Regeneration of Cartilage Glycosaminoglycan After Degradation by Interleukin-1
BARKER
by
MASSACHUSETTS INSTITUTE
OF TECHNOLOGY
Ashley Williams
APR 2 4 2001
B.S., Aerospace Engineering (1998)
LIBRARIES
University of Colorado - Boulder
Submitted to the Department of Electrical Engineering
in Partial Fulfillment of the Requirements for the Degree of
Master of Science in Electrical Engineering and Computer Science
at the
Massachusetts Institute of Technology
January 2001
© 2001 Massachusetts Institute of Technology
All Rights Reserved
Signature of Author..........................
.......
........... .....
Department of Electrical Engine
Certified by ..................
Accepted by ....................
.....................................
.........-..
ng and Computer Science
January 25, 2001
. . ......................
Martha L. Gray
Professor of Electrical Engineering and eomputer Science
Thesis Supervisor
.
.
.................-------
Arthur C. Smith
Chairman, Committee on Graduate Students
Department of Electrical Engineering and Computer Science
1
Regeneration of Cartilage Glycosaminoglycan After Degradation by Interleukin-1
by
Ashley Williams
Submitted to the Department of Electrical Engineering on January 25, 2001
in Partial Fulfillment of the Requirements for the Degree of
Master of Science in Electrical Engineering and Computer Science
0 Abstract
The osteoarthritic (OA) disease process is characterized by the progressive loss of proteoglycans
(PGs), particularly glycosaminoglycans (GAGs), from the articular cartilage and a subsequent
reduction in the compressive strength of the extracellular matrix (ECM). The concentration of
GAG present in the ECM is therefore used as an indicator of cartilage compositional integrity
and health. Gadolinium-enhanced magnetic resonance imaging of cartilage, a method referred to
as GEMRIC, permits direct, specific and non-destructive measure of cartilage GAG content and
distribution.
The current study employs GEMRIC to follow GAG replenishment over time in cartilage
explants after OA-like degradation. Osteoarthritis-like GAG loss was simulated with the
degradative cytokine interleukin-1 (Il-1). Young bovine articular cartilage explants were
incubated for 3, 6 or 9 days with 10 or 20 ng/ml fl-1 and then cultured in basal media in sterile
NMR tubes. Explants were imaged before and after degradation treatments and then weekly
throughout the recovery period. As per the GEMRIC method, cartilage GAG content was
determined from MRI measured Ti maps via a modified Donnan electrochemical equilibrium
theory. Conversion of TI maps to GAG maps and regional analyses were performed using
custom-coded MATLAB image-processing programs. GAG release to culture media was
monitored daily with DMMB assay.
This study demonstrates that cartilage explants can, at least partially, recover from Il-1-induced
degradation, by synthesizing new glycosaminoglycans. The data show that GAG concentration
increases significantly with time in post-treatment culture and the rate of increase may be
dependant on the proximity to blood vessels in the tissue. The rate of [GAG] recovery varied
between samples and between different regions within a sample, but the mean rate of recovery
observed across all regions of all fl-1 treated samples remained relatively stable at 1-2 mg/ml/day
throughout 3 weeks of recovery. The data also suggest that the average rate of GAG recovery
following 11-1 treatment is independent of absolute GAG content for at least two weeks posttreatment. However, during the 3rd week of post-treatment culture, perivascular regions
exhibited a significant slowing of GAG recovery indicating that the GAG synthesis or retention
capability of the tissue very near to blood vessels was in some way diminished.
Thesis Supervisors: Martha L. Gray, Professor of Electrical Engineering and Computer Science,
MIT, and Deborah Burstein, Associate Professor of Radiology, HMS
2
Table of Contents
0 Abstract ........................................................................................................................................
Table of Tables ...........................................................................................................................
Table of Figures ..........................................................................................................................
1 Introduction.................................................................................................................................
2 Background..................................................................................................................................
2.1 Articular Cartilage Function, Structure and Biochemical Components ............................
2.2 Proteoglycan and Collagen Degradation in Osteoarthritis................................................
2.3 Proteoglycan Degradation and Recovery in Simulated Osteoarthritis ..............................
2.31 M odel System s..........................................................................................................
2.32 Inducing Proteoglycan Degradation in Bovine Explants.............................................
2.33 Degradation Patterns.................................................................................................
2.34 Spatial and Temporal Recovery Patterns ...................................................................
2.4 Non-destructive Quantitative Measurement of Cartilage Proteoglycan ..........................
2.5 Objectives ...........................................................................................................................
3 Methods ......................................................................................................................................
3.1 Culture and D egradation Protocols.................................................................................
3.2 GA G A ssay .........................................................................................................................
3.3 Spectroscopy .......................................................................................................................
3.4 Im aging Protocols ...............................................................................................................
3.5 m age Analysis....................................................................................................................
3.51 Im age Processing ........................................................................................................
3.52 Small Region Analysis...............................................................................................
3.6 Statistical Analysis..............................................................................................................
4 Results ........................................................................................................................................
4.1 Tissue Swelling ...................................................................................................................
4.2 GA G Release Rates............................................................................................................
4.3 Im ages -11-1 Treated Sam ples ........................................................................................
4.4 GA G Recovery Rates - 11-1 Treated Samples.....................................................................
4.41 Degradation Dependence ..........................................................................................
4.42 Depth Dependence ....................................................................................................
4.5 Regional Analysis - 11-1 Treated Samples......................................................................
4.51 Degradation Patterns .................................................................................................
4.52 Regional Recovery Patterns......................................................................................
4.53 Regional Recovery Rates...........................................................................................
4.6 GA G Degradation and Recovery - Trypsin Treatm ents .....................................................
4.61 Degradation...................................................................................................................
4.62 Absolute and N orm alized GAG Recovery ...............................................................
4.63 GAG Recovery Rates....................................................................................................
5 Discussion.................................................................................................................................
5.1 Comparison of Observed and Previously Reported GAG Release Rates.......................
5.2 Comparison of Observed and Previously Reported TI Decrease due to Degradation...
5.3 Comparison of Observed and Previously Reported GAG Synthesis Rates....................
3
2
4
4
5
6
6
7
8
8
9
10
10
11
12
13
13
16
16
16
17
18
19
19
20
20
20
23
26
26
26
29
29
29
31
31
31
31
31
34
34
35
35
5.4 Conclusions from the Current Studies ..............................................................................
5.41 Average GAG Recovery ............................................................................................
5.42 Perivascular GAG Recovery Patterns...........................................................................
5.5 Comparison of Observed and Previously Reported GAG Recovery.............................
5.6 Comparison to Tissue-Engineered Cartilage Studied with MR......................................
5.7 Limitations and Directions for the Future.....................................................................
5.8 C onclusions........................................................................................................................
6
Acknow ledgem ents...............................................................................................................
7 R eferences.................................................................................................................................
Appendix A: Derivation of Donnan Electrochemical Equilibrium Relation..............
Appendix B: Derivation of Tissue Fixed Charge Density (FCD).............................................
Appendix C: Codes for TI Maps ..............................................................................................
Appendix D: MATLAB Code to Scale TI Maps Before Registration....................................
Appendix E: MATLAB Code to Calculate Mean [GAG] in a Sample ...................................
Appendix F: MATLAB Code for Regional Analysis ...............................................................
Appendix G: MATLAB Code to Analyze [GAG] in Pixels Near Blood Vessels....................
A ppendix H : Raw D ata................................................................................................................
Appendix I: DETERMINATION OF FCD WITH MS-325.....................................................
37
37
38
39
41
41
44
45
47
51
52
55
61
63
66
71
80
83
Table of Tables
Table 3.1
Table 4.1
Table 4.2
Table 5.1
Culture Media Formulation....................................................................15
Wet Weights of Samples.....................................................................21
Parameters Used in GAG Calculations....................................................23
GAG Synthesis Estimations....................................................................36
Table of Figures
Figure
Figure
Figure
Figure
Figure
Figure
Figure
Figure
Figure
Figure
Figure
Figure
3.1
3.2
4.1
4.2
4.3
4.4
4.5
4.6
4.7
4.8
4.9
5.1
Shortened NMR Culture/MR Tube and Cardboard Cap.................................14
Imaging Assembly............................................................................14
Daily GAG Release to Culture Media........................................................22
Cummulative GAG Release to Culture Media During 11-1 Treatments..................22
Images of Control and Il-1 Degraded Samples..........................................24
Mean [GAG] Recovery of 11-1 Treated Samples............................................25
Degradation Dependence of [GAG] Recovery..............................................27
Depth Dependence of [GAG] Recovery.....................................................28
Regional Analysis of [GAG] Recovery....................................................30
Images of Control and Trypsin Degraded Samples.........................................32
Mean [GAG] Recovery of Trypsin Treated Samples......................................
33
GAG Loss During IU-1 Treatments by Assay and MRI.................................42
4
1 Introduction
Osteoarthritis (OA) is a potentially debilitating disease of joint inflammation involving the
erosion of cartilage, damage to subchondral bone and impediment of joint function. OA afflicts
as many as 1 in 7 people, over 2/3 of Americans over 65, and is considered a leading cause of
movement limitation due to associated articular dysfunction,
61 .
There is no known cure for OA
and medical management of this disease focuses on pain reduction and limitation of functional
impairment
32.
Nonsteroidal anti-inflammatories (NSAIDs) are most commonly used but are a
frequent cause of serious adverse effects 31,33,34,61. Recently, non-prescription glucosamine and
chondroitin sulfate supplements have gained immense popularity due to their apparent safety and
allegations by several lay publications that they can "cure" arthritis 1'3. A review of human trials
of these supplements by the Journal of the American Medical Association confirmed that
glucosamine and chondroitin preparations "demonstrate moderate to large treatment effects on
symptoms" but that the human studies also exhibit "methodological problems that have been
associated with exaggerated estimates of benefits".
The mechanisms of action of most existing OA drug therapies, including glucosamine and
chondroitin, have not been fully elucidated and are currently a topic of much study by the
osteoarthritis and cartilage research communities 4' 6,8,9, 0 ,23 ,25,26 . Correlating results from such
studies is confounded by the many varieties of OA model systems within which chemical
interventions are studied and by an incomplete knowledge of the model system's behavior before
application of or in the absence of an intervention. Commonly employed model systems include
in vitro cell 4 .6, 22,25 and tissue explant
8,9,10,14,16,23,27
systems as well as in vivo human 33 and animal
studiess,7,26. In order to interpret the effects of chemical interventions within a model system, it
is necessary to first understand the structure, function and metabolism of that system in health
and disease without any intervention.
This thesis examines cartilage metabolism under simulated OA conditions in a bovine explant
model system. Magnetic resonance imaging is used to non-destructively and quantitatively
assess spatial and temporal recovery of cartilage proteoglycan, a biochemical of central
importance in the OA disease process, following cytokine-induced degradation.
5
2 Background
2.1 Articular Cartilage Function, Structure and Biochemical Components
Articular cartilage is a hard, smooth tissue that caps the ends of articulating bones in synovial
joints. Cartilage is a complex composite material capable of withstanding and distributing
compressive loads to subchondral bones while allowing the articulating surfaces to move on each
other with minimal wear and friction.
By weight cartilage tissue is approximately 75% water enmeshed in a network of collagen fibers
containing noncollagenous macromolecules (proteogly cans and hyaluronan), smaller
noncollagenous matrix proteins and cells 36 . The collagen fibers make up the extracellular matrix
(ECM), entrap macromolecules and cells, and lend tensile strength to the tissue'
42 .
Roughly 90-
95% of the collagen in articular cartilage is type II, but types VI, IX, X and XI are also present
38
Proteoglycans (PG) account for up to 10% of cartilage wet weight 3,42. Nearly 95% of these are
polysaccharides attached to a protein backbone (5%)38. Polysaccharides in articular cartilage
generally belong to the family of glycosaminoglycans (GAGs), unbranched disaccharides made
from two sugars (one amino sugar and one other sugar)3 8 . Common forms of GAG found in
articular cartilage include hyaluronic acid, chondroitin sulfate, keratan sulfate, dermatan sulfate
and heparan sulfate 38. Several hundred individual GAG molecules attach covalently as sidechains to a common protein core to form a proteoglycan monomer. In cartilage, proteoglycan
monomers of keratan sulfate and chondroitin sulfate aggregate by linking to a single hyaluronic
acid chain to form aggregates called aggrecans. Water and proteoglycans fill the interfibrillar
space. Most of the PG in cartilage is aggrecan, but several smaller PGs are also present in
articular cartilage: fibromodulin, biglycan, and decorin'.
Cartilage derives its compressive strength from water molecules attracted to GAG in the ECM.
Negatively charged sulfate or carboxylate groups reside on at least one component of each GAG
molecule causing the GAG side-chains to repel each other and other anions while attracting
cations and water molecules3 8 . Considerable osmotic swelling pressures result from water in the
ECM and are responsible for the remarkable compressive strength of articular cartilage4 2 6 2
6
The noncollagenous proteins, glycoproteins, fibronectin and tenascin, are also present in small
amounts in articular cartilage38. These polypeptides are thought to further stabilize the ECM and
anchor chondrocytes to the matrix38 .
Cells, primarily chondrocytes, constitute less than 1% of cartilage tissue volume but are actively
involved in maintaining tissue mechanical integrity via collagen and PG regulation and are also
believed to sense the mechanical environment modifying their PG regulating activities in
36,38
. Proteoglycan metabolism is regulated to maintain a constant
response to changes in loading
concentration of PG's in the matrix, but the balance of PG catabolism and anabolism is altered in
the presence of insulin-like growth factors (IGFs), transforming growth factor-beta (TGF-* ),
interleukin- 1 (11-1) and tumor necrosis factor-alpha (TNF-
)3,36,53
2.2 Proteoglycan and Collagen Degradation in Osteoarthritis
Cartilage damage in osteoarthritis originates with denaturation and loss of type II collagen fibrils
at the articular surface and around chondrocytes, then extends deeper into the tissue with
progressive degeneration' . Damage to collagen fibrils leads to a loss of aggrecan and the
smaller proteoglycans as the ECM network erodes and hyaluronic acid attachments are broken.
Osteoarthritis also involves an increased expression of metalloproteinases (MMPs), but the
reason for this activation of MMPs at the cellular level not yet understood
18
. Once stimulated,
MMPs, in particular stromelysin (MMP-3), several collagenases (MMP-1,-8-13) and an
'aggrecanase' effectively degrade the cartilage ECM "in a sudden and potentially irreversible
manner" 3 . First, collagenases cleave collagen fibrils whose fragments spontaneously denature
39
reducing the tensile properties of the tissue . Second, aggrecanase, an as yet unidentified
proteinase with properties common to the MMP and ADAM family, cleaves the aggrecan core
protein in at least 5 different specific Glu-X bonds between G1 and G2 domains of the
2'3,36,41
interglobular region233'4.
Cleaved aggrecans diffuse out of the matrix causing much of the
endogenous water to leave effectively decreasing the compressive resilience of the ECM.
7
A reduction of the mechanical strength (tensile and compressive) of cartilage alters the loading
environment of chondrocytes in the ECM. These alterations in the ECM loading environment
change chondrocyte-mediated turnover rates of both collagen and proteoglycan4 3' 45 .
Consequently, it is thought that cartilage degradation progressively involves adjacent
chondrocytes in the surrounding matrix through a combination of altered biomechanics and
biochemical production by chondrocytes
. Degradation of cartilage proteoglycan promotes
mechanical dysfunction furthering metabolic imbalances in PG regulation and contributing to the
progressive erosion of cartilage in osteoarthritis. Thus, understanding proteoglycan metabolism
is central to the study of osteoarthritis and potential therapeutic interventions.
2.3 Proteoglycan Degradation and Recovery in Simulated Osteoarthritis
2.31 Model Systems
An ideal model for study of proteoglycan metabolism under osteoarthritis conditions would
allow OA induced metabolic changes to be isolated from all other tissue or cellular metabolic
processes. Given the interdependence of physiological systems such a model is extremely
difficult to achieve in vivo with humans because OA degeneration is frequently coupled with age
or activity related injury. Moreover, only non-destructive imaging and metabolic analysis
measures are permissible for human in vivo cartilage studies.
Most proteoglycan research, therefore, is performed either in vivo with animal models (where
age and activity can be closely controlled and destructive measures are permitted) or in vitro
using human or animal cells and tissue explants. Alginate or tissue-engineered constructs can
provide uniform 3-dimensional cell suspensions that are sufficiently stable to allow long -term
proteoglycan studies49' 50 . However, the extra-cellular environments of cell suspensions are
neither mechanically or biochemically normal. Since the surrounding ECM affects chondrocyte
activities in naturally occurring OA, some PG research questions are better answered in the
context of a natural ECM. Cultured cartilage explants provide a context for studying
chondrocytes in their native ECM, but they also exhibit harvest-site and animal-related variations
in their regulation of PG metabolism. Explants of certain species are better suited for PG studies
than are others. Explanted rabbit cartilage experiences a biphasic PG metabolic response to
culture and may take several weeks to achieve steady-state PG turnover40 . Bovine cartilage
8
explants, on the other hand, are known to achieve steady-state PG turnover rates close to their in
vivo rates within a few days of explantation and can be successfully cultured for 5-6 weeks4 0.
2.32 Inducing Proteoglycan Degradation in Bovine Explants
In human OA, PG degradation is probably initiated by mechanical damage to cartilage from
traumatic injury or overuse and chronic synovitis that give rise to a cascade of chemical events
leading to the PG cleavage by aggrecanase as previously described. OA-like PG degradation can
also be mechanically induced in vitro by compressing tissues or cells with sufficient loads and/or
load rates so as to damage the collagen network and causing chondrocyte death thus disrupting
the normal balance between PG synthesis and catabolism
11 5
, ' ,2. In order to specifically examine
PG metabolism, however, chondrocytes must be viable.
Chemical stimulations of cartilage explants by various degrading agents have been shown to
alter PG metabolism in ways similar to that observed in osteoarthritis. Retinoic acid (vitamin A),
has been found to induce dedifferentiation of chondrocytes and acts as an inhibitor of
chondrogenesis decreasing PG synthesis53 . Enzymes (MMPs, aggrecanase, trypsin) and
proenzyme activators (proMMPs, nitric oxide) cleave PGs from the ECM as previously
described. Cytokines and proinflammatory agents (interleukin-l. , tumor necrosis factor-- ) are
of particular interest in study of PG metabolism because they trigger latent MMPs and initiate
the degradation process. Tumor necrosis factor (TNF-e ) upregulates the transcription of MMPs
in synoviocytes55 . Interleukin-l* (11-1. ) acts more broadly upregulating MMP transcription in
chondrocytes, synovial cells and possibly also endothelial cells5 5 .
