
274.
275.
276.
277.
Porada C & Almeida-Porada G (2010) Mesenchymal stem cells as therapeutics and vehicles for gene
and drug delivery. Advanced drug delivery reviews 62(12):1156-1166.
Henschler R, Deak E, & Seifried E (2008) Homing of Mesenchymal Stem Cells. Transfusion
medicine and hemotherapy : offizielles Organ der Deutschen Gesel/schaftfur Transfusionsmedizin und
Immunhamatologie 35(4):306-312.
Chamberlain G, Fox J, Ashton B, & Middleton J (2007) Concise review: mesenchymal stem cells:
their phenotype, differentiation capacity, immunological features, and potential for homing. Stem
cells (Dayton, Ohio) 25(11):2739-2749.
Levy 0, et al. (2013) mRNA-engineered mesenchymal stem cells for targeted delivery of interleukin10 to sites of inflammation. Blood.
Fox J, Chamberlain G, Ashton B, & Middleton J (2007) Recent advances into the understanding of
mesenchymal stem cell trafficking. Britishjournal ofhaematology 137(6):491-502.
Spaeth E, Klopp A, Dembinski J, Andreeff M, & Marini F (2008) Inflammation and tumor
microenvironments: defining the migratory itinerary of mesenchymal stem cells. Gene therapy
15(10):730-738.
278.
279.
280.
281.
282.
283.
284.
285.
286.
287.
288.
289.
290.
Semon J, et al (2010) Integrin expression and integrin-mediated adhesion in vitro of human
multipotent stromal cells (MSCs) to endothelial cells from various blood vessels. Cell and tissue
research 341(1):147-158.
Teo G, et al. (2012) Mesenchymal stem cells transmigrate between and directly through tumor
necrosis factor-a-activated endothelial cells via both leukocyte-like and novel mechanisms. Stem cells
(Dayton, Ohio) 30(11):2472-2486.
Veilleux I, Spencer JA, Biss DP, Cote D, & Lin CP (2008) In Vivo Cell Tracking With Video Rate
Multimodality Laser Scanning Microscopy. Selected Topics in Quantum Electronics, IEEEJournalof
14(1):10-18.
Chen M, Whisler J, Jeon J, & Kamm R (2013) MECHANISMS OF TUMOR CELL
EXTRAVASATION IN AN IN VITRO MICROVASCULAR NETWORK PLATFORM. Integr.
Biol.
Svensj6 E & Arfors K (1979) Dimensions of postcapillary venules sensitive to bradykinin and
histamine-induced leakage of macromolecules. Upsalajournal of medicalsciences 84(1):47-60.
Lim L, Solito E, Russo-Marie F, Flower R, & Perretti M (1998) Promoting detachment of
neutrophils adherent to murine postcapillary venules to control inflammation: effect of lipocortin 1.
Proceedings ofthe NationalAcademy of Sciences of the United States ofAmerica 9 5(24):14535-14539.
Sadik C, Kim N, & Luster A (2011) Neutrophils cascading their way to inflammation. Trends in
immunology 32(10):452-460.
Boilard E, et al. (2010) Platelets amplify inflammation in arthritis via collagen-dependent
microparticle production. Science 327(5965):580-583.
Camerer E, et al (2009) Sphingosine-1-phosphate in the plasma compartment regulates basal and
inflammation-induced vascular leak in mice. The Journalof clinicalinvestigation 119(7):1871-1879.
Wang L & Dudek S (2009) Regulation of vascular permeability by sphingosine 1-phosphate.
Microvascularresearch 77(1):39-45.
Gao Z, Zhang L, Hu J, & Sun Y (2013) Mesenchymal stem cells: a potential targeted-delivery vehicle
for anti-cancer drug, loaded nanoparticles. Nanomedicine: nanotechnology, biology, and medicine
9(2):174-184.
Studeny M, et al, (2004) Mesenchymal stem cells: potential precursors for tumor stroma and
targeted-delivery vehicles for anticancer agents. Journalof the National Cancer Institute 96(21):15931603.
Doyle N, et al (1997) Neutrophil margination, sequestration, and emigration in the lungs of Lselectin-deficient mice. TheJournalofclinicalinvestigation 99(3):526-533.