Interleukin- 1 is especially interesting because it both initiates PG degradation and also interferes
with synthesis of new PGs36 5, 5 . 11-1 is believed to play a major role in the inflammation and joint
destruction of OA by acting in the disease process at several levels through stimulation of: 1)
collagenase and prostaglandin production by synovial cells, 2) collagenase production by
fibroblasts, and 3) production of prostaglandin and plasminogen activators by articular
chondrocytes4
31
. 11-1 signals chondrocytes via cell surface receptors to upregulate MMPs
aggrecanase (ADMP-1) and collagenase expression and activity while down regulating type II
collagen and PG synthesis and MMP inhibition4 . 11-1 induced proteases increase the rate of PG
9
turnover and can upset the normal balance of catabolic and anabolic processes that regulate
cartilage GAG content.
2.33 Degradation Patterns
Histological evidence (length scale on the order of - 1 tm) suggests that the spatial distribution
of GAG in articular cartilage and the rate of change of that distribution vary with proximity to
chondrocytes. Quinn et al showed that the rate of PG turnover under control conditions is
spatially heterogeneous with greatest rates of GAG degradation and deposition observed
pericellularly". Moreover, Hollander et al reported that PG loss and type II collagen damage
due to I-1 treatment are first observed in the pericellular matrix 1. As a result, increased PG
catabolism and collagen denaturation in pericellular regions is thought to be due to a higher
concentration of membrane-associated or discreted degradative enzymes"" 2 .
Using MRI to observe the spatial patterns of GAG degradation (length scale on the order of 100ptm) in young bovine explants, Bashir et al found a heterogeneous distribution of
degradation with perivascular regions most degraded 3 . In young bovine cartilage, which tends
to be vascular, increased degradation in perivascular regions suggests an increased concentration
of chondrocytes in the vicinity of blood vessels and/or endothelial cell mediation of 1I-1 induced
PG and collagen degradation.
In addition to propagating the cascade of reactions resulting in OA-like cartilage degradation,
chondrocytes themselves may be damaged by exposure to 11-1. Nerucci et al showed that
chondrocytes cultured with 11-1 in vitro appear collapsed and lacking endoplasmic reticulum, the
Golgi apparatus and mitochondria4 . Such 11-1 induced changes likely alter the ability of
chondrocytes to synthesize new PGs and replenish the ECM. The temporal and spatial
distribution of GAG within tissue may therefore be used to infer the location and activities of
viable chondrocytes and the ECM intactness.
2.34 Spatial and Temporal Recovery Patterns
The ability of chondrocytes to replace depleted proteoglycans determines whether cartilage can
continue to withstand mechanical stresses. For this reason, PG regeneration following severe
degradation is of great interest to researchers seeking to arrest and reverse the progression of
OA.
10
Long-term recovery of cartilage PG following severe OA-like degradation has only been
reported by a few researchers. Recently, Allen et al used MRI to observe PG recovery in young
bovine explants after severe and homogeneous trypsin degradation of cartilage
glycosaminoglycan (70% loss). They found cultured cartilage explants capable of restoring
GAG to 85% of its initial concentration following trypsin treatment'4 . Furthermore, GAG
replenishment occurred in a spatially homogenous fashion in planes parallel to the articular
surface and with a depth dependence that reflected the initial physiologic distribution 4 . PageThomas et a15 and Amer7 examined the replenishment of GAG in PG-depleted rabbit knee
cartilage following intra-articular injection of 11-1 using biochemical (DMMB) assays and sulfate
uptake. Page-Thomas et al showed that in vivo, 1I-1 injections caused joint cartilages to lose
roughly 50% of GAG, which was then gradually replaced over 3 to 4 weeks5 . Amer investigated
the age dependence of GAG replenishment after Il-1 injections and found more rapid recovery in
younger animals and decreased recovery rate with increased severity of degradation 7.
Recently Il-1 treated bovine cartilage explants have been used to study the effects of several PG
regulating therapies -10. However, the baseline rates of GAG synthesis and replenishment in Il-1
degraded bovine cartilage explants have not been quantified nor has the spatial distribution of
GAG regeneration in long-term culture been observed following 11-1 degradation. It is not
known if PG replenishment occurs at all in vitro following severe 11-1 degradation in the absence
of any therapeutic interventions. Nor is it known if PG replenishment does occur, whether it
occurs in a spatially homogenous fashion, as observed following trypsin degradation 14 , or in a
pericellular distribution, either parallel or complimentary to that observed following 11-1
degradationi' 1 1.
2.4 Non-destructive Quantitative Measurement of Cartilage Proteoglycan
MR Imaging of Cartilage GAGs in the Presence of a Charged Contrast Agent
Cartilage GAG content can be derived from magnetic resonance (MR) measurements of tissue in
the presence of a negatively charged contrast agent. MR spin-lattice relaxation rates (l/T 1 times)
of tissue measured with and without a contrast agent can be used to determine the concentration
of agent within the tissue. Donnan theory of electrochemical neutrality implies that negatively
11
charged contrast agents distribute in cartilage in concentrations inversely proportional to the
local fixed charge density (FCD). Thus, measurement of the concentration of agent in the tissue
allows calculation of tissue GAG 13
Accurate measurements of cartilage FCD and GAG based on MR measured TI times have been
made with the contrast agent Gd-DTPA 2 (Magnevist, Berlex Laboratories, Wayne, NJ). Bashir
et al demonstrated that tissue T1 times measured in the presence of Gd-DTPA2 can be used as a
sensitive and specific indicator of cartilage FCD and GAG 3 . However, Bashir et al also found
that ideal Donnan-theory FCD predictions based on tissue and bath concentrations of Gd-DTPA 2
under-predicted the actual tissue FCD by a factor of 2
13.
Therefore, an empirical scaling factor
of 2 is needed to modify Donnan-theory FCD predictions when using Gd-DTPA.
(See
Appendix A for a full derivation of cartilage GAG content via Donnan Theory of
electrochemical equilibrium.)
2.5 Objectives
The primary purposes of the current study are:
1) To determine whether young bovine cartilage explants spontaneously recover GAG after IL-I
degradation.
2) To demonstrate a simple, MRI compatible culture system for following GAG
replenishment over time.
To accomplish these goals, we used magnetic resonance imaging to non-destructively and
quantitatively assess both spatial and temporal GAG changes in cultured bovine cartilage
explants after varying degrees of 11-1 degradation.
12
3 Methods
3.1 Culture and Degradation Protocols
Cartilage-bone cores of young bovine articular cartilage from the medial and lateral
femoropatellar groove were harvested within 24 hours of slaughter. Fifteen discs (5mm
diameter by 1mm thick ) from one animal and 6 discs (7mm diameter by 1mm thick) from a
second animal were taken from depths of 1.5 to 5.5 mm below and parallel to the articular
surface. Slices containing the articular surface and tissue up to 1.5 mm below the surface were
excluded from these studies. A flat edge was made on some of the discs to ease orientation and
registration during imaging and analysis. The discs were weighed and then immediately placed
in 2 ml of sterile culture media.
After harvest, samples were first cultured individually in sterile 24-well plates. Immediately
before imaging, the samples were transfered to sterile flat-bottomed 10 mm NMR tubes custom
cut to a length of 5cm (Wilbur Scientific, Boston) and capped with sterile cardboard caps.
Cardboard caps were hand-made and designed to allow gas exchange while maintaining a sterile
internal environment (Rachel Oppenheimer, HIM, Fig. 3.1). For imaging, the cardboard caps
were removed and the shortened NMR/culture tubes were joined to full-length NMR tubes via a
sterilized rubber stopper inserted into the open ends of both tubes (Fig 3.2). The imaging
assembly, consisting of the short NMR tube - rubber stopper - long NMR tube was secured with
tape so that the connection between the tubes was both rigid and long enough to allow the
sample to be positioned in the center of the imaging coil. Between imaging sessions, the samples
were incubated at 370 C and cultured in the shortened NMR tubes capped with sterile cardboard
caps.
Basal culture medium was prepared in 500 ml batches and refrigerated at 4 'C. Samples were
cultured in 2 ml of basal media supplemented daily with 1% by volume heat-inactivated fetal
calf serum, 1-glutamine, ascorbic acid and antibiotics/antimycotics. Media was changed daily
and saved for assay analysis. Media formulation was as follows:
13
flattened
strips of cardboard
sitting on top...
El
of NMR tube
Fig. 3.1 Cardboard caps on shortened NM R
tubes allow gas exchange while maintainin g a
sterile internal environment. Design and
schematic courtesy of Rachel A. Oppenhei mer.
into positioning
spinmer/support
Fig. 3.2 Imaging assembly.
Shortened NMR/culture tube is
joined to an inverted full-length
NMR tube with a sterilized rubber
stopper.
4
inverted NMR tube
0
connectng rubber
stopper
C
Shortened NMR/culture
tube
culture
media
sapde -+
14
I
into magnet
Table 3.1 Culture Media Formulation
Constituent
Culture Media
Low-glucose Dulbecco's modified Eagle
Basal
medium (DMEM)
10 mM HEPES DMEM
Basal
10 mM Non-essential Amino Acids
Basal
100 mM L-proline
Basal
0.5 M gadolinium-DTPA (Magnevist)
Basal
Basal Media
Supplement
200 mM L-Glutamine
Supplement
5 mg/ml Ascorbic Acid
Supplement
500 units/ml Penicillin and
Supplement
0.5 mg/ml Streptomycin
Fetal Calf Serum
Supplement
Amount
300 ml
Source
GIBCO BRL
200 ml
5 ml
2 ml
ml
9.6 ml
0.1 ml
0.1 ml
0.1 ml
GIBCO BRL
Sigma Chemical
Sigma Chemical
Berlex Imaging
0.1 mi
GIBCO BRL
Sigma Chemical
Sigma Chemical
Sigma Chemical
All explants were incubated at 37 'C for 3 to 6 days in basal media before starting degradative
treatments. Control samples were cultured in basal media for the entire experiment. To elicit
degradation, 11-1 P (Cistron Biotechnology, Pine Brooks, NJ) was added daily to the media of 14
samples as outlined below. Following degradative treatments, the samples were cultured in basal
media for the remainder of the experiment.
Two series of 11-1 experiments were conducted, each with its own set of controls. Samples from
the same series were harvested from the same animal (two animals total, one animal for each
experiment series). In the first series, samples were treated for 3&6 days with 10 ng/ml of 11-1
(n=4) and incurred "mild" degradation. In the second series, samples were treated for 6&9 days
with 20 ng/ml of 11-1 (n= 10) and incurred "moderate" degradation. Control samples are referred
to as "mild controls" or "moderate controls" according to the Il-1 series with which they were
cultured (n=2,2).
As a reference point to compare with published literature, three samples were degraded with
trypsin and their recovery was monitored. Three samples were incubated for 5 hours in 15ml of
a trypsin (GIBCO BRL) solution reconstituted with Hanks physiologic saline (GIBCO BRL) to
make a lOX solution. Following incubation in trypsin, the samples were washed in two
consecutive 30-minute baths of fetal calf serum then returned to culture in basal media for the
remainder of the experiment. All trypsin samples were harvested from the "second" animal.
15
3.2 GAG Assay
The quantity of GAG released to the culture medium was measured daily by dimethylmethylene
blue (DMMB) assay. DMMB assay solution was prepared as previously described using 1,9dimethylmethylene chloride (Polysciences, Warrington, PA), NaCl (Mallinckrodt), glycine
(Sigma Chemical), sodium azide (Fluka Chemika, Switzerland), demineralized water and 100%
ethanol (Pharmco, Brookfield, CT)". Culture media was thermally equilibrated to room
temperature then 200 ul of DMMB solution was added to 20 ul of media in a 96 well microtiter
plate. The absorbance at 520nm of the DMMB and media mixture was measured with a
spectrophotometer microplate reader (Molecular Devices). Media GAG concentrations were
determined by comparing measured absorbencies to standards of purified shark chondroitin
sulfate (Sigma Chemical) dissolved in demineralized water. The rate of GAG mass released into
the media per day was calculated by multiplying the measured concentration of GAG in assayed
culture media by media volume (2ml).
3.3 Spectroscopy
Spectroscopy measurements were performed with a Bruker 8.45 T spectrometer (Bruker
Instruments, Billerica, MA, U.S.A.) with a standard 10 mm radiofrequency coil. Tissue Tis
without contrast agent were determined spectroscopically using an inversion delay pulse
sequence with 12 delays ranging from 0.2 to 10 seconds and a 10mm broadband RF probe. An
average tissue TI was measured in each of four samples (two samples from each experiment
series, one control and one degraded sample). Previously, Bashir et al reported that TI did not
change significantly even with complete loss of GAG13 . As expected, very little difference
(<10%) in TI time was found between samples of the same experiment. Therefore, the TI times
in the absence of contrast agent of samples of the same experiment were averaged and these
values assumed for all other samples within the same experiment series.
3.4 Imaging Protocols
All images were acquired on a Bruker 8.45 T microimaging system (Bruker Instruments,
Billerica, MA, U.S.A.) with a standard 10 mm radiofrequency coil. Ti-weighted images in the
axial orientation with respect to explant cylindrical geometry were measured weekly during post-
16
treatment culture with either a saturation recovery ("moderate" series) or inversion recovery
("mild" series) sequence. The saturation-recovery protocol consisted of 10 TI-weighted images
measured with TR times of 25, 75, 125, 175, 275, 375, 475, 600, 900, and 1800 ms. For
inversion-recovery measurements, images were acquired with 9 inversion delays of 16.7, 33.3,
40, 66.7, 100, 150, 250, 400 and 600 ms. Both pulse sequences used a TE of 8.5 ms, section
thicknesses of 0.5 mm, in-plane resolutions of 100
*
m, and 2 averages, for a total imaging time
per sample of less than an hour.
Analysis of GAG release trends following these experiments suggested that within the range of
sensitivity provided by our DMMB assay, GAG release patterns were unaffected by removal
from incubation at 370 C to room temperature for 3-6 hours of imaging each week (as all of the
plugs were out of the incubator for the imaging session).
3.5 Image Analysis
MATLAB (The Math Works, Natick, MA, U.S.A.) was used to create a T1 map by curve-fitting
each TI-weighted image series on a voxel-by-voxel basis. TI maps were then tranformed into
GAG maps with MATLAB using equations derived from a modified ideal Donnan theory. This
GEMRIC (Gadolinium-Enhanced Magnet Resonanance Imaging of Cartilage) method of relating
measured TI and cartilage glycosaminoglycan concentration has previously been validated and
reported'.
(See Appendices A and B for full derivation of Donnan electrochemical equilibrium
theory and GAG determination from TI measurements, respectively.)
Briefly, the concentration of Gd-DTPA2 in the tissue can be derived from measured TI data
according to Equation 1, where TITissue+Agent is the measured TI of tissue equilibrated in contrast
agent, TITissue is the measured TI of tissue without contrast agent, and R is the known relaxivity
of the contrast agent. The relaxivity of Magnevist in tissue at 8.45 Tesla at room temperature is
known to be R=4.5 mMs].
R Tlrissue+Agent
17
Tissue
Fixed charge density (FCD) is calculated from the measured Gd-DTPA2- concentration in the
tissue and the known Gd-DTPA2- concentration in the bath using a quasi-theoretical computation
based on a modified Donnan-theory for ions in electrochemical equilibrium. The empirical factor
of 2 appearing on the right side of Equation 2 is necessary to fit the Donnan-based prediction to
biochemically measured FCD'.
FCD = 2x[Na+], x
I[Gd -DTPA 2-]
[Gd - DTPA
]b
[Gd - DTPA 2-b
[Gd - DTPA2 -]
Eq. 2
Tissue GAG content is calculated by assuming -2 moles of charge per mole of GAG in the tissue
and the molecular weight of GAG = 502.5 g/mole (Equation 3).
[GAG] = FCD 502.5g Imol
2
10
Eq. 3
3.51 Image Processing
Custom coded MATLAB programs that were used to process the MRI data appear in Appendices
C-G. Included are codes to generate a TI map, scale TI maps, transform TI maps into GAG
maps and analyze regions of interest across a series of GAG maps. The mean [GAG] for a given
sample at a given time point was computed as the mean [GAG] calculated across all pixels of the
image. Pixels from image regions corresponding to blood vessels were excluded from mean
[GAG] analysis for images from the "mild" series, where more than 10% of the tissue pixels
appeared in vascular regions. Pixels corresponding to vascular regions of images from the
"moderate" series were included in mean [GAG] calculations because less than 10% of the tissue
pixels appeared in vascular regions and inclusion of these values was found to have a negligible
on mean [GAG] calculations. The rate of [GAG] accumulation, the tissue's recovery rate, was
calculated by comparing mean [GAG] values at various time points and dividing the change in
[GAG] by the elapsed time.
18
3.52 Small Region Analysis
Qualitative assessment of images from samples treated with 11-1 showed that perivascular
regions were, in general, more severely degraded than regions farther from blood vessels at all
time points. In order to objectively quantitate this observation, GAG maps were registered using
Adobe Photoshop to allow chosen regions of interest to be automatically analyzed across
multiple images from successive imaging sessions. Registered images were segmented so that
tissue regions of relatively high, medium, or low [GAG] were identified in images taken 3 weeks
post-treatment. The [GAG] and location of these pixels were tracked in time. High, medium
and low [GAG] regions of the 3-week images were discerned according to the following
definition:
High [GAG]pixei >
(mean [GAG]all
pixels -
(mean [GAG]ai
SDai pixels/ 2 ) <
Low [GAG]pixei <
pixels +
SDal
pixels/ 2 )
Medium [GAG]pixei < (mean [GAG]a 1 pixels
(mean [GAG]ai
pixels -
SDai
pixels/ 2 )
+
SDai pixels/ 2 )
Eq. 4
3.6 Statistical Analysis
MRI derived group mean [GAG] changes were assessed by repeated -measure one-way analysis
of variance (ANOVA) with a compound symmetry variance structure using SAS (SAS Institute
Inc., Cary, NC) to test the hypothesis that mean [GAG] in a given sample or regions of a given
sample did not change in time. This technique analyzed the significance of time as an effect on
weekly [GAG] measurements (or weekly changes in [GAG]) taken from the same samples each
week. Paired two-sample student's t-test (Microsoft Excel) were used to determine the degree of
[GAG] recovery observed with respect to initial, pre-Il- 1-treatment [GAG].