137
291.
292.
293.
294.
Lee RH, et al. (2006) A subset of human rapidly self-renewing marrow stromal cells preferentially
engraft in mice. Blood 107(5):2153-2161.
Carman C & Springer T (2004) A transmigratory cup in leukocyte diapedesis both through
individual vascular endothelial cells and between them. The Journalofcell biology 167(2):377-388.
Schulte D, et al. (2011) Stabilizing the VE-cadherin-catenin complex blocks leukocyte extravasation
and vascular permeability. The EMBOjournal30(20):4157-4170.
Kim M-H, Curry F-RE, & Simon S (2009) Dynamics of neutrophil extravasation and vascular
permeability are uncoupled during aseptic cutaneous wounding. Americanjournalofphysiology. Cell
physiology 296(4):56.
295.
296.
Piston D (2005) When two is better than one: elements of intravital microscopy. PLoS biology 3(6).
Saverymuttu S, Peters A, Keshavarzian A, Reavy H, & Lavender J (1985) The kinetics of 11 indium
distribution following injection of 11 lindium labelled autologous granulocytes in man. British
journalof haematology 61(4):675-685.
297.
298.
van Furth R & Cohn Z (1968) The origin and kinetics of mononuclear phagocytes. The Journalof
experimental medicine 128(3):415-435.
van Furth R, Raeburn J, & van Zwet T (1979) Characteristics of human mononuclear phagocytes.
Blood 54(2):485-500.
299.
300.
301.
Yu X, Cohen D, & Chen C (2012) miR-125b Is an adhesion-regulated microRNA that protects
mesenchymal stem cells from anoikis. Stem cells (Dayton, Ohio) 30(5):956-964.
Shimony N, et al. (2008) A 3D rotary renal and mesenchymal stem cell culture model unveils cell
death mechanisms induced by matrix deficiency and low shear stress. Nephrology, dialysis,
transplantation: official publicationof the European Dialysis and TransplantAssociation - European
RenalAssociation 23(6):2071-2080.
Frisch S & Francis H (1994) Disruption of epithelial cell-matrix interactions induces apoptosis. The
Journalof cell biology 124(4):619-626.
302.
303.
304.
Bergert M, Chandradoss S, Desai R, & Paluch E (2012) Cell mechanics control rapid transitions
between blebs and lamellipodia during migration. Proceedingsofthe NationalAcademy ofSciences of
the UnitedStates ofAmerica 109(36):14434-14439.
Lorentzen A, Bamber J, Sadok A, Elson-Schwab I, & Marshall C (2011) An ezrin-rich, rigid uropodlike structure directs movement of amoeboid blebbing cells. Journalofcell science 124(Pt 8):12561267.
Kramer R & Nicolson G (1979) Interactions of tumor cells with vascular endothelial cell monolayers:
a model for metastatic invasion. Proceedingsof the NationalAcademy of Sciences ofthe United States of
America 76(11):5704-5708.
305.
Friedl P & Wolf K (2010) Plasticity of cell migration: a multiscale tuning model. The Journalofcell
biology 188(1):11-19.
306.
307.
308.
309.
310.
Ferrari C, et al. (2012) Limiting cell aggregation during mesenchymal stem cell expansion on
microcarriers. Biotechnologyprogress 28(3):780-787.
Kuroda Y, et al. (2010) Unique multipotent cells in adult human mesenchymal cell populations.
Proceedingsof the NationalAcademy ofSciences of the UnitedStates ofAmerica 107(19):8639-8643.
Bartosh T, et al. (2010) Aggregation of human mesenchymal stromal cells (MSCs) into 3D spheroids
enhances their antiinflammatory properties.Proceedings ofthe NationalAcademy of Sciences ofthe
United States ofAmerica 107(31):13724-13729.
Welter J, Solchaga L, & Penick K (2007) Simplification of aggregate culture of human mesenchymal
stem cells as a chondrogenic screening assay. Bio Techniques 42(6):7.
Molnar B, Ladanyi A, Tanko L, Sreter L, & Tulassay Z (2001) Circulating tumor cell clusters in the
peripheral blood of colorectal cancer patients. Clinicalcancer research : an officialjournalofthe
American Associationfor CancerResearch 7(12):4080-4085.
138
311.
312.
313.
314.
315.
316.
Glinsky V, et al, (2003) Intravascular metastatic cancer cell homotypic aggregation at the sites of
primary attachment to the endothelium. Cancerresearch 63(13):3805-3811.
Tatsumi K, et al. (2013) Tissue factor triggers procoagulation in transplanted mesenchymal stem cells
leading to thromboembolism. Biochemical and biophysicalresearch communications 431(2):203-209.
Bromberg ME (2004) Clotting and cancer progression: platelets count. Blood 104.
Freedman J & Loscalzo J (2002) Platelet-monocyte aggregates: bridging thrombosis and
inflammation. Circulation 105(18):2130-2132.
Ott I, Neumann F, Gawaz M, Schmitt M, & Scho A (1996) Increased neutrophil-platelet adhesion
in patients with unstable angina. Circulation.
Pamuk G, et al, (2006) Increased circulating platelet-neutrophil, platelet-monocyte complexes, and
platelet activation in patients with ulcerative colitis: a comparative study. American journal of
hematology 81(10):753-759.
317.
318.
319.
Sarma J, et al. (2002) Increased platelet binding to circulating monocytes in acute coronary
syndromes. Circulation 105(18):2166-2171.
Ana Caterina P-P, et al. (2011) Trafficking of CAR-Engineered Human T Cells Following Regional
or Systemic Adoptive Transfer in SCID Beige Mice. Journalof ClinicalImmunology 31.
McCormick S, et al. (2008) Mucosally delivered dendritic cells activate T cells independently of IL-
12 and endogenous APCs. Journalofimmunolog (Baltimore,Md. : 1950) 181(4):2356-2367.
320.
321.
322.
323.
NIH (2008) Evaluation of PROCHYMAL (Adult Human Stem Cells for Treatment-Resistant
Moderate-to-Severe Crohn's Disease.
Walasek M, van Os R, & de Haan G (2012) Hematopoietic stem cell expansion: challenges and
opportunities. Annals of the New York Academy of Sciences 1266:138-150.
Prockop D & Oh J (2012) Mesenchymal stem/stromal cells (MSCs): role as guardians of
inflammation. Molecular therapy: the journalof the American Society of Gene Therapy 20(1):14-20.
Prockop D, et al. (2010) Defining the risks of mesenchymal stromal cell therapy. Cytotherapy
12(5):576-578.
324.
Coffelt S, et al (2009) The pro-inflammatory peptide LL-37 promotes ovarian tumor progression
through recruitment of multipotent mesenchymal stromal cells. Proceedings of the NationalAcademy
of Sciences ofthe United States ofAmerica 106(10):3806-3811.
325.
326.
327.
328.
329.
330.
331.
Ankrum J, Ong J, & Karp J (2014) Mesenchymal stem cells: immune evasive, not immune
privileged. Nature biotechnolog 32(3):252-260.
Parodi A, et al. (2013) Synthetic nanoparticles functionalized with biomimetic leukocyte membranes
possess cell-like functions. Nature nanotechnolog 8(1):61-68.
Auffray C, et al (2007) Monitoring of blood vessels and tissues by a population of monocytes with
patrolling behavior. Science (New York, N. Y) 317(5838):666-670.
Audoy-R6mus J, et al, (2008) Rod-Shaped monocytes patrol the brain vasculature and give rise to
perivascular macrophages under the influence of proinflammatory cytokines and angiopoietin-2. The
Journalof neuroscience: the officialjournalof the Society for Neuroscience 28(41): 10187-10199.
Nourshargh S & Marelli-Berg F (2005) Transmigration through venular walls: a key regulator of
leukocyte phenotype and function. Trends in immunolog 26(3):157-165.
Luu NT, et al. (2013) Crosstalk Between Mesenchymal Stem Cells and Endothelial Cells Leads to
Down-Regulation of Cytokine-iNduced Leukocyte Recruitment. STEM CELLS.
Choi J, Enis DR, Koh KP, Shiao SL, & Pober JS (2004) T lymphocyte-endothelial cell interactions.
Annu. Rev. Immunol 22:683-709.
139