19
4 Results
4.1 Tissue Swelling
Over the total 5 week culture period (2 weeks pre-treatment/treatment phase, plus 3 week
recovery phase) most samples were observed to increase markedly in size. This observation was
supported measurements of initial and final wet weights. Sample volumes at harvest were
nominally the same within each series, 42 ±6 mg for the "mild" series and 19 ±2 mg for the
"moderate series. (This difference in weights between groups was a consequence of the different
plug diameters used for the two studies.) At the end of the study sample weights had increased
by as much as two-fold, with samples in the control, mild and moderate groups increasing by 90
± 27%, 50 ± 11%, 29 ±34%, respectively. The increase in volume was accommodated primarily
by an increase in thickness. Trypsin treated samples (n=3) swelled only slightly in both the axial
and radial directions. Over the course of the experiment, the wet weights of trypsin treated
samples increased by 12-40%. Table 4.1 lists sample wet weights at harvest and after 5-6 weeks
of culture.
4.2 GAG Release Rates
The release of GAG into the media was measured daily as a surrogate for monitoring the effect
of IL- 1 treatment and of stability following IL-I withdrawal. Control samples from each series
had a small rate of release throughout (0.4 ± 0.2 ug/mg initial wet-weight/day), except for
slightly higher release rate (0.7 ± 0.2 ug/mg initial wet-weight/day) in the first 2-3 days
following harvest (Fig 4.1). Assuming an initial [GAG] of roughly 5% of wet weight, this steady
state release rate corresponds to a loss of about 0.6 to 1 %/day.
As expected, during the treatment period, the treated samples lost significantly more GAG than
controls, in accordance with the severity of the treatment. Those in the "mild" and "moderate"
group lost 148 ±49 ug and 433 ±98 ug GAG, respectively compared with the 81 ±5 ug and 103
58 ug lost during the same period by their control samples (Fig 4.2). The GAG release rates
never dropped to negligible levels during the treatment period, indicating that some GAG was
likely remaining in the treated disks (Fig 4.1). Turning to the recovery period, within 1-2 days of
cessation of 11-1 treatments the GAG release rates dropped to levels comparable to control
samples. GAG release persisted at this level (0.3 ± 0.1 and 0.5 ± 0.3 ug/mg initial wet weight/day
20
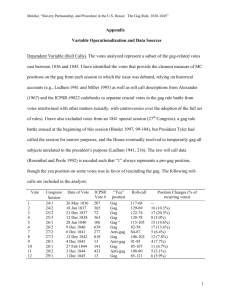
Table 4.1 Wet Weights of Samples
Treatment
plug
wet wt
final wet
Animal
(experimen
@harvest wt [mg]
t series)
[mg]
% weight
change over
culture
period
18%
6-day 11-1
2
11
17.8
21.0
(20 ng/mI)
2
19
24.6
24.0
-2%
"moderate"
2
2
2
2
4
9
20.7
17.9
18.1
36.2
24.5
26.1
75%
37%
44%
9-day 11-1
2
12
20.1
20.8
3%
(20ng/ml)
"moderate"
2
2
17
1
17.9
19.5
21.0
26.0
17%
33%
2
2
14
16
17.4
18.4
20.9
27.2
20%
48%
3-day 11-1
1
3
34.7
47.4
37%
(10ng/mI)
"mild"
1
4
41.2
61.3
49%
6-day H-1
1
5
40.6
66.3
63%
(10ng/mI)
"mild"
1
7
37.0
55.3
49%
Control
"moderate"
2
2
6
10
19.5
18.6
'39.0
27.8
100%
49%
Control
"mild"
1
1
1
2
50.2
47.5
102.0
98.8
103%
108%
Trypsin
5 hrs, 1OX
2
2
2
3
13
15
16.9
18.9
17.9
19.0
23.6
25.1
12%
25%
40%
for "mild" and "moderate" groups respectively) throughout the remainder of the study (Fig 4.1).
Examination of daily release patterns reveals no obvious effects of the imaging protocol on GAG
release, as the data from imaging days and non-imaging days are comparable (Fig 4.1).
Absorbances of trypsin treatment solutions indicate that trypsin-treated samples (n=3) lost about
420 ug sGAG, approximately 50% of their initial GAG, during degradation procedures (see
trypsin protocol in Methods). During the recovery period, trypsin-treated samples released GAG
to media at a steady-state rate of 0.3% initial GAG/day (n=3, std=0.04%).
21
Figure 4.1
120
100
0
0O
80
60
40
60
C
0
-10
-5
0
5
Days of Recovery
10
15
- - - control, 10 ng/ml - - -0- - control, 20 ng/ml -X3-day @ 10 ng/ml
--6-day @ 10 ng/ml - -U- -6-day @ 20 ng/ml - -0- .9-day @ 20 ng/ml
- -
Figure 4.2
700, 600&
500400-
>
-
300...
E 200 -
200-
0
-7
-6
-5
-4
-3
-2
-1
0
1
2
Days of Recovery
e--- control 10 ng - - -o- - - control 20 ng
-*-6
day @ 10 ng --
-x-3
day @ 10 ng
6 day @ 20 ng -o--9 day @ 20 ng
Figures 4.1 and 4.2. GAG released to culture media. (4.1) average daily sGAG release
by each treatment group; (4.2) average amount of sGAG cummulatively lost to media on
each day of 11-1 treatment by each treatment group. Day 0 is the last day of Il-1
treatment and Day 1 is the first day of the "recovery" period.
22
20
4.3 Images - 11-1 Treated Samples
Images of samples measured without/before treatment (n=6 "mild", n=6 "moderate") reveal that
initial [GAG] varied considerably between the two animals (or, equivalently, between the "mild"
and "moderate" series), with initial values ranging from 77 to 105 mg/ml (92 ± 11 mg/ml) for the
animal from the "mild" series and from 50 to 66 mg/ml (57 L 6 mg/ml) for the animal from the
"moderate" series. These differences are illustrated in Figure 4.3, week 0, and pre-treatment
[GAG] values are represented by the shaded regions in Figures 4.4a and b. Images during the
recovery period show that at the initial time point the treated samples had lower [GAG] overall
than control samples, and that the [GAG] in treated samples increased with time of recovery
-2
(Figures 4.3 and 4.4). Table 4.2 lists the known bath concentrations of Gd-DTPA2, measured
tissue TI without Gd-DTPA 2 and measured tissue TI with Gd-DTPA 2 used for each GAG map
generation.
Table 4.2 Parameters used in GAG calculations
[Gd-DTPA -2
Imaging Week
Treatment Group
bath
3&6 days 1I-1 @ 10
ng/ml and 2 controls
Before&After
treatment, 1 week of
Tissue t1
without GdDTPA 2
1.04 mM
1.4 sec
0.97 mM
1.4 sec
0.83 mM
1.6 sec
0.92 mM
1.6 sec
Recovery
3&6 days Il-1 @ 10
2-3 weeks of
ng/ml and 2 controls
Recovery
6 days Il-1 @ 20
ng/ml and 1 controls
Before&After
treatment, 1 week of
Recovery
6 days Il-1 @ 20
2-3 weeks of
ng/ml and 1 controls
Recovery
9 days Il-1 @ 20
ng/ml and 1 controls
9 days Il-1 @ 20
Before Treatment
0.83 mM
1.6 sec
After Treatment
1.25 mM
1.6 sec
1-3 weeks of
0.92 mM
1.6 sec
0.83 mM
1.6 sec
0.92 mM
1.6 sec
ng/ml and
1 controls
9days Il-1 @ 20
ng/ml and
Trypsin
1 controls
Recovery
Before&After
Treatment, 1 week of
Recovery
Trypsin
2-3 weeks of
Recovery
23
The images of the control samples showed relatively stable [GAG] over the culture period.
(Figure 4.3a and c) with the coefficient of variation (SD/mean over time) ranging from 2-12%.
Over the three week recovery period following treatment, [GAG] was seen to increase in all
samples treated with IL-I (Figure 4.3b and d and Figure 4.4; n=14, p<0.0001). In the mild
group the [GAG] increased by 19± 5 mg/ml (n=4, p=0.06) while in the "moderate" group
[GAG] increased by 26± 11 mg/ml (n=10, p<0.000 1).
Only samples for which pretreatment images existed (n=4 "mild"; n=4 "moderate") were
evaluated in terms of degree of degradation (%[GAG]/initial [GAG]). In these cases the [GAG]
after 3 weeks of recovery almost reached pretreatment levels in the "mild" group, 77 ± 19%
(p=0.04 n=4), but reached only 49 ± 11% (p<0.00 1, n=4) in the "moderate" group.
Weeks of Recovery
Before Il-1
Treatment
0 wks
1 wk
2wks
3wks
MILD SERIES
A. Control
80
60
40
B. Treated
m 20
[AG]
MODERATE SERIES
C. Control
60
40
D. Treated
20
[GAG]
mg/ml
Fig. 4.3 Representative GAG map series derived from TI maps measured on successive weeks.
Initial [GAG] was substantially different for the 2 animals (1 animal per series) therefore, each
series is shown on its own colorscale. (A and C) Control [GAG] is stable (COV varied ± 2 to
12%) throughout the recovery period for both series. (B and D) [GAG] of treated samples is
lower than initial[GAG] at the beginning of the recovery period (week 0), and steadily increases
over the 3 week recovery period. As expected, degradation is preferentially perivascular.
24
A
Mildly Degraded Samples
100-Esso--
E
8060--
c
40--
0
0 wks
1 wk
2 wks
3 wks
Weeks of Recovery
70
B
Moderately Degraded Samples
60
1 50
E
40
-.
-.........
o30
-g
C
' 20
10
0
Owks
1wk
2wks
3wks
Weeks of Recovery
Fig. 4.4 [GAG] in I-1 treated samples measured at weekly intervals by GEMRIC. The
mean [GAG] increased with recovery time for samples subjected to (A) mild (3&6
days of 10 ng/ml 11-1, n=4) or (B) moderate (6&9 days of 20 ng/ml I-1, n=10)
degradation then permitted to recover for 3 weeks in culture. The mean [GAG] for a
given sample at a given time point was computed as the mean of [GAG] measured
across all pixels of the image; error bars are ± SD between sample means. Shaded
regions represent pretreatment [GAG]; 92±11 mg/ml for "mild" series and 57±6
mg/mi for "moderate" series.
25
4.4 GAG Recovery Rates - Il-1 Treated Samples
The rate of [GAG] accumulation, the tissue's recovery rate, is inferred from the Figures 4.4a and
4.4b by comparing the means at successive time points. The mean rate of [GAG] recovery
(increase in [GAG]/time) averaged across all pixels of 11-1 degraded samples from both series
was relatively steady, despite wide inter- and intra-sample variation, throughout 3 weeks of posttreatment culture (p=O. 11) at a rate of 1-2 mg/ml/day (1.2 ± 0.9 mg/ml/day).
4.41 Degradation Dependence
The amount of [GAG] remaining in the samples at the completion of Il-1 treatments (i.e. percent
initial [GAG] measured immediately after treatment) was found to significantly affect weekly
[GAG] measurements (p=0.0008) but not the amount of GAG gained in an individual week
(recovery rate, p=O. 11, Figure 4.5). It should be noted that in 7 of 8 cases where normalized
[GAG] recovery analysis was possible, the samples were sliced from depths of 1.5-2.5mm below
the articular surface. The 8th sample of this set was sliced from a depth of 2.5-3.5 mm below the
articular surface.
4.42 Depth Dependence
Images from samples in the "moderate" group, which were taken from -1.5 to 5.5 mm below the
articular surface, suggested that the depth of origin of the samples may influence the rate of
[GAG] recovery. Samples from the deepest levels with respect to the articular surface (3.5 - 5.5
mm below the articular surface, n=6) appeared to recover faster than those taken nearer to the
articular surface (1.5 - 2.5 mm below the articular surface, n=4), but the differences were only
marginally statistically significant (p=0.0 8 ). Figure 4.6 illustrates the depth dependence of
[GAG] recovery rates of "moderate" samples.
26
60%
40%
20%
.1
0%
-J
0-20%
CO
-40%
-60%
1st wk
2nd wk
3rd wk
Week of Recovery
0 3-day @ 10 ng/ml
0 3-day @ 10 ng/ml
N 6-day @ 10 ng/ml
M6-day @ 10 ng/ml
0 6-day @ 20 ng/ml
06-day @ 20 ng/ml
U 9-day @ 20 ng/ml
U 9-day @ 20 ng/ml
Fig. 4.5 Average [GAG] increased the same amount each week independent of the
degree of degradation elicited by 11-1 treatments. Despite large spatial variations of
[GAG] recovery within each sample, the rate of recovery among samples sliced from
depths of 1.5-2.5 mm below the articular surface remained at 5-10 % pre-Il-1
treatment [GAG] through the first 3 weeks of recovery.
27
30
0
25-
E
"
20-
E
S1510-
r
0
I
0-
-5
1st wk
2nd wk
3rd wk
Week of Recovery
0 shallow (n=4)
M deep (n=6)
Fig. 4.6 Rate of [GAG] recovery varied marginally (p=0.08) with distance from the
articular surface. "Shallow" explants, sliced from depths of 1.5-2.5 mm below the surface
(n=4), recovered more slowly than "deep" explants, sliced from 2.5-6.5 mm below the
surface (n=6). The shallow and deep groups shown here each contain an equal number of
samples treated with 20 ng/ml Ill for 6 and 9 days.
28
4.5 Regional Analysis - Il-1 Treated Samples
Looking specifically at the spatial distribution of [GAG], considerable differences in degradation
and weekly [GAG] recovery were clearly evident across different regions of the same sample
and between samples of the same treatment group (Fig. 4.3).
4.51 Degradation Patterns
In both the "mild" and "moderate" groups, heterogeneous degradation patterns prevailed, with
greatest degradation occurring in perivascular regions (Figure 4.3 b,d week 0), though the
degradation in the "moderate" group was more severe and homogeneous than in the "mild"
group. (The control images support the implicit assumption here that the initial pre-treatment
distribution of [GAG] was homogeneous.)
4.52 Regional Recovery Patterns
From a qualitative examination of the recovery images, it can be appreciated that the regions
having relatively low [GAG] after 3 weeks were also the regions having relatively low [GAG]
immediately after treatment (Fig. 4.3).
To examine this observation more quantitatively, and assess whether the rates of GAG
accumulation were correspondingly heterogeneous, the [GAG] accumulation in three "regions",
where the regions are those having "high", "medium" and "low" [GAG] at week 3 (as specified
by Eq. 4), were examined separately (Fig. 4.7). Consistent with the qualitative observations,
vessels are usually surrounded by "low" regions and almost never surrounded by "high" regions
(see sample analysis Appendix G). Quantitative analysis indicated that regions defined as
having "low" [GAG] after 3 weeks of recovery also contained relatively low [GAG] at time 0,
immediately after treatment (Figure 4.7b).
29
A
0 wks
Segmented
3 week
[GAG] Image 3 week image
Weeks of Recovery
2 wks
1 wk
3wks
60
4"high"
OOO
40
~20
"medium"
[GAG]
mg/mi
"low"
C
B
70
30
60
25
E 50
E
40
30
15
44)
E
0E1
to -Z0
o30
10
-
j
2 E
E20
0
~10
-5
-10
0
0 wks
1 wk
2 wks
3 wks
lst wk
2nd wk
3rd wk
Week of Recovery
Weeks of Recovery
Fig. 4.7 (A) Example of regional analysis scheme. [GAG] maps measured after 3 weeks of recovery
were segmented into "low," "medium," and "high" regions according to Equation 4, then the mean
[GAG] of each region was followed in time. As was typically observed, the region defined as "low"
was mostly perivascular while regions of medium and high [GAG] tended not to be perivascular and
were interspersed with each other. At each time point, segmented images were analyzed separately to
assess whether GAG contents and recovery rates were comparable. (B) Weekly mean [GAG] ± SD
of regions defined as "low"(red), "medium"(yellow), or "high" (green)according to the process
illustrated in (A). (C) Weekly changes in mean [GAG] ± SD are shown for each region. Rate of
[GAG] recovery is independent of absolute [GAG] for the first two weeks of post 11-1-treatment
culture. "Low," "medium" and "high" GAG regions recover at statistically different (*) rates during
their third week in post-treatment culture (p<0.0001). All mean [GAG] values and recovery rates are
derived from a total of 10 samples.
30
4.53 Regional Recovery Rates
Interestingly, regions of "low" [GAG] appear to recover at the same rate as do regions of
"medium" or "high" [GAG] during the first 2 weeks of post-treatment culture. In the first two
weeks of recovery, all regions recovered at a rate of 10-15 mg/ml/week. During the third week,
the recovery patterns for the 3 regions differ significantly (p<0.001 ), with the "low" regions
showing negligible [GAG] accumulation and the "high" regions the greatest accumulation
(Figures 4.7b,c).
4.6 GAG Degradation and Recovery - Trypsin Treatments
4.61 Degradation
Figure 4.8 shows that degradation due to trypsin treatments was nearly homogeneous and more
severe than that induced by 11-1 treatments. Comparison of figures 4.3 and 4.8 indicates that
recovery of trypsin-treated samples lagged behind that of 11-1 treated samples. It is unclear from
the images if degradation and recovery of GAG in trypsin-treated samples occurs with a
perivascular distribution .
4.62 Absolute and Normalized GAG Recovery
Three weeks of post-trypsin culture resulted in a net increase in [GAG] for each individual
trypsin-treated sample despite the fact that the combined average [GAG] change of all trypsintreated plugs (n=3) did not increase each week (Figure 4.9a). Repeated-measure ANOVA
analysis indicates [GAG] changes observed during the first three weeks following trypsin
treatment varied significantly with time (p=0.0195). The average GAG contents of the trypsintreated samples fell 75-95% during treatment and then recovered to 30-40% their pre-treatment
[GAG] values in three weeks of culture (Figure 4.9b).
4.63 GAG Recovery Rates
Group mean [GAG] of trypsin-treated samples did not show a steady trend of GAG recovery.
However, comparison of group mean [GAG] measured immediately after treatment and then
after 3 weeks of recovery indicates an average recovery rate of 0.4 mg/ml/day.
31
Weeks of Recovery
Before Trypsin
Treatment
0 wks
1 wk
2wks
3wks
Control
Trypsin
Degraded
Sample
a0
a
4 wks
60
B
40
20
[GAG]
mg/ml
Fig. 4.8 Representative GAG map series derived from TI maps measured on
successive weeks. Control [GAG] is stable (varied ± 2 to 12%) throughout the
recovery period. [GAG] of trypsin treated sample is lower than initial[GAG] at the
beginning of the recovery period (week 0), and steadily increases over the 4 week
recovery period. As expected, degradation is homogenous.
32
A
70
60
50
E
EU
Q
,..
40
-
30
-
I
T
20
10
0
____r_~
0 wks
----
1 wk
2wks
Weeks of Recovery
IETrypsin (n=3)
3wks
M Allen et al
B
120%
4E
ITT
-
100%80%-
0_
60%
-
40%20%
r-
T
T
T
-
0% 4Before
Degradation
I
I1~
1 wk
0 wks,
2 wks
3 wks
Weeks of Recovery
I Plug #15
M Plug
#13
Fig. 4.9 [GAG] is recovered in young bovine cartilage explants pre-treated with lOX
trypsin for 5 hours and then cultured in 10mm NMR tubes. (A) Mean [GAG] of trypsin
treated samples (light grey, n=3) versus weeks after 11-1 treatment; error bars are ± SD
between sample means. Shaded region represents pretreatment [GAG]; 57±6 mg/ml for
"moderate" series. (B) Weekly [GAG] measurements from each of four individual
samples; error bars are ± SD between the =1600 pixels of each sample. [GAG] did not
increase steadily each week in all samples. However, the rate of GAG increase
observed over 4 weeks post-treatment is similar to that observed by Allen et al.
33
5 Discussion
This study clearly demonstrates that cartilage explants can, at least partially, recover from Il-1induced degradation, by synthesizing new glycosaminoglycans. The data show that [GAG]
increases significantly with time in post-treatment culture and the rate of increase may be
dependant on the proximity to blood vessels in the tissue. The data also suggest that the average
rate of [GAG] recovery following 11-1 treatment is independent of absolute [GAG] for at least
two weeks post-treatment. In addition, this study provides an additional demonstration that MRI,
in particular, the in vitro GEMRIC method, can be used to non-destructively and quantitatively
monitor the spatial distribution of GAG concentration over time in culture. In an advance over
previous studies, the studies presented here demonstrate the feasibility of using shortened NMR
tubes as a simple, MRI compatible culture system for individual cartilage explants.
5.1 Comparison of Observed and Previously Reported GAG Release Rates
The rates of GAG release to culture media observed in the studies presented here are in-line with
those reported in the literature 1''
16 .
Quinn et al measured the daily release of sGAG from
control and 11-1 treated bovine calf cartilage explants cultured under conditions similar to those
presented here except for the addition of 10% fetal calf serum to the basal media (samples in the
present study were cultured with 1% FCS)11 . Control samples in the Quinn study released
sGAGs at a steady-state rate of 3-4% per day, which is slightly larger than the 1-2% per day
observed in this study". The difference in control sGAG release rates between these two studies
may be related to the greater dose of FCS employed by Quinn et al. Reported release rates of
sGAGs by adult bovine control explants have varied from 1.3 - 3% per day" 6 .
During 11-1 treatments, Quinn et al reported sGAG release at rates of up to 20% per day in the
presence of 100 ng/ml 11-1". In the current study, the largest one-day sGAG release observed
during 11-1 treatments was 10-15%. However, the concentrations of 11-1 employed in the current
study were only tenth to one fifth that used by Quinn et al. In adult bovine explants, Billinghurst
et al report sGAG release rates of up to 8% per day during treatment with 5 ng/ml l
34
116
5.2 Comparison of Observed and Previously Reported T1 Decrease due to Degradation
After degradation by 11-1 and trypsin, MRI measured TI times of the cartilage explants in the
present study dropped by as much as 60%. Cartilage TI changes of this magnitude have been
previously reported by Bashir et al using similar degradation and imaging protocols'3 .
Specifically, Bashir et al found that the TI of epiphyseal cartilage from newborn bovine calves
dropped about 150 ms after 6 days of incubation with 10 ng/ml when measured in 1mM GdDTPA-2 13. In the present study, samples degraded for 6 days with 10 ng/ml 11-1 (n=2) also
experienced a TI decrease of about 150 ms (from 500 to 350 ms) in the presence of 1mM GdDTPA-2 . Bashir et al also reported that incubation of an intact newborn calf knee joint for 5
hours with 10 mg/ml trypsin led to a TI decrease of roughly 200 ms when imaged with 1mM
Gd-DTPA~2
. In this study, the TI times of trypsin treated explants dropped by about 150ms
(from 380 to 230 ms).
5.3 Comparison of Observed and Previously Reported GAG Synthesis Rates
Examination of MR and assay data reveals that the post-treatment GAG contents of degraded
samples increased in time while steadily releasing GAG to the media. The rate of GAG
synthesis of degraded samples is the sum of the rate of GAG release to media and the rate of
GAG accumulation in the sample. In order to estimate GAG accumulation within a sample, its
volume must be known. Two samples degraded with 11-1 maintained their initial wet weights
within 5% over the entire course of culture (5-6 weeks) and showed no obvious signs of
swelling. Therefore the volume of these samples was assumed constant throughout culture and
was estimated from their initial wet weights. Total sample GAG [mg] was estimated from the
product of volume [ml] and average GAG concentration [mg/ml] measured weekly with MR.
The sum of assay release rates and accumulation rates for the two samples studied suggests a
common GAG synthesis rate of about lug GAG/mg tissue wt/day following 11-1 degradation
(Table 5.1).
The rate of GAG synthesis of control samples in this study is unclear due to significant sample
swelling observed over the course of the experiment (see Table 4.1 in Results). Swelling of all
samples, and especially controls, is to be expected following explantation. The process of slicing
35
Table 5.1 GAG Synthesis Rate of Il-1 Degraded Cartilage
Steady
relative
wet weight
Treatment
Group
plug #
estimated
volume change
@ harvest
final wet
over culture
[mg]
weight [mg]
period
volume of
MR GAG State Assay
MR [GAG]
tissue water recovery rate
[ml]
[mg/ml/day]
recovery
GAG
Total GAG
Synthesis rate
normalized to
release rate tissue weight [mg
rate
[mg/day]
[mg/day]
GAG/mg tissue]
Moderate
6-day
19
24.6
24.0
-2%
0.0175
1.2
0.02
0.005
0.0011
12
20.1
20.8
3%
0.0151
1.2
0.02
0.002
0.0010
Moderate
9-day
Table 5.1 GAG synthesis rates of "moderate" explants pre-treated with 20 ng/ml Il-1 for 6 or 9 days are
estimated from a linear combination of MR derived GAG recovery rates and assay derived GAG release
rates. Rate estimation was only possible for samples whose volume remained constant through 5-6 weeks
of culture (n=2). MR recovery rate represents the net increase in GAG during 3 weeks of post-treatment
culture divided by 21days. In both cases where estimation was possible, similar rates of GAG synthesis
were found.
36
individual cartilage plugs from intact joint tissue necessarily requires cutting collagen fibrils. As
GAG molecules that remain within the matrix osmotically imbibe water against a reduced tensile
integrity, the tissue swells. Thus, swelling is expected to increase with increasing [GAG].
The rate of GAG synthesis estimated in this study is on the order of GAG synthesis rates
formerly measured by us and other labs 14 , 29 . Freed et al. report GAG synthesis rates in terms of
sodium sulfate incorporation for normal human cartilage at 332 ± 36.3 ng sulfate / ug DNA /
day29 . Assuming 1 mole 35SO4 / mole GAG and 502 g/mole GAG, the reported sulfate
incorporation rates correspond to a daily GAG synthesis rate of approximately 5 ug GAG/mg
tissue/day. Previously, our lab reported sulfate incorporation ratios of 0.06-0.13 nmol/mg wet
wt./hour for young bovine cartilage degraded with trypsin 4 . Such rates correspond to roughly
0.7-1.5 ug GAG/mg wet wt /day (assuming I sulfate per disaccharide, 502 g/mol of disaccaride,
and 0.8 ml tissue water/g wet weight) which agree very well with calculated GAG synthesis rates
(1.0-1.1 ug GAG/mg wet wt/day, Table 5.1) in the present study of 11-1 degraded explants.
Furthermore, the rates of GAG regeneration observed following trypsin treatment in the current
study, 0.4-0.6 mg/ml/day, are quite similar to those measured by Allen et al who also measured
GAG recovery via MRI. Allen et al observed GAG recovery in young bovine explants after
severe and homogeneous trypsin degradation of cartilage glycosaminoglycan (70% loss) at rates
of 0.7-0.8 mg/ml/day averaged over 3-4 weeks post-trypsin 4 . Unlike the current study,
however, Allen et al observed GAG replenishment to occur in a spatially homogenous fashion in
planes parallel to the articular surface and with a depth dependence that reflected the initial
physiologic distribution
14
5.4 Conclusions from the Current Studies
5.41 Average GAG Recovery
MR measured [GAG] changes represent the sum of GAG release to media and new GAG
synthesis. Given that the GAG release and synthesis measurements are within the expected
ranges reported in the literature, it is likely that the [GAG] recovery and recovery rates presented
here are both credible and reasonable for this model system.
37
Young bovine articular explants subjected to "mild" degradation (3 or 6 days of Il-1 at 10
ng/ml), resulting in 25-50% GAG loss, were found to recover [GAG] to near control levels
within 2-3 weeks following treatment. Tissue depleted of up to 90% of its GAG by "moderate"
degradation (6 or 9 days of 11-1 at 20 ng/ml), on the other hand, recovered only 30-60% of its
initial value within 3 weeks following 11-1 treatment. The mean rate of [GAG] recovery
observed in 11-1 degraded samples from both series was relatively steady, despite wide inter- and
intra-sample variation, throughout 3 weeks of post-treatment culture at a rate of roughly 1-2
mg/ml/day. Comparison of these GAG accumulation rates with the rate of GAG release into the
culture medium clearly suggests that at least 75% of the GAG synthesized is retained by the
tissue. By contrast, the amount of GAG synthesized in control tissue is roughly equivalent to the
amount released into the medium.
Weekly MRI measurements indicate that the amount of [GAG] measured in a sample recovering
from 11-1 may depend on several factors. First, [GAG] increases significantly with time posttreatment culture, but the rate of [GAG] recovery appears to be independent of the amount of
[GAG] within the sample. Samples of both low and high mean [GAG] after Il-1 treatment
appear to synthesis new GAG at the same rate. Second, the amount of [GAG] within a sample
both before and after degradation varies with animal (bovine calves), degradation protocol and
possibly depth beneath the articular surface. However, the extent to which each of these factors
influenced [GAG] recovery in the present experiment cannot be determined from the data.
5.42 Perivascular GAG Recovery Patterns
It is known that Il-1 degradation of cartilage proteoglycan content occurs in a spatially
heterogeneous pattern with greatest degradation occurring in pericellular regions". In this study,
patterns of GAG recovery following 11-1 degradation were investigated. Interestingly, it was
found that although low GAG regions tended to be perivascular and high GAG regions tended
not to be perivascular, the rate of GAG replenishment in low GAG regions occurred at the same
rate as regions with higher absolute [GAG]. A single average recovery rate independent of
absolute [GAG] persisted for at least the first two weeks of recovery. During the 3 rd week of
post-treatment culture, however, low [GAG] regions exhibited a significant slowing of [GAG]
recovery indicating that the GAG synthesis or retention capability of the tissue very near to
blood vessels was in some way diminished.
38
I am not aware of any histological (or other) data describing the apparent dependence of the rate
of [GAG] replenishment on the proximity to blood vessels. Indeed, it is important to note that
vascular tissue is characteristic of an immature skeleton, and would not be expected in mature
cartilage at risk for OA. Since IL-I-induced degradation preferentially affects the perivascular
regions, it may be reasonable to assume that within a given sample, the perivascular regions are
more severely degraded than regions more distant from the vessels. In that context, the fact the
recovery in the perivascular regions does not keep pace with recovery in more distant regions is
consistent with in vivo observations of IL-I-induced degradation in rabbits that suggested that
recovery rates decreased with severity of degradation7 .
The mechanism for the spatial and temporal heterogeneity in GAG degradation and recovery
following 11-1 treatment is unclear. Since perivascular regions show greater degradation due to
11-1 treatment than less vascular regions, it is likely that tissues in the vicinity of blood vessels
contain a higher density of chondrocytes, epithelial or other 11-1 mediating cells than does the
ECM in non-vascular regions. A slowing of GAG accumulation in perivascular regions during
the third week of recovery may be a manifestation of chondrocyte heterogeneity, or it may
suggest that cell viability in the vicinity of the blood vessels is disrupted rendering the cells
unable to sustain GAG synthesis long after Il-1 treatment. In support of this interpretation is the
fact that IL- 1 has been shown to damage chondrocytes in vitro as evidenced by cell collapse and
lack endoplasmic reticulum, the Golgi apparatus and mitochondria4 . Another possibility is that
the ECM surrounding the vessels is damaged (the collagen scaffold may be heterogenesouly
affected by 11-1), perhaps due to increased collagenase expression and activity, such that the
perivascular ECM is unable to retain newly synthesized GAG. The inherent heterogeneity of
this model may provide a good system for better understanding these mechanisms, and thereby
better understanding the capacity of cartilage to repair osteoarthritis-like degradation.
5.5 Comparison of Observed and Previously Reported GAG Recovery
To my knowledge, no previous attempt has been made to determine the baseline in vitro [GAG]
recovery rate in 11-1 degraded bovine cartilage although [GAG] recovery from 11-1 degradation
has been reported in other model systems. Takegami et al reported post-exposure [GAG]
39
recovery in human intervertebral disc cell suspensions degraded with 0.5 ng/ml Il-1 for 3 days .
During the first two weeks of post-treatment culture, they observed [GAG] recovery rates of
approximately 3-8 mg/mI/day with very little change in [GAG] observed during the third week.
After three weeks of observation, [GAG] recovery achieved by the 11-1 treated cell suspensions
in this study reached about 85% control level 6. Care must be taken when comparing [GAG]
replenishment within alginate suspensions, such as that used in the Takegami study, to [GAG]
replenishment within a naturally occurring ECM, such as that presented in the current study.
The effects of Il-1 on the collagenous ECM and [GAG] retaining abilities are not well
understood and might differ depending on the source and/or structure of the ECM.
Page-Thomas et al investigated GAG replenishment in vivo in rabbit knee joints5. In response to
intra-articular injections of Il-1, They reported that SO 4 uptake and toluidine blue staining
indicated GAG losses of 25-60% in several cartilage sites with gradual recovery over the 3-4
weeks5 . The time courses for [GAG] regeneration in our study and those of the Page-Thomas
study are similar in that both studies saw the greatest weekly gains in GAG during the first two
weeks of recovery and then a slowing of GAG replenishment in the third week. The studies
were dissimilar in the relative magnitudes of GAG loss and also in their overall rates of recovery.
Explanted bovine samples in our study lost up to 90% of their initial [GAG] during treatment
compared to only a 50% decrease in the in vivo rabbit study. Furthermore, GAG was replenished
3 times faster in the in vivo rabbit model than in our in vitro bovine model.
Amer also examined the in vivo effects GAG synthesis and accumulation rabbits following intraarticular injections of I-17. Using DMMB assay and sulfate incorporation, Amer found that both
single and multiple injections of Il-I lead to an initial depression in GAG synthesis rate and
slight drop in tissue [GAG] for 4 days following treatment. After 7-9 days, she observed an
increase in [GAG] accumulation (above post-treatment levels) with recovery achieving 90%
control [GAG] 7. In the present study, GAG synthesis and accumulation rates over the first 4
days of recovery were not specifically examined, but an increase in GAG release to culture
media (evidence of further [GAG] decline) was not observed beyond the first day of recovery in
this in vitro model.
40
The lag-time between 11-1 treatment cessation and tissue [GAG] stabilization/recovery apparent
in Arner's in vivo study and absent in the present in vitro study and the faster GAG recovery
rates observed in Page-Thomas et al's study suggests that Il-1 operates through different
metabolic pathways in the two models. In vivo, 11-1 actions are mediated by many cells in
addition to the chondrocytes (and perhaps vascular endothelial cells) present in in vitro models.
Consequently, caution should be taken in comparing the findings of this study to those of in vivo
models because (aside from the difference in animal species examined) the likely involvement of
synovial cells and inflammation on GAG degradation and recovery processes in vivo was not
modeled in vitro.
5.6 Comparison to Tissue-Engineered Cartilage Studied with MR
Williams et al used the same gadolinium-enhanced MRI method as presented in the current study
to monitor GAG accumulation in tissue engineered cartilage over a period of 6 weeks56 . They
found relatively steady GAG accumulation over the entire culture period. Using proton NMR
without any additional contrast agent, Potter et al observed the growth of tissue engineered over
a period of 4 weeks.
The relative changes in tl and t2 times of these studies suggested that the
overall solid matrix content of neocartilage proteoglycans increased for the first 3 weeks of
culture and remained relatively constant during the fourth week. Both of these studies used a
closed MR-compatible bioreactor system to establish a stable culture environment that could be
transferred to the MR magnet without handling the sample. The system reported here, in which
individual samples were cultured in MR tubes, offers the same ability to image samples in their
culture medium with no handling of the sample while avoiding the use of large volumes of
culture media and maintenance of a cumbersome recirculation system.
5.7 Limitations and Directions for the Future
The imaging and assaying methods used in this study to monitor changes in cartilage GAG
concentration during and after degradative treatments certainly allow relative assessment of
GAG content. However, quantification of absolute GAG recovery is confounded by several
factors. First, different imaging protocols lead to slightly different absolute GAG measurements.
Consecutive TI-images acquired first with inversion recovery (IR) and then by saturation
41
recovery (SR) revealed that TI times measured with SR were 10-15% longer than those
measured with IR, possibly due to a slight difference in relaxivity of Gd-DTPA 2 between the
two methods. Second, the amount of sGAG released from samples to their media does not match
the amount of GAG loss seen in MR images. Figure 5.1 illustrates the disparity between assay
and GEMRIC derived GAG losses observed during 11-1 treatments.
80-
~70~60s50
gAssay
40-
MMRI
A30-
~2010-
0 4
mild
moderate
Fig. 5.1 GAG lost during 11-1 treatment as measured by cummulative GAG released to
culture media (Assay) or by [GAG] change observed with GEMRIC (MRI) over the
treatment period for samples from each treatment series, "mild" and "moderate," (n=4,4)
for which pre-treatment images existed. Initial GAG is estimated as 5% wet weight at
harvest.
While the GAG losses observed with MRI and DMMB assay are of the same order, the disparity
between their absolute values serves as a reminder neither assay nor MRI measures absolute
cartilage GAG. DMMB assay is primarily sensitive to chondroitin sulfate (CS) while up to 8%
of the GAG in bovine calf cartilage may be in the form of keratan sulfate3 0 . In addition, the dyebinding properties of assay calibration standards from shark cartilage CS may be different from
those of young bovine tissue. These effects may cause DMMB assay measurements to slightly
under-estimate GAG release from cartilage explants, as was suggested by the data of
Lesperance 2 . The cummulative effect of small (<5%) daily assay underestimations could explain
the -50% difference between MRI and assay data seen in Figure 5.1.
42
Furthermore, gadolinium-enhanced MRI measurements may slightly over-estimate cartilage
GAG concentration. Gadolinium-enhanced MRI TI measurements of cartilage FCD are not
exclusively sensitive to cartilage GAG. Tissue constituents other than GAG (collagen, decorin
and hyaluronate, for example) contribute to the fixed charge density of the tissue, although their
net contribution is assumed to be quite small42 . Consequently, Gd-DTPA-2 distributes in inverse
proportion to all negatively charged molecules, potentially causing overestimation of cartilage
GAG by MRI.
Although perhaps more reliable than absolute GAG values, relative GAGchange trends
measured between pixels within a sample, between samples and over time are not free from
errors. In order to calculate GAG content from a measured TI time in the presence of GdDTPA-2, it is necessary to also know the rate of tissue relaxation without Gd-DTPA-2. For these
studies, a single value of T1 without Gd-DTPA
2
was applied to all pixels within an image and to
all images within an experiment. Theoretical calculations indicate that this procedure introduces
an uncertainty of about 10% in GAG calculations. In addition, noise in the TI measurements
due to magnetic field inhomogeneities may also be propagated into GAG calculations.
Il-1 induces heterogeneous degradation, with perivascular regions more degraded than less
vascular regions. It is unclear from the data of this study whether or not GAG regeneration
following 11-1 degradation occurs in a similarly heterogeneous fashion. The reason for the
confusion is twofold. First, the ability to track the GAG content of a small region in time is
limited by the ability of all images of a series to be accurately registered. Careful slice selection
and image rotation have resulted in images that appear to be accurately registered ± 3 pixels.
Tissue swelling (often asymmetrically) is known to have occurred in the course of these
experiments, so registration accuracy is limited to h 0.5 mm. Secondly, pre-treatment images are
lacking from some samples preventing the interpretation of their post-treatment GAG recovery
from being assessed in terms of percent initial GAG or with respect to blood vessel proximity.
Further studies are necessary to test if full [GAG] recovery can be achieved with more than 3
weeks of post-treatment culture. As seen in the present study, biological variability between
samples from different animals and between samples from different source locations or depths
43
from the same animal complicate the analysis and confound the conclusions. Therefore, future
studies of this type would benefit from the inclusion of more control samples harvested from as
many depths and locations as the studied samples. Likewise, pre-treatment images are needed
for all samples so that post-treatment recoveries can be referenced to their own individual control
or "healthy" state. Finally, future analysis requiring knowledge of absolute sample GAG would
be greatly aided by 3-dimensional image sets from which sample volumes, and hence sample
GAG, can be accurately determined.
5.8 Conclusions
Unlike in vivo or in vitro models that utilize sulfate incorporation to measure GAG
replenishment, MR GAG imaging of cartilage GAG content provides additional information
about the spatial distribution of GAG loss and recovery. Furthermore, the non-destructive nature
of MR imaging allows the spatial distribution of GAG in the same sample or same tissue region
to be tracked in time. Application of this technique to monitoring GAG replenishment in Ildegraded samples has uncovered further evidence for cellular regulation of both GAG synthesis
and matrix-modeling agents. As predicted by Page-Thomas et al, we have evidence to suggest
that "chondrocytes are well able to repack the matrix with proteoglycan if the collagenous
framework is intact
The findings of this thesis demonstrate a basis for evaluating the spatial and temporal effects of
chemical and mechanical interventions on long-term cartilage metabolism in bovine explant
model systems. In addition, this study provides additional evidence that the gadoliniumenhanced MRI method can non-destructively image and quantify glycosaminocglycan
concentration in living cartilage in culture over long time periods and that the shortened NMR
tube culture system used here provides a practical alternative to perfused bioreactor culture
systems. As an adjunct to existing methods, this technique provides a practical means for
studying glycosaminoglycan homeostatis and events that disturb it. Ultimately , studies such as
this provide the foundation for further studies evaluating the effects of potentially therapeutic
interventions on cartilage degradation or regeneration in explant or engineered tissue culture
studies and in vivo animal and human studies.
44
6 Acknowledgements
First, I would like to thank my advisors Martha Gray and Debbie Burstein for their patient
guidance, expertise, support and encouragement. In addition to teaching me about cartilage and
MRI, they taught me to identify important research questions and how to structure experiments
to provide answers. I am greatly appreciative for the time they spent reading and editing drafts
of this thesis, protocols/write-ups and our manuscript.
I am especially indebted to Rachel Oppenheimer. Besides maintaining the samples in culture for
weeks and weeks (even coming into lab on her weekends!!) and running daily media assays,
Rachel taught me how to harvest plugs, mix the media, change the media, image the samples,
process the images, and navigate the nuances of machines and personalities in our laboratory. In
addition to all that, Rachel conducted a portion of these imaging experiments, edited drafts of
this thesis, and was tremendously patient and kind to me.
The generous MATLAB coding assistance of Joseph Samosky pushed my image processing
abilities over critical thresholds and helped me achieve self-sufficiency in coding programs to
analyze these images. I am further grateful to Joe for reminding me of the world beyond the lab
by taking in many hikes, dance concerts and meals with me.
I want to thank Robert Parker for his enthusiastic statistical analysis advice; Charles Raworth for
his NMR tube-cutting expertise; Nina Menezes for her mentorship, friendship, and music; Jeeva
Munasinghe for his MR help and big heart and Becky Sun for always getting me in to see
Martha.
This work was supported by an NIH grant, AR42773; the New England Baptist Bone and Joint
Institute; Martha L. Gray's Taplin Professorship in Medical and Electrical Engineering,
Harvard-MIT Division of Health Sciences and Technology; and the MIT Electrical Engineering
and Computer Science Rosenblith Fellowship.
45
46
7 References
[1]
Hay, E.D. Cell Biology of Extracellular Matrix, Second Edition. Chapter 2, Plenum Press, New York,
1991.
[2]
Lesperance, L., Compositional studies of cartilage matrix using NMR spectroscopy. Doctoral Thesis,
Massachusetts Institute of Technology, 1993.
[3]
Smith, R. L., Degradative enzymes in osteoarthritis. Frontier in Bioscience 4. (1999). d704-712.
[4]
Nerucci, F., Fioravanti, A., Cicero, M.R., Collodel, G., Marcologo, R. Effects of chondroitin sulfate and
interleukin- 1 on human chondrocyte cultures exposed to pressurization; a biochemical and morphological
study. Osteoarthritis and Cartilage, (2000), 8, 279-287.
[5]
Page Thomas, DP., King, B., Stephens, T., Dingle, J.T., In vivo studies of cartilage regeneration after
damage induced by catabolin/interleukin-1. Ann Rheum Dis (1991) 50:2, 75-80.
[6]
Takegami, K., Masuda, K., An, H., Kamada, H., Pietryla, D., Thonar, I. The effect of osteogenic protein-I
on intervertebral disc cells pre-exposed to interleukin-1. 46t Annual Meeting, Orthopaedic Research
Society, March 12-15, 2000.
[7]
Arner, E., Effect of animal age and chrondronicity of interleukin-1 exposure on cartilage proteoglycan
depletion in vivo. Journal of Orthopaedic Research. (1994) 12:321-330.
[8]
Badger, A., Cook, M., Swift, B., Newman-Tarr, T., Gowen, M., Lark. Inhibition of interleukin-1-induced
proteoglycan degradation and nitric oxide production in bovine articular cartilage/chondrocyte culture by
natural hymenialdisine. J. Pharmacol Exp Ther, (1999), 290(2):587-593.
[9]
Fenton, J., Chlebek-Brown, K., Peters, T., Caron, J., Ortho, M. Glucosamine HCL reduces equine articular
degradation in explant culture. Osteoarthritis and Cartilage, (2000), 8(4):258-265.
[10]
Mims, T, O'Grady, C., Marwin, S., Grande, D. Effects of dietary supplements on cartilage metabolism and
its potential role in osteoarthritis. 46t Annual Meeting, Orthopaedic Research Society, March 12-15
(2000).
[11]
Quinn, T. , Maung, A., Grodzinsky, A., Hunziker, E. and Sandy, J. Physical and biologic regulation of
proteoglycan turnover around chondrocytes in cartilage explants: implications for tissue degradation and
repair. Annals of New York Academy of Sciences, (1999), 878:420-421.
[12]
Hollander, A., Pidoux, I., Reiner, A., Rorabeck, C., Bourne, R., Poole, A.R. Damage to Type II Collagen in
Aging and Osteoarthritis Starts at the Articular Surface, Originates Around Chondrocytes, and Extends into
the Cartilage with Progressive Degeneration. Journal of Clinical Investigation. (1995) 96:2859-2869.
[13]
Bashir, A., Burstein, D., Gray, ML, GD-DTPA2 as a measure of cartilage degradation. MRM (1996)
36:665-673.
[14]
Allen, R.G., Burstein, D., Gray, M.L. Monitoring glycosaminoglycan replenishment in cartilage explants
with gadolinium-enhanced magnetic resonance imaging. Journal of Orthopaedic Research. (1999) 17:430-
436.
[15]
Allen, G., Eisenberg, S., Gray, M. Methods for the Quantification of the Biological Response of Cartilage
to Mechanical Deformation. Harvard-MIT Division of Health Sciences and Technology, Cambridge,
Massachusetts; and Department of Biomedical Engineering, Boston University, Boston, Massachusetts.
47
[16]
Billinghurst, R., Wu, W., Ionescu, M., Reiner, A., Dahlberg, L., Chen, J., van Wart, H., Poole, R.
Comparison of the degradation of type II collagen and proteoglycan in nasal and articular cartilages
induced by interleukin-l and the selective inhibition of type II collagen cleavage by collagenase. Arthritis
and Rheumatism. (2000), 43(3):664-672.
[17]
Setton, L., Elliott, D., Mow, V., Altered mechanics of cartilage with osteoarthritis: human osteoarthritis
and an experimental model of joint degeneration. Osteoarthritis and Cartilage. (1999) 7, 2-14.
[18]
Poole, A. R., An introduction the pathophysiology of osteoarthritis. Frontiers in Bioscience 4, (1999)
d662-670.
[19]
Koob, T., Clark, P., Hernandez, D., Thurmond, F., Vogel, K. Compression loading in vitro regulates
proteoglycan synthesis by tendon fibrocartilage. Archives of Biochemistry and Biophysics. (1992) 298:1,
303-3 12.
[20]
Kuettner, K., Scheleyerbach, R., Hascall, V. Articular Cartilage Biochemistry. Raven Press : New York,
1986.
[21]
Bashir, A., Gray, ML, Hartke, J, Burstein, D. Nondestructive Imaging of Human Cartilage
Glycosaminoglycan Concentration by MRI. Magnetic Resonance in Medicine.
(1999). 41:857-865.
[22]
Beekman, B., Verzijl, N., de Roos, J., TeKoppele, J. Matrix degradation by chondrocytes cultured in
alginate: Il-1[Beta] induces proteoglycan degradation and proMMP synthesis but does not result in
collagen degradation. Osteoarthritis and Cartilage. (1998) 6(5):330-340.
[23]
Patwari, P., Kurz, B., Sandy, J., Grodzinsky. A. Mannosarine Inhibits Aggrecanase-Mediated Changes in
the Physical Properties and Biochemical Composition of Articular Cartilage. Archives of Biochemistry
and Biophysics. (2000) 374(l):79-85.
[24]
Kaufman, K., Kai-Nan, A. "Joint-Articulating Surface Motion." Chapter 22. The Biomedical Engineering
Handbook. Ed. Joseph Bronzino. CRC Press, Inc. (1995), pp 3 0 4 - 3 3 2 .
[25]
McCarty, M., Russell, A. Niacinamide therapy for osteoarthritis - does it inhibit nitric oxide synthase
induction by interleukin- 1 in chondrocytes? Medical Hypotheses. (1999) 53(4):350-360.
[26]
Caron, J., Fernades, J., Martel-Pelletier, J., Tardif, G., Mineau, F., Geng, C., Pelletier, J. Chondroprotective
effect of intraarticular injections of interleukin-I receptor antagonist in experimental osteoarthritis:
suppression of collagenase-1 expression. Arthritis and Rheumatism. (1996) 39(9):1535-1544.
[27]
Martin, I., Obradovic, B., Freed, L., Vunjak-Novakovic, G. Method for quantitative analysis of
glycosaminoglycan distribution in cultured natural and engineered cartilage. Annals of Biomedical
Engineering. (1999) 27:656-662.
[28]
Harvey, A., Yu, X., Frolik, C., Chandrasekhar, S. Parathyroid Hormone-(1-34) Enhances Aggrecan
Synthesis via an Insulin-like Growth Factor-I Pathway. J Biol Chem, Vol. 274, Issue 33, 23249-23255,
August 13, 1999.
[29]
Freed, L., Langer, R., Martin, I., Pellis, Vunjak-Novakovic, G. Tissue engineering of cartilage in space.
Proc. Natl. Acad. Sci., (1997) 94:13885-13890.
[30]
Campbell, M., Handley, C., Hascall, V., Campbell, R., Lowther, D. Turnover of proteoglycans in cultures
of bovine articular cartilage. Archives of Biochemistry and Biophysics. (1984) 234(l):275-289.
[31]
Theodosakis, J., Adderly, B., Fox, B. The Arthritis Cure. St. Martin's
Press:New York. 1997.
48
[32]
Altman, R., Hochberg, M., Moskowitz, R., Schnitzer, T. Recommendations for the Medical Management
of Osteoarthritis of the Hip and Knee. Arthritis and Rheumatism. (2000) 43(9):1905-1915.
[33]
McAlindon, T., LaValley, M., Gulin, J., Felson, D. Glucosamine and Chondroitin for Treatment of
Osteoarthritis: A Systematic Quality Assessment and Meta-analysis. JAMA, (2000) 283(11):1469-1474.
[34]
Sahelian, R. All About Glucosamine and Chondroitin. Avery Publishing Group: New York. (1998).
[35]
Furey, Michael J. "Joint Lubrication." Chapter 23. Handbook of Biomedical Engineering. Ed. Joseph
Bronzino. CRC Press, Inc. (1995) pp 333-351.
[36]
Handley, C., Cheng, K. Biological Regulation of the Chondrocytes. Chapters 3, 7,12. CRC Press,
Inc.:Boca Raton. 1992.
[37]
Bank, R., Soudry, M., Maroudas, A., Mizrahi, J., TeKoppele, J. The increased swelling and instantaneous
deformation of osteoarthritic cartilage is highly correlated with collagen degradation. Arthritis and
Rheumatism. (2000) 43(10):2202-2210.
[38]
Temenoff, J., Mikos, A. Review: tissue engineering for regeneration of articular cartilage. Biomaterials.
(2000) 21:431-440.
[39]
Billinghurst, R., Dahlberg, L., lonescue, M. Enhanced cleavage of type II collagen by collagenases in
osteoarthritic articular cartilage. J Clin Invest (1997) 99:1534-1545.
[40]
Maroudas, A., Kuettner, K. Methods in Cartilage Research. Chapters 5, 12, 29, 30. Academic Press:San
Diego, 1990.
[41]
Arner, E., Hughes, C., Decicco, C., Caterson, B., Tortorella, M. Cytokine-induced cartilage proteoglycan
degradation is mediated by aggrecanase. Osteoarthritis and Cartilage. (1998). 6:214-228.
[42]
Bateman, J., Lamande, S., Ramshaw, J. Collagen Superfamily. Chapter 2. Extracellular Matrix, Vol. 2,
Molecular Components and Interactions. Ed. Wayne Comper, (1996).
[43]
Sah, R., Doong, H., Grodzinsky. Effects of compression on the loss of newly synthesized proteoglycans
and proteins from cartilage explants. Archives of Biochemistry and Biophysics. (1991) 286:20-29.
[44]
Caron, J., Fernandes, J., Martel-Pelletier, J., Rardif, G., Mineau, F., Geng, C., Pelletier, J.
Chondroprotective Effect of Intraaarticular Injections of Interleukin-1 Receptor Antagonist in Experimental
Osteoarthritis: Suppression of Collagenase-1 Expression. Arthritis and Rheumatism. (1996) 39(9):15351544.
[45]
Steinmeyer, J., Knue, S., Raiss, R., Pelzer, I. Effects of intermittently applied cyclic loading on
proteoglycan metabolism and swelling behavior of articular cartilage explants. Osteoarthritis and Cartilage.
(1999) 7(2):155-164.
[46]
Walesby, H. A., Rosenbusch, R. F. and Booth, L. C.: In vivo Distribution of Polysulfated
Glycosaminoglycans Into Rabbit Serum, Urine and Superficial Digital Flexor Tendon. Vet. Surg. 27(5):
520, 1998.
[47]
Ratcliffe, A., Azzo, W., Saed-Nejad, F., Lane, N., Rosenwasser, M., Mow, V. In Vivo Effects of Naproxen
on Proteoglycan Metabolism and Matrix Metalloproteinase Activities in Canine Articular Cartilage.
[48]
Stoop, R., Van Der Krann, P., Buma, P., Hollander, A., Poole, A., Van Den Berg, W. Denaturation of type
II collagen in articular cartilage in experimental murine arthritis. Evidence for collagen degradation in both
reversible and irreversible cartilage damage. Journal of Pathology. (1999) 188:329-337.
[49]
Freed, L., Hollander, A., Martin, I., Barry J., Vunjak-Novakovic, G. Chondrogenesis in a cell-ploymerbioreactor system. Exp Cell Res. (1998) 240: 58-65.
49
[50]
Hauselmann, H., Fernandes, R., Mok, S., Schmid, T., Block, J., Aydelotte, M., Keuttner, K., Thonar, E.
Phenotypic stability of bovine articular chondrocytes after long-term culture in alginate beads. Journal of
Cell Science 107(1):17-27.
[51]
Larsson, T., Aspeden, R., Heinegard, D. Effects of Mechanical Load on Cartilage Matrix Biosynthesis In
Vitro. Matrix (1991) 11:388-394.
[52]
Grodzinsky, A., Kim, Y., Buschman, M., Garcia, M., Quinn, T., Hunziker, E. Response of the chondrocyte
to mechanical stimuli. Chapter 7.2.5 in Osteoarthritis. Eds. Brandt, K., Doherty, M., Lohmander, L.
Oxford University Press. 1998.
[53]
Hering, T. Regulation of Chondrocyte Gene Expression. Frontiers in Bioscience 4, (1999) d743-761.
[54]
Maroudas, A., Balance between swelling pressure and collagen tension in normal and degenerate cartilage.
Nature. (1976) 260: 808-809.
[55]
Denko, C., Malemud, C. Metabolic disturbances and synovial joint responses in osteoarthritis. Frontiers in
Bioscience 4. (1999) d686-693.
[56]
William, S., Obradovic, B., Burstein, D., Freed, L., Gray, ML, Langer, R., Vunjak-Novakovic, G. MRI
Measurements of Fixed Charge Density as a Measure of Glycosaminoglycan Content and Distribution in
Tissue Engineered Cartilage. Transactions, 44t Annual Meeting, Orthopaedic Research Society. (1998)
23:203.
[57]
Potter, K., Butler, J., Adams, C., Fishbein, K., McFarland, E., Horton, W., Spencer, R.
Cartilage Formation in a Hollow Fiber Bioreactor Studied by Proton Manetic Resonance
Microscopy. Matrix Biology. (1998) 17:513-523.
[58]
Boustany, N., Gray, ML, Black, A., Hunziker, E. Correlation between synthetic activity and
glycosaminoglycan concentration in epiphyseal cartilage raises questions about the regulatory role of
interstitial pH. Journal of Orthopaedic Research. (1995) 13:733-739.
[59]
Hascall, V., Handley, C., McQuillan, D., Hascall, G., Robinson H., Lowther, D., The effect of serum on
biosynthesis of proteoglycans by bovine articular cartilage in culture. Archives of Biochemistry and
Biophysics. (1983) 224:206-223.
[60]
Sah, RL-Y Biophysical regulation of matrix synthesis, assembly, and degradation in dynamically
compressed calf cartilage [Ph.D. thesis]. Cambridge, Massachusetts, Massachusetts Institute of
Technology, (1990).
[61]
Arthritis Foundation website: www.arthritis.org/Answers/DiseaseCenter/oa.asp, and
www.arthritis.org/answers/drugguide/default.asp#NSAIDs .
[62]
Freeman, MAR. Adult Articular Cartilage. New York,Grune and Stratton, 1972.
50
Appendix A: Derivation of Donnan Electrochemical Equilibrium Relation
At equilibrium, the sum of forces acting on a charged species in solution is 0.
In tissue, these forces include:
1) Electric field force,
f =qE
2) Chemical energy gradient,
f = -kBT
d ln c
d
Assumptions:
" No bulk flow
* Quasi-static approximations are valid
1) Gauss' Law (a volume of charged particles creates an electric field),
V -E = p, = I zFc,
2) Faraday's Law (the magnetic field induced by the electric field is negligible)
-
VxE=-
dptt
~
di
Therefore, the electric field across an interface is represented by:
F = -VP
And, the sum of all forces acting on a charged species in a solution at equilibrium is
-
SF=O=q -
kBT dc
'
c,
dx
At equilibrium, there is NO NET FLUX of any charged species.
No bulk flow = convection = 0
Flux = 0 = drift + diffusion + convection
ucZ - DVc, + 0
N,0 0=
zi
In a tissue at equilibrium, drift balances diffusion:
dx
zj
Apply the quasi-static Faraday relation,
E
=
-V(I,
the Einstein relation,
rearrange to get:
de
-D zIdc1
-RT I dc
dx
uc, z, dx
z,F c, dx
51
D
RT
u
~ F'
and
Integrate to find the Nernst Potential:
d--(x)dx =
RT I dc. dx
z.F c dx
D(x) - (D(-oo) =
V=-RT Inn
Nernst Potential:
zF
R
Inr
ziF
i()
c,
(
Kc
At equilibrium, all charged species in a solution or tissue feel the same electric potential:
V
-RT
cx
= ZFIn
1F caz
=V2=
Rearranged, this is the Donnan Potential:
RT
(E2(
2FIn
2F
C;1
C11,
c0 2 )
Z[
C
(C2b 1
=---)
C
C31,
Definition of Variables:
f
q
kB
T
= electric field strength vector
force
= quantity of electric charge
= Boltzmann constant
absolute temperature
C=
Pu
F
c
zi
p
h
dielectric constant
density of mobile charges
farad, electrical capacitance
= concentration of charged species i, c= ref, ct
=valence of charged species i
= magnetic moment
= magnetic field strength vector
=
=
electric potential
diffusivity of species i
= mobility of species i
= Nernst potential
=
D
u
V
=
52
tissue, cb
=
bath
Appendix B: Derivation of Tissue Fixed Charge Density (FCD)
Donnan Electrochemical Equilibrium Relation, Electroneutrality, and MRI measured
Concentration of Charged Contrast Agent
Method: Use principles of electroneutrality and electrochemical equilibrium to relate known
bath concentrations of a positively charged ion (sodium, Na+) and a negatively charged ion
(chloride, Cl-, or gadolinium, Gd-DTPA- 2) to a measured tissue concentration of the negative
species.
Governing Equations:
1) Electroneutrality, no net charge in the tissue. (The sum of all fixed and mobile charges
in a tissue is zero; a tissue is electrically neutral only after fully equilibrating with its
bathing solution.)
I zici = 0 = FCD, - [Na ], + [ClJ, + 2[Gd
2
], + [other ch arged species]
Note: Under normal physiologic conditions, the concentrations of sodium and chloride in
the tissue are much greater than the concentrations of other mobile charged species.
e
z
other charged species have a negligible effect on net tissue electroneutrality
[Gd-2 ]t and [other]t can be ignored in the description of tissue electroneutrality
Therefore, in tissue,
I zc, = 0 ~ FCD, - [Na+], + [Cl~ ],
2) Ideal Donnan Theory, description of charged species distribution across an interface
Assumptions:
" the electrical environments on each side of the interface are spatially
homogeneous
* electrical inhomogeneities at the interface are confined to a small region*
small region = debeye length - K
F
2
8nm
" the interface region is small enough to be ignored
Donnan Electrochemical Equilibrium Relation (see derivation in Appendix A):
= cons tan t
C,,,
-
C1=
(C2b 1
C1) )
53
C31,
For a physiologic saline or media solution containing the charged contrast agent Gd-DTPA-2, the
Donnan relation can be written as:
C[
Na'],
1
cc
S
[Gd
[C-],
],
[ Na*]b)
Solve for concentrations sodium and chloride in tissue in terms of the assumed tissue
concentration of contrast agent and known bath concentrations of other ions.
[Na ] =
2
[ Na ]h )[Gd],
2
[G ],
[C-[]d =l
V[Gd -2],I
[Cl-
],
'
[ Gd -2
[ Gd- 2 ]
Combine Electroneutrality and Donnan relations:
0 ~ FCD -[Na+ ], +[Cl- ],
0~dFCD
],, [Gd- ],
[Cl-
[Na+]b [Gd]b
+
[Gd -2,
[Gd ]
Note: bath concentration of sodium is equal to the bath concentration of chloride
])
FCD, = [Na+]i{
->
->
FCD, = -[Na+ ]b
[Gd-2 ]
[Gd-2
[Gd- 2 ]
[Gd-2
S[Gd-2 ]
[d-1
[Gd]
[Gd-2]
[Gd-
Experimental results have shown that this expression underpredicts cartilage tissue FCD by a
factor of 2. Therefore, in order to match true cartilage FCD, this expression is scaled by an
empirical factor of 2.
2
FCD = - [ Na] r
e
[Gd-2]b
Gd]-2 ]
[Ghar
)[Gd-2],
Definition of Variables:
ci
Zi
= concentration of charged species i,
ct = in tissue,
cb =
in bath
= valence of charged species i
FCDt = fixed charged density of tissue
[Na+]t = concentration of sodium in tissue,
[Cl~]t = concentration of chloride in tissue,
[Gd-2 ]t = concentration of Gd-DTPA 2 in tissue,
54
[Na*]b = conc. of sodium in bath,
[Cl-]b = conc. of chloride in bath,
[Gd- 2]b =conc. of Gd in bath,
ZNa
ZCi = -I
ZGd=
-2
Appendix C: Codes for T1 Maps
I. MATLAB code to create a TI map from Inversion Recovery Experiments
%
0
excised_ti_map_ir.m
Program to create T1 map from multiple T1 inversion recovery images in
a Paravision 2dseq file
Author unknown
echo off
clear
close all
clc
scale
=
sname =
Se6;
%set to 5e6 for 1mM Gd;
input('File
used to
save the t1 map:
9e6
for no Gd
','s');
sizi
= 128;
siz2 = 128;
noofti = 9;
data =
fopen('2dseqTlO9l900a',
file name to fit
imas = fread(data, [sizl*siz2
fclose (data);
'r',
'b');
no of ti]
,'long');
clear data;
imas = imas./scale;
for n = 1:noofti,
ima = reshape(imas(:,n),siz1,siz2);
ima = flipud(rot9o(ima));
imal = medfilt2 (ima, [2 2])
I(:,n) =
imal(:);
end
colormap(gray)
imshow(imal,gray);
mask = roipoly;
mask = double(mask(:));
clear Im Jm Vm
tempi = I(:,no of ti).*mask;
[Im Jm Vm] = find(tempi < 4);
for n = 1:size(Im,l),
mask(Im(n))
= 0;
end
for n =
1:no of ti,
Imasked(:,n) = I(:,n).*mask;
end
clear I ima imas mask scale siz n
55
%use 'b'
for PC, input
[I,
J, V]
=
find(Imasked(:,noofti));
for n = 1:noof ti,
Data(:,n) = Imasked(I,n);
end
clear Imasked J V
iniguess = [35 1 0.35);
TI = [0.00667 0.02333 0.04 0.05667 0.09 0.14 0.24 0.39 0.59];
%VDlist as used in Paravision
TI = TI + 0.01;
%TR as used in Paravision:
TR = 1000;
1000 for 1mM
Gd, 6000 for no Gd
OPTIONS = 0;
s = size(Data,1)
pfitted = zeros(s,3);
for n = 1:s,
%find T1 with external minimization function
SI = Data(n,:);
n;
pfitted(n,:) = fmins('excised_tifun ir',iniguess,OPTIONS, [],SI,TI,TR)
end
ti ima = zeros(sizl,siz2);
tlima = tiima(:);
pfittedbackup = pfitted;
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%o%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
clear testl spots
tlupper bound = .6;
%use 0.6
for 1mM Gd
spots = find(pfitted(:,3) > t1_upper bound);
testi = isempty(spots);
if testi == 0;
for n = 1:size(spots)
pfitted(spots(n),3)=0;
end
end
clear testi spots
tilowerbound = .05;
%use 0.05 for 1mM Gd
spots = find(pfitted(:,3) < tllowerbound);
testi = isempty(spots);
== 0;
for n = 1:size(spots)
if testl
pfitted(spots(n),3)=0;
end
end
%--------------------------------------------------------------------------
clear testi spots
mupper bound = 100;
56
spots = find(pfitted(:,1) > mupperbound);
=
testl
isempty(spots);
== 0;
n = 1:size(spots)
if testi
for
pfitted(spots(n),3)=0;
end
end
clear testl spots
m_lowerbound = 0;
spots = find(pfitted(:,1)
testl = isempty(spots);
if testl ==
for n
< mlowerbound);
0;
= 1:size(spots)
pfitted(spots(n),3)=0;
end
end
----------------------------------------------------------------------------clear testl
spots
a upperbound = 2;
spots = find(pfitted(:,2)
testl
= isempty(spots);
if
testl
==
> aupperbound);
0;
for
n = 1:size(spots)
pfitted(spots(n),3)=O;
end
end
clear testl
spots
a_lowerbound = 0.25;
spots =
testl
if
find(pfitted(:,2)
<
alowerbound);
= isempty(spots);
testl
==
for
0;
n = 1:size(spots)
pfitted(spots(n),3)=0;
end
end
tlvalues
tlima(I)
tlima
= pfitted(:,3);
= tlvalues;
=
1000*tlima;
t1_ima = reshape(tima,
siz2,
sizl);
save(sname,'tlima');
figure
imshow(tlima,hot(2500));
57
I. MATLAB code to create a T1 map from Saturation Recovery Experiments
%
excised_ti_map_sr.m
%
%
Program to create T1 map from multiple T1 saturation recovery images in
a Paravision 2dseq file
%
Author unknown
echo off
clear
close all
clc
scale = 2e6;
sname = input('File used to save the tl map:
sizl = input('Matrix Size [128]: ');
','s');
(length(sizl)==0 I sizl<=0),
if
sizl=128;
end
siz2=sizl;
no of slices = input('No. of slices [1]: ');
if (length(noofslices)<=0
no-ofslices<=0),
1;
noofslices =
end
noofTR = input('No.
of TR [10]: ');
if (length(noofTR)<=0 I no_ofTR<=0),
noof TR = 10;
end
TR=input(['TR =
('
int2str(no ofTR) ')
values
[25 75 125
175 275 375 475
900
1800]'1);
if (length(TR)==0 I TR(1)<=0),
TR=[25 75 125 175 275 375 475
600 900 1800];
end
initial guesstl =input(['Initial Guess for T1 =
[400]
if
:]);
(length(initial_guess_tl)==0 I initial_guess_t1(1)<=0),
initialguess tl=[400];
end
initialguess = [1 initialguess ti];
noise level = input('Noise blanking level[10]:
if (length(noiselevel)<=0 I noiselevel <=0),
noiselevel
end
noofimages
=
=
');
10;
noofslices
.*
noofTR
[fname path]=uigetfile('*','Please Select File');
data = fopen([path fname],
ima
=
'r','b');
fread(data, [sizl*siz2 no of-images],'long');
ima = ima./scale;
58
600
fclose(data);
clear data;
clear temp
% if first image is longest TR then uncomment the following line
%temp = reshape(ima(:,1),siz1,siz2);
%if last image is longest TR then uncomment the following line
temp = reshape(ima(:,noofTR),sizl,siz2);
**
%-** * ***
*
**
***
***
*******
***
**
*
***
*
****
***
* ********
****
****
***
*
**
temp = flipud(rot90(temp));
colormap(gray(255));
imshow(temp, gray (255))
mask = roipoly;
mask = double(mask(:));
clear temp
tiima = zeros(sizl*siz2,noofslices);
for m
1:noofslices,
=
for n
1:noofTR,
=
temp
temp
reshape(ima(:, (noofTR*(m-1)) + n),sizl,siz2);
flipud(rot9C(temp));
I(:,n) = temp(:);
=
=
end
clear templ
*****************************
9-*** ********************************
% if first image is longest TR then uncomment the following line
%templ = I(:,1).*mask;
% if last image is longest TR then uncomment the following line
tempi = I(:,noofTR).*mask;
**
***
****
roind =
* ****
****
***
find(templ
* ***
* ****
**
*****
**
*************
> noise-level);
clear Data
for n
=
1:noofTR,
= I(roind,n);
Data(:,n)
end
OPTIONS
=
s =
(Data,1)
size
0;
clear pfitted
pfitted = zeros(s,2);
strl=[' of total ' int2str(s)
for n
=
pixels'];
1:s,
SI = Data(n,:);
initial guess(l) = max(SI);
59
**
******
***
:)
= fmins('excised_tifunsr'
pfitted(n,
if n==10*round(n/10),
fprintf(1, ['finished ' int2str(n) strl
end
,initial-guess,OPTIONS,
'\n']);
end
clear ti values
t1_values = pfitted(:,2);
tlima(roind,m) = tlvalues;
end
ti ima = reshape(tlima,sizl,siz2);
save(sname,'tl ima');
imshow(tlima,hot(2500));
III. MATLAB TI finding function for IR and SR T1 fit programs
function f = excised-t1_fun
err
f =
= SI - abs( p(1)
sum(err.^2);
*
(1
-
ir(p,SI,TI,TR)
2*p(2)*exp(-TI/p(3))
60
+ exp(-TR/p(3))));
[I] ,SI,TR);
Appendix D: MATLAB Code to Scale T1 Maps Before Registration
%
%
%
%
%
scale_timaps.m
contained in the current directory
Input: The .mat files
Output: A new set of files containing scaled, unsigned byte data.
Program to scale tl maps to range of 0 to 255, and save as
new files.
% Program should be run from a directory containing a series of .mat
% files; each .mat file contains a tl map stores in an N x N array
% named t1_ima
% Author:
Joe Samosky
5/21/00
% Rev 1.0
clear;
imagesize =
%
%
%
%
128 *
128;
Set these values to establish the range of the input data mapped to the
output.
All input values <= lowerthreshold will be mapped to 0 in the
scaled output files. All input values >= upperthreshold will be mapped
to 255 in the scaled output files.
lowerthreshold = 220;
upper-threshold = 650;
% use 220 for Spring, 200 for fall
% use 650 for Spring, 600 for fall
scale = 255/(upperthreshold - lowerthreshold);
% Get name of current directory
p
=
cd;
% Create structure containing names of all Matlab files in current directory
matlabfiles = what(p);
= size(matlabfiles.mat, 1);
numberoffiles
% Open each input .mat file, load the tlima image, scale it, then save
% the scaled data as a new file containing N * N unsigned bytes.
for i=1:number of files,
load(matlabfiles.mat{i});
tiima = (tlima - lowerthreshold) *
tlima = round(tlima);
tiima(find(tl_ima < 0)) = 0;
tlima(find(tlima
> 255))
scale;
= 255;
% Transpose the image.
Matlab reads and saves arrays by "column-order", most
% other image-manipulation programs read and save images by "row-order". Thus
% when Matlab saves an image array to disk the image will be read in a
% transposed orientation by most other image programs.
Since the .scale
% files created by this program will be read by Photoshop, we transpose the
% image array prior
to writing to disk.
tlima = tl ima';
61
savefilename = [strtok(matlabfiles.mat{i},
outfile id = fopen(savefilename, 'w');
fwrite(outfileid, tiima,
'.')
'uint8');
fclose(outfileid);
end
disp([num2str(i)
disp('
'
files were just written to disk.']);
');
disp('Heya!
All done...have a really super-nice day!');
62
'.scale'];
Appendix E: MATLAB Code to Calculate Mean [GAG] in a Sample
%
Ashley Williams, May 23,
%
%
%
Program to find average value of pixel intensity over a small region.
Input image must be a T1 map.
Output image will be a GAG map.
2000
echo off
clear
R=4.5;
T1=1.4;
Gdbath=1.0;
% relaxivity for Magnevist at 8.45T
% good guess for tissue T1 without Gd, use 1.6 for fall
% concentration of Gd in bath, CHANGE AS NECESSARY
% These two values are defined in scale_tlmaps. The values here must be made
% the same as the values used in scale tlmaps at the time the input files
were
% created.
lowerthreshold = 220;
%set to
200-600
for August 2000, 220-650
for Spring
upper-threshold = 650;
inverse-scale
=
-
(upperthreshold
lower-threshold)
/255;
* Get the reference image name and image dimensions.
[refimagename ref imagepath] = uigetfile('*', 'Please select reference image');
refimagefullname = [refimagepath refimagename];
size x = input ('Enter the horizontal dimension of the images:
size-y =
input
(' Enter
image-size = sizex *
the vertical
dimension
'
reference fid = fopen(refimagefullname,
pixels]
images:
')
');
size-y;
% Read in the reference image file.
message = ['Reading in reference image
disp (message);
[temp image,
of the
'r');
= fread(reference_fid,
fclose(referencefid);
pixelss = sprintf('%d', pixels);
disp([pixelss
' pixels read from
ref imagename]
imagesize,
'
'uint8');
refimagename]);
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
6 Convert the one-column input image to an appropriately dimensioned 2D array
input_image (:, :) = reshape (tempimage, sizex, size-y) ' ;
% Re-scale the input data values from [0 255]
lowerthreshold)]
inputimage = inverse-scale * inputimage;
%Change input_image
data
to
range
from
to [0
[lowerthreshold
nonzeroregion = find(inputimage > 0);
inputimage(nonzeroregion) = inputimage(nonzero
tldisplay image = inputimage (:,:);
63
(upper-threshold -
-
region)
upperthreshold]
+ lower-threshold;
%Convert
inputimage from a T1 map to a
[GAG]
map
Gdt=(l./R).*(1000./input_image-l./Tl);
FCD=2.*150.*((Gdt./Gdbath).^0.5-(Gdbath./Gdt).^0.5);
GAG=-0.5.*0.5025.*FCD;
inputimage = GAG;
% Take care of the NaNs created by the above equations
input_image(find(isinf(input_image))) = 0;
GAGimage=input_image;
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
% Display GAG Map
5e6;
clear I
I = GAGimage;
scale =
GAG_min = min(GAGimage(:));
GAG-max = max(GAG image(:));
figure;
imagesc(I,([GAG_min GAGmax]));
titlestring = 'GAG Map:
title(titlestring);
axis (' image');
grid
colorbar;
% This section allows the user to zoom into a desired region of the image
% by left-clicking. Double click to return to full image.
Strike any key
% to stop the zoom and start choosing an area for GAG calculation. Left click
% to choose the perimeter of desired area.
response = input
('Find
while response == 'y'
average GAG in
Double click to finish selection.
a region?
[y/n]
',
's');
echo on
zoom on
pause % use left mouse button to zoom and strike any key to continue
zoom off
echo off
mask = roipoly;
mask = double(mask(:));
I
=
I()
%%%%%%%%%%%%%%000
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
% This section eliminates areas outside of tissue from average
% Lower bound can be used as a threshold value [ **if thresholding
% has not already been done while scaling tl images!Ito eliminate media
% from averaging process - don't increase above 1 if data is already scaled
64
= I.*mask;
lowerbound = 1;
tempi
< lowerbound);
l:size(Im,1),
mask(Im(n))
= 0;
[Im]
find(templ
=
for n
=
end
clear Im
upper bound = 150;
[Im] = find(tempi >
for n
upper-bound);
1:size(Im,1),
mask(Im(n)) = 0;
=
end
[Im]
%
=
find(mask);
Perform calculations on selected area.
GAGvalues = GAGimage(Im);
avg-in-mg-per ml = mean(GAGvalues)
sd = std(GAGvalues)
end
figure;
imshow(GAGimage, [],'notruesize');
titlestring = 'GAG Map (greyscale)
title(titlestring);
axis('image');
grid
colorbar;
65
Appendix F: MATLAB Code for Regional Analysis
%
%
%
%
%
reg.m
Program to clip out the blood vessels from a GAG image, cut out the
surrounding media,determine high, low, med GAG regions based on remaining
pixels of the last inputted image and follow those regions in time.
Ashley Williams, 10/27/00
clear
echo off
R=4.5;
T1=1.6;
% relaxivity for Magnevist at 8.45T
% good guess for tissue T1 without Gd
% use 1.6 for 20 ng/ml, 1.4 for 10 ng/ml
% Get number of images and sizes.
numberof_images = input('How many images will be input?
disp(['Choose images in chronological order '])
');
size x = input('Enter the horizontal dimension of the images:
sizey = input('Enter the vertical dimension of the images:
')
');
imagesize = size x * sizey;
displayimage = zeros(sizey, number ofimages*size x);
0000000000000000000000000000000000%000000000000000000
% Define high contrast colormap for GAG display
cml = imadjust(gray(1)
, [0,1], [0,1],1);
cm2 = imadjust(jet(100), [0,1], [0,1],1); cm=[cml;cm2(1:100,:)];
%
%
%
%
Turn chosen tl maps into GAG maps with the scaling and [Gd]bath appropriate
to each.
Upper and lower threshold values are defined in
scale_tlmaps.
The values here must be made the same as the values used in
scale_tlmaps at the time the input files were created.
for i=1:numberof_images,
[imagename{i} inputimagepath]
number
'
num2str(i)
=
uigetfile('*,
['Please select image
':
cd(inputimagepath);
Gdbath = input('Enter Concentration of Gd in bath: ');
lowerscale = input('Lowerthreshold for image: ')
upperscale = input('Upper threshold for image: ');
inversescale=(upper_scale-lowerscale)/255;
message = ['Reading in image number ' num2str(i)
':
' imagename{i}]
disp(message);
input_fid(i) = fopen(imagename{i}, 'r');
[tempimage, pixels] = fread(inputfid(i), imagesize, 'uint8');
pixelss = sprintf('%d', pixels);
disp([pixels_s ' pixels read from ' imagename{i}]);
% Convert the one-column input image to an appropriately dimensioned 2D image.
input_image = reshape(temp_image, size x, sizey)';
tlmap = inversescale * inputimage;
nonzero-region = find(tl_map > 0);
tlmap(nonzeroregion) = ti_map(nonzeroregion) + lower-scale;
66
%Convert inputimage
from a T1 map to a
[GAG]
map
Gdt=(1./R).*(1000./t1_map-l./Tl);
FCD=2. *150.*((Gdt./Gdbath).^0.5-(Gdbath./Gdt).^0.5);
GAG=-0.5.*0.5025.*FCD;
GAGimage = GAG;
% Take care of the NaNs created by the above equations, which generate
% them by the boatload in an obscure and non-reproducible manner
GAGimage(find(isinf(GAGimage))) = 0;
GAGmap(:,:,i)= GAGimage;
end
% Clip away the
surrounding media
clear I
I = GAGmap (:,:,1);
figure(1);
imshow(I,cm);
titlestring
=
'Draw around the plug excluding media:
title(titlestring);
axis('image');
grid
colorbar;
00000000%%%%%%00%0%0%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
%
%
%
%
This section allows the user to zoom into a desired region of the image
by left-clicking. Double click to return to full image.
Strike any key
to stop the zoom and start choosing an area for GAG calculation. Left click
to choose the perimeter of desired area.
Double click to finish selection.
echo on
zoom on
pause % use left mouse button to zoom and strike any key to continue
zoom off
echo off
mask = roipoly;
mask = double(mask(:));
for i=1:numberofimages;
outside=-1000*ones(sizex,size_y);
%make area surrounding plug -1000
[Im] =
find
(mask);
outside(Im)= 0;
GAG-map(:,:,i) =GAGmap(:,:,i) +outside;
end
figure(2)
imshow(GAG-map(:,:,l),cm,'notruesize');
title('GAG map after cutting out the surrounding media');
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
%%%%%%%%%
67
%Now Clip out the vessels
numberofvessels = input('How many vessels will be clipped?
for j=2:numberofvessels+1;
');
clear I
I = GAGmap(:,:,1);
GAG-min = min(GAG_map(:));
GAGmax = max(GAG_map(:));
figure(3);
imagesc(I,([0 GAGmax]));
title string = 'Draw Around Each Vessel to be Removed from Image:
title(title string);
axis('image');
grid
colorbar;
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
%
%
%
%
This section allows the user to zoom into a desired region of the image
by left-clicking.
Double click to return to full image.
Strike any key
to stop the zoom and start choosing an area for GAG calculation. Left click
to choose the perimeter of desired area. Double click to finish selection.
echo on
zoom on
pause % use left mouse button to zoom and strike any key to continue
zoom off
echo off
mask = roipoly;
mask = double(mask(:));
for i=1:numberof_images;
areaofinterest(:,:,i,l)=GAG map(:,:,i);
new image=areaofinterest(:,:,i,j-1);
[Im] =
find(mask);
newimage(Im) = -10;
%make area inside vessels =
areaofinterest(:,:,i,j) = new-image;
end
end
%
-10
Define Low, Med, High GAG values using last inputted image
finalpixels = areaofinterest(:,:,numberof images,numberofvessels+l);
[impix] = find(finalpixels>-9);
finalvalues = final pixels(impix);
[a,b,finaljpix]=find(finalvalues);
finalaverage = mean(final_pix);
finalstd = std(final_pix);
maxlowgag = final average-(.5*finalstd);
minhighgag=finalaverage+(.5*finalstd);
0%%%%%%%%%%%%%%0%%%%000%0%00%0%0%%%%0
0%%00%%0%0000%0%0%00%0%
68
in the last inputted image
%
Find the High, low, med GAG regions
%
Make masks for display of these regions
= areaof
clippedmap
(week 3).
: , numberof_images, numberofvessels+1)
interest(:,
lowmap=-1000*ones(sizex, size_y);
medmap=-1000*ones(sizex, size_y);
highmap=-1000*ones(sizex, size_y);
%low map shows low GAG regions of wk 3
%med map shows med GAG regions of wk 3
Thigh map shows high GAG regions of wk 3
templ=zeros(sizex, size_y);
% templ,2,3 to use for display only
temp2=zeros(sizex, size_y);
temp3=zeros(sizex, size_y);
% Don't use these masks
for calculations!
for p=1:size-x*sizey,;
if clipped map(p) >-9;
lowmap (p)=clippedmap (p);
tempi (p) =1;
end
if clipped map(p) > maxlowgag;
lowmap(p)= -1000;
medmap(p) = clipped map(p);
templ (p) =0;
temp2 (p) =1;
end
if clipped map(p)> minhighgag;
medmap(p) =
highmap(p)
-1000;
=
clipped map(p);
temp2 (p) =0;
temp3 (p)=1;
end
end
% Find average and std of non-zero low, med, high GAG pixels in all images
% from which vessels have been removed
for i=1:numberofimages;
allpixels=areaof interest
[Imlow]
=
(:,
:,i, numberofvessels+1);
find(lowmap>-9);
[Immed] = find(medmap>-9);
[Imhigh] = find(highmap>-9);
lowmapvalues= allpixels(Imlow);
medmapvalues=allpixels (Immed);
highmapvalues = allpixels(Imhigh);
69
lowave(:,i) = mean(lowmapvalues);
medave(:,i)
= mean(medmapvalues);
high_ave(:,i) = mean(highmapvalues);
lowsd = std(lowmapvalues);
medsd = std(medmapvalues);
highsd =std(highmapvalues);
output(i,
:)=[low_ave(:,i) ,high_ave(:,i)]
lowGAGmap(:,:,i)=areaofinterest(:,:,i,numberofvessels+1).*templ;
medGAGmap(:,:,i)=areaofinterest(:,:,i,numberofvessels+l).*temp2;
highGAGmap(:,:,i)=areaofinterest(:,:,i,numberof vessels+1).*temp3;
end
%
%
Now display original GAG image series, GAG series with vessels and
surrounding media clipped, low GAG series, high GAG series
for i=l:numberof_images,
original(:,
(sizex*(i-l)+l):(sizex*i)) = GAGmap(:,:,i);
multi imagetop(:, (size x*(i-1)+l):(size x*i)) = areaofinterest(:,:,i,j);
multi imagemiddle(:, (sizex*(i-1)+1):(sizex*i)) = lowGAGmap(:,:,i);
multi image-bottom(:, (sizex*(i-1)+1):(sizex*i)) = highGAGmap(:,:,i);
end
figure(4);
multi display(:,:)=[original;multi imagetop;multiimage middle;multi imagebo
ttom];
imshow(multi display(:,:),cm, 'notruesize');
titlestring =
'Pixels of Initially Low or High GAG Followed:
title(titlestring);
axis('image');
colorbar;
save novessels
70
Appendix G: MATLAB Code to Analyze [GAG] in Pixels Near Blood Vessels
%0.
%6
%6
surround.m
Program to determine the relative distribution of low, med, high
in pixels surrounding blood vessels.
Ashley Williams, 11/14/00
%%%%%%%%%%%%%%%%%%%%%obob@0000%ooo
000%%%%%%%%%%%%%%%%%%%%%%%%%
[GAG]
%
clear
close all
echo off
R=4.5;
T1=1.4;
% relaxivity for Magnevist at 8.45T
% good guess for tissue T1 without Gd
% use 1.6 for 20 ng/ml, 1.4 for 10 ng/ml
% Get number of images and sizes.
numberofimages = input('How many images will be input?
disp(['Choose images in chronological order
');
'])
size x=128;
sizey=128;
%size x = input('Enter the horizontal dimension of the images: ');
%size y = input('Enter the vertical dimension of the images: ')
image size = size x * sizey;
display-image = zeros(size_y, numberof images*sizex);
%
Define high contrast colormap for GAG display
cml = imadjust(gray(1) , [0,1], [0,11,1); %[0.02,1]
cm2 = imadjust(jet(150) , [0,11, [0,1] ,);
%[0.025,1]
cm=[cml;cm2(1:150,:)];
LOW = 35;
%use 100, 25, 70, 85 for fall data; 150, 35, 100, 140 for spring
MEDIUM = 100;
HIGH = 140;
%
%
%
Turn chosen ti maps into GAG maps with the scaling and
[Gd]bath appropriate
to each. Upper and lower threshold values are defined in
scale_timaps. The values here must be made the same as the values used in
71
%
scale_timaps at the time the input files were created.
for i=l:numberof_images,
[imagename{i} inputimagepath]
= uigetfile('*',
number
'
['Please select image
':
']);
num2str(i)
cd(inputimagepath);
Gdbath = input('Enter Concentration of Gd in bath: ');
lowerscale = input('Lowerthreshold for image: ')
upperscale = 600; %600 for fall, 650 for spring
inversescale=(upperscale-lowerscale)/255;
message = ['Reading in image number ' num2str(i) ': ' imagename{i}]
disp(message);
input_fid(i) = fopen(imagename{i}, 'r');
[tempimage, pixels] = fread(inputfid(i),
pixelss = sprintf('%d', pixels);
disp([pixelss ' pixels read from
'
imagesize, 'uint8');
image_name{i}]);
% Convert the one-column input image to an appropriately dimensioned 2d matrix
inputimage = reshape(tempimage, sizex, size_y)';
timap = inversescale * inputimage;
find(tl_map > 0);
timap(nonzero_region) = tlmap(nonzeroregion) + lower-scale;
nonzeroregion =
%Convert inputimage from a T1 map to a [GAG] map
Gdt=(1./R).*(1000./tl _map-1./T1);
FCD=2.*150.*((Gdt./Gdbath).AO.5-(Gdbath./Gdt).^A.5);
GAG=-0.5.*0.5025.*FCD;
GAGimage = GAG;
% Take care of the NaNs created by the above equations, which generate
% them by the boatload in an obscure and non-reproducible manner
GAG image(find(isinf(GAG image))) = 0;
AG map(:,:,i)= GAG-image;
end
000000000%0%00%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
%Clip away the media
clear I
I = GAG_map (:,:,1);
GAG_min = min(GAGmap(:));
GAG-max = max(GAGmap(:));
72
figure(1);
imshow(I,cm);
titlestring
=
'Draw around the plug excluding media:
';
title(titlestring);
axis('image');
grid
colorbar;
%
%
%
%
This section allows the user to zoom into a desired region of the image
by left-clicking. Double click to return to full image. Strike any key
to stop the zoom and start choosing an area for GAG calculation. Left click
to choose the perimeter of desired area. Double click to finish selection.
echo on
zoom on
pause % use
left mouse button to zoom and strike any key to continue
zoom off
echo off
mask = roipoly;
mask = double(mask(:));
for
i=1:numberofimages;
%make area surrounding plug negative
outside=-1000*ones(sizex,size_y);
[Im] =
find
(mask>0)
outside(Im)= 0;
GAGmap(:,:,i) = GAGmap (:,:,i) +outside;
end
figure(2)
imshow(GAG-map(:,:,l),cm,'notruesize');
title('GAG map after cutting out the surrounding media');
%Now Clip out the vessels
number of vessels = input('How many vessels will be clipped? ');
for j=2:numberofvessels+l;
clear I
I = GAGmap(:,:,1);
GAG_min = min (GAG-map(:));
GAGmax = max(GAG-map(:));
figure(3);
imagesc (I, ([0 GAGmax]));
title string =
'Draw Around Each Vessel to be Removed from Image:
title(titlestring);
axis ('image');
grid
73
';
colorbar;
% This section allows the user to zoom into a desired region of the image
Strike any key
% by left-clicking. Double click to return to full image.
% to stop the zoom and start choosing an area for GAG calculation. Left click
% to choose the perimeter of desired area.
Double click to finish selection.
echo on
zoom on
pause % use left mouse button to zoom and strike any key to continue
zoom off
echo off
mask = roipoly;
mask = double(mask(:));
for i=l:numberof_images;
areaofinterest(:,:,i,l)=GAG map(:,:,i);
newimage=areaofinterest(:,:,i,j-1);
[Im]
=
find(mask);
newimage(Im) = -5-(j-l)*5;
% give each vessel its own negative value
areaofinterest(:,:,i,j) = new-image;
end
end
%
Use last inputted image to define low, medium, high GAG
finalpixels = areaofinterest(:,:,numberofimages,j);
[impix]
= find(final-pixels>-l);
finalvalues = finalpixels(impix);
[a,b,final-pix]=find(finalvalues);
finalaverage = mean(finalpix);
74
-a947
5
TT
A9T~qTjpS
PGA1eTdsTp
AM
P 04 GSO[O 4OU ST TaxTd ;alq jI
(STXTd E txTtL4TM) S9SS9A "e 04 GSOTO
GLI14 '
SUOTf5a.
OE
mOT
'UWnTpaU
't{5ttI UT
q%~~
ST
UOTS62I
I
d'eIUTT4I=d
9q'j9SS9A
9 1T4LtJTjS PGAL-TdsTp ST UoTf5a
JI
(T~xTdT) UTior5a 9~
ST
sTaSSGA
0
;o AlTuaTXOad 9Lfl
ND91q
%
%
%
%
!T9.9.99.9.9.99.9.9.9.9.9.09000009
AT~ad~s
T9SS9A
TqOVG
pufloat
XoaD~.%
PUG
PUG
!HDIH
=
(d)d-eluTMq
!&6-e5tTj6TM~uTr < (d) dplupaddTTD
JT
PUG
~w~itaw
!E1?5mOTxtu1 <
=(d)deu'Tut
(d)dupaddTTO
9T
PUG
!mcYI =
(d)dvunnTT
0OT -< (d) dvupadd-T
~T
(d) d-ew-padd-TO= (d) dL-wtuTT4
!6->(d)d-euipadd-TD
!'A-aZTs~X - zTS:T=d
JT
a0J
SUOTBGt
OJVD PTUI PUP
(A79z's
'mOT'qT~tl jo dpua sT dPmtuTT%
!(~~saz-oaq
(z Nfam) af~pwT paqqnduT
4 S4P
'X-GzTs)s~UO*OOOT-dVU1U1T
)
us~w-oaqnl':
T aqiuoT69jE DeV
qsaauTgopatp = dIpw-ddTTO
uwniptu
'LMSTH
'MaT
%
aLfl PuT
5
~(Ps-TPUTEJ*S *) +G~vaAvTPuT;=6T
TtUTtu
(ps TLPUTJ;S') -GEP2E9APTTJ=PMTXU
Pqs
(xTd-Tvul)Pqs =
TvuTJ
hlmmap2=hlmmap;
for i=1:128,
for j=1:128;
if p(i,j) == -1000,BREAK;
for t=2:numberofvessels+1
if
p(ij)==(-5-(t-1)*5),
BREAK;
end
end
else
NEAR = 0;
%-.= FALSE
:(i+3)
for
ii=(i-3)
for jj=(j-3):(j+3);
if ii<=0, BREAK;
elseif
jj<=
%a
%c
%c
%a
%5
%6
0, BREAK;
elseif ii>=128, BREAK;
elseif jj>=128, BREAK;
elseif p(ii,jj)==(-5-(q-1)*5);
NEAR=1;
end
end
end
if
%2
%3
p(i,j)==LOW,
if NEAR==O;
hlmmap2 (i, j)=LOW+5;
else hlmmap2 (i, j )=LOW-5;
%In a Vessel?
%1- 1 = TRUE
%06
%5
%-o4
%7
%8
end
elseif
p(i,j)==MEDIUM,
if NEAR==0;
hlmmap2 (i, j)=MEDIUM+5;
else hlmmap2 (i, j )=MEDIUM-5;
end
elseif p(i,j)==HIGH,
if NEAR==0;
hlmmap2 (i, j)=HIGH+5;
else hlmmap2 (i, j)=HIGH-5;
end
end
%10
%10
%*.7
%03
end
end
end
vesselmap
(:,:,
(q-1))=hlmmap2;
% Count pixels that are near to vessels by low, medium, high GAG groupings
low GAG near vessels=size (find(hlmmap2==LOW-5));
medGAGnear vessels=size (find (hlmmap2==MEDIUM-5));
highGAGnearvessels=size (find (hlmmap2==HIGH-5));
totpixelsnearvessels=lowGAGnearvessels
(:,1) +medGAGnearvessels (:,1) +hi
ghGAGnearvessels(:,l);
percentlownearvessels=100*lowGAGnear_vessels(:,l)/totpixelsnearvessels
percent mednearvessels=100*medGAGnearvessels(:,l) /totpixels near vessels
76
percent_highnearvessels=100*highGAG_nearvessels(:,1)/tot_pixels near vesse
tot_pixelsnearvessels;percentlownearvessels;
percentmednear vessels;percenthighnearvessels]
',output);
%fprintf('%6.0f\r
output(:,q-l)=
% Count total
by low,
pixels
medium,
high GAG groupings
lowGAGnotnear=size(find(hlmmap2==LOW+5));
(find (hlmmap2==MEDITM+5));
medGAGnotnear=size
(find (hlmmap2==HIGH+5));
high_GAGnotnear=size
(:,1) ;
(:,1) +lowGAGnotnear
totlow=lowGAGnearvessels
totmed=medGAGnearvessels (:,1) +med_GAGnotnear(:,1) ;
(: , 1) +highGAG not
near (: , 1);
tothigh=highGAGnearvessels
totpixels=totlow+totmed+tothigh;
percentlowtot=100*totlow/totpixels;
percentmedtot=100*totmed/tot pixels;
percent high tot=100*tot high/totpixels;
med-tot;percenthightot];
output2(:,q-1)=[percentlowtot;percent
',output2);
%fprintf('%6.0f\r
%b
end
%
Display relevant
images
for i=l:number of images,
original(:,
(size
x*(i-1)+1):(size x*i))
=
GAG-map(:,:,i);
multiimagebottom(:, (sizex*(i-1)+1):(sizex*i))
areaofinterest(:,:,i,numberofvessels+l);
=
end
for i=1:number of vessels;
(size
vesselimages(:,
x*(i-1)+1):(size x*i))
=
vesselmap(:,:,i);
end
figure(7);
multidisplay(:,:)=[original;multiimage bottom];
imshow(multidisplay(:, :) ,cm, 'notruesize');
titlestring =
'Originals, Without Vessels, HLM maps:
title(titlestring);
axis('image');
colorbar;
77
';
f igure
(8)
;
imshow(vessel images(:,:),cm,'notruesize');
title('Vessels Analyzed One at a Time');
colorbar;
save surround
78
GAG contents of pixels near blood vessels
100%
80%/0+-
II
W
X
600/6
61 6
1
-0
OR
40%20%
U-/*
HIP
II
I
I
-
I
I I
Xb
0
404,
Elow GAG
C,',
40
Omed GAG
e\,
40
0
O\0
E high GAG
Example analysis of GAG contents of pixels surrounding vessels
after 3 weeks of recovery: each vessel individually, all vessels
considered together, and all pixels in the 'whole' sample
irregardless of proximity to vessels. Perivascular (pixels within a 3pixel distance to a blood vessel) regions contain less GAG than
non-perivascular regions.
79
Appendix H: Raw Data
MRI Data: average [GAG] at each imaging session
Average [GAG] measured with MATLAB, mg/ml
20 ng/ml 11-1 Series, average over entire sample including vessels
Plug ID
Weeks of
Recovery
11, (s) M2s2
19, (s) L2S2
4, (s), M1S3
2, (s) M2S5
9, (s), M3S4
12, (1) M3S2
17, (1) L3S2
14 (1), M4S3
16 (1), L4S3
1, (1) MiS5
15, (t) L4S2
3, (t), M3S5
13, (t) M4S2
10, @ M1S2
6, ( L2S3
6-day
6-day
6-day
6-day
6-day
9-day
9-day
9-day
9-day
9-day
Trypsin
Trypsin
Trypsin
Control
Control
Before
Treatment
After 1 wk 2 wks 3 wks 4 wks
16
16
25
27
24
7
19
26
33
30
18
26
40
51
51
27
40
51
56
56
22
28
47
40
63
63
6
17
26
31
77
18
21
25
26
11
27
42
46
14
21
44
52
5
14
40
44
61
3
7
19
20
30
3
5
14
11
16
60
13
6
16
15
19
50
49
47
50
51
52
49
53
47
78
72
10 ng/ml Il-1 Series, average over entire sample excluding vessels
Plug ID
3,(3d)M2S2
4(3d) L4S2
5(6d)L3S2
7 (6d)L2S3
10 MiSi
20 L2S1
Weeks of
Recovery
3-day
3-day
6-day
6-day
control
control
Before
Treatment
81
97
105
99
After 1 wk 2 wks 3 wks 4 wks
60
63
70
82
74
37
73
75
61
62
61
70
68
79
68
59
68
76
72
70
77
93
70
78
71
91
91
74
81
71
80
Appendix H
Assay Data: Daily GAG release (ug) to media
Media Change:
M1 M2
M3
M4
M6
M5
M7
M9 M1O M11 M12 M13 M14 M15 M16 M17 M18 M19 M20 M21 M22 M23 M24 M25 M26
M8
20 ng/mI Il-1
8/9 8/10 8/11 8/12 8/13 8/14 8/15 8/16 8/17 8/18 8/19 8/20 8/21 8/22 8/23 8/24 8/25 8/26 8/27 8/28 8/29 8/30 8/31
1
6
1
4
0
0
2
4
0
0
67 61 42 11
84 75 78
16
18 20 30 46 83
9/1
0
9/2
2
9/3
1
7
3
5
5
2
0
0
0
2
5
1
2
3
3
9
5
35
0
5
3
22
1
25
5
24
0
3
3
24
0
7
4
24
0
6
12
26
Plug ID
1,(l)
M1S5
TX
9-day
2,(s) M2S5
6-day
24
22
34
36
41
68
66
66
71
47
3
6
4
4
2
9
5
5
8
5
10
4
3,(t), M3S5
trypsin
21
15
18
10
6
11
7
11
4
7
9
0
0
0
0
0
0
0
1
0
3
0
4,(s), M1S3
6-day
10
14
15
37
41
75
78
64
43
12
0
5
0
15
0
3
6
2
3
4
6
5,(t) M2S3
6,@L2S3
7,(t) M1S4
8,@ M2S4
Trypsin
Control
Trypsin
Control
22
16
20
23
15
14
15
16
21
13
20
27
16
10
5
17
8
2
4
9
10
14
10
13
6
8
7
10
8
4
9
11
6
6
11
12
3
3
2
11
18
4
34
14
0
5
0
9
0
5
0
14
0
5
0
18
0
5
0
22
0
4
2
26
0
11
1
35
0
5
7
14
0
9
4
33
0
7
3
28
9,(s), M3S4
6-day
21
12
16
19
31
10, @M1S2
Control
23
13
18
11,(s)M2s2
6-day
12,(1)M3S2
9-day
21
13
16
14
18
16
13,(t)M4S2
Trypsin
23
15
14(l),M4S3
9-day
23
15,(t)L4S2
Trypsin
25
16(l),L4S3
9-day
17,(l)L3S2
18,@L3S4
64
66
84
98
44
9
5
4
1
0
3
2
4
4
5
5
4
5
3
3
3
8
17
16
19
23
15
11
13
16
10
12
10
10
11
10
10
9
6
8
5
6
9
18
47
52
68
68
2
1
2
2
16
2
0
0
6
5
1
16
5
2
5
68
3
1
2
57
5
0
6
36
9
37
3
12
21
39
7
14
85
63
3
3
4
2
2
3
3
19
5
3
11
10
10
7
7
26
6
1
0
0
1
4
1
4
5
2
2
4
2
3
2
17
20
15
24
50
65
75
96
79
83
64
3
3
7
4
5
8
3
3
5
3
3
3
15
18
10
8
12
6
5
8
11
20
6
4
0
0
1
1
3
2
5
1
3
4
2
1
3
21
15
19
26
37
52
75
80
89
66
73
69
22
1
3
3
2
4
3
6
2
4
5
4
3
5
9-day
Control
19
16
13
30
20
26
17
17
31
5
30
10
51
10
23
5
64
11
57
12
44
13
22
19
17
16
6
15
0
10
1
13
10
17
3
15
5
19
5
20
3
20
3
15
3
16
3
18
2
17
4
21
19,(s)L2S2
6-day
26
25
24
15
70
46
95
82
66
20
7
3
0
0
0
34
3
2
4
7
4
2
4
2
2
20,@ L2S3
Control
20
25
23
12
9
16
12
11
11
9
12
12
12
11
8
11
28
13
17
18
15
10
14
11
12
6
Start 11-1
10 ng/nl Experiment
Plug ID
1©M1S1
2@ L2S1
TX
4/5
Control 37
Control 38
4/6
21
18
4/7
24
35
4/8
13
13
stop trypsin
6d
stop
6 day
9 day
3
14
4/9 4/10 4/11 4/12 4/13 4/14 4/15 4/16 4/17 4/18 4/19 4/20 4/21 4/22 4/23 4/24 4/25 4/26 4/27 4/28 4/29 4/30
15
10 12 4.5
18
11 9.3 5.7
17
11
14 1.3 20 20
16
13
17
20 17
17 20 23
21
12 8.7 4.8
12 6.8
11 8.5
11
8
11
0 12
13 7.6
11
16 12
16 12
19 19
3,(3d)M2S2
3-day
35
13
13
8
11
6.8
6.8
17
98
5.4
6
3.5
0.3
2.2
3.5
0.4
3.5
6.8
3.4
4
5.7
2.9
5.3
4
8.3
10
4(3d) L4S2
5(6d)L3S2
3-day
6-day
19
32
17
15
14
50
6.9
12
14
24
8.5
13
8.2
12
14
11
95
72
6
4.9
6
7.4
6.6
1.3
6.4
5.7
5.7
3.6
9.2
8.4
0
0
9.5
8.4
12
11
10
6.4
10
10
9.6
9.8
11
11
7.4
11
11
12
12
10
14
15
7 (6d)L2S3
6-day
36
13
38
13
23
13
77
6.9
73
7
3.1
7
5.3
16
3.4
0.1
5.9
8.6
5.3
6
16
6.3
9.6
5.5
8.4
8.7
81
Appendix H
Assay Data: Daily GAG release (ug) to media
Media Change:
M29 M30
M28
M27
M32 M33
M31
20 ng/m 11-1
Plug ID
TX
9/4
9/5
9/6
9/7
9/8
9/9
9/10
1, (1) M1S5
9-day
2
2
4
1
1
2
3
2, (s) M2S5
6-day
7
5
7
5
8
6
5
3, (t), M3S5
trypsin
1
0
1
0
0
0
1
4, (s), M1S3
6-day
4
3
3
3
1
2
1
5,(t) M2S3
Trypsin
0
0
0
0
0
0
0
6, @ L2S3
Control
7
6
8
8
7
4
6
7,(t) M1S4
Trypsin
30
48
34
38
22
12
9
8,@ M2S4
Control
24
28
27
26
24
26
37
9, (s), M3S4
6-day
4
4
4
8
4
3
4
10, D M1S2
Control
6
10
7
7
6
8
9
11, (s) M2s2
6-day
3
4
6
12
8
18
7
12, (1) M3S2
9-day
3
3
2
2
1
0
2
13, (t) M4S2
Trypsin
3
3
3
3
1
2
3
14 (1), M4S3
9-day
3
3
3
4
3
3
4
15, (t) L4S2
Trypsin
3
4
3
3
2
4
4
16 (1), L4S3
9-day
3
5
4
6
3
9
5
17, (1) L3S2
9-day
4
3
2
5
2
4
3
18,@L3S4
Control
21
25
22
26
20
23
49
19, (s) L2S2
6-day
3
3
4
4
2
3
5
20,0 L2S3
Control
13
15
15
52
71
57
10 ng/mI Experiment
Plug ID
TX
5/1
5/2
5/3
5/4
5/5
5/6
5/7
5/8
5/9
1W
Control
18.7
18.2
14
15.5
19.4
17
21
21
23
2@ L2S1
Control
16.6
14.2
10
10.7
15.2
11
14
7.44
11
3,(3d)M2S2
3-day
6.7
8.58
2.5
6.84
10.7
10
10
9.23
7.6
4(3d) L4S2
3-day
13.3
11.5
4
13.2
12.3
10
11
11.2
4.9
5(6d)L3S2
6-day
13.2
10.3
5.9
12.4
20.8
13
15
11.3
14
7 (6d)L2S3
6-day
8.26
9.85
3.4
13
15.7
9.2
8.5
8.63
14
MiSi
82
Appendix I: DETERMINATION OF FCD WITH MS-325
ABSTRACT
Articular cartilage owes its compressive stiffness to its proteoglycan proteins whose high
negative charge density attracts counterions into the collagenous extracellular matrix and
produces significant Donnan osmotic swelling pressures. The tissue concentration of PG sidechain glycosaminoglycans (GAGs), has been shown to be a good indicator of cartilage
compositional integrity and health.' Negatively charged contrast agents distribute in cartilage in
inverse proportion to GAG content. Thus, cartilage GAG content can be derived from magnetic
resonance (MR) measurement of the concentration of agent in tissue. Tissue agent concentration
is found from a difference of MR spin-lattice relaxation rates of tissue with and without agent.
Tissue and bath concentrations of the agent and a modified Donnan-theory can then be applied to
calculate the cartilage fixed charge density (FCD) as a measure of GAG content.
In this study, MS-325, an MR imaging contrast agent with a -3 valence, was evaluated as a
potential alternative to the previously validated agent, Magnevist, for cartilage FCD and GAG
determinations.' The relaxivity of MS-325 in saline at 8.45 T was experimentally determined to
be 5.2 mMs'. The relaxivity of MS-325 in tissue was assumed to be the same as in saline.
Normal young bovine cartilage plugs (n=4) were equilibrated MS-325 and Magnevist solutions,
and their TI relaxation times in each agent were measured by MR spectroscopy. In another
experiment, the Ti's of trypsin-degraded samples were measured in several MS-325 solutions of
different concentrations. The FCD of each plug was calculated using the TI relaxation time in
Magnevist and a previously validated quasi-theoretical computation based on a modified
Donnan-theory in which the ideal Donnan FCD prediction is multiplied by an empirical factor of
2.1 A modified Donnan-theory was similarly developed for MS-325, a compound with a
dissociated charge of -3. In order to match the calculated FCD of 1mM MS-325 to that predicted
by Magnevist, ideal Donnan predicted FCD values for MS-325 were multiplied by an average
empirical factor of 2.4.
The results of these experiments suggest that MS-325, in concentrations of ImM or greater, and
a modified Donnan theory, can predict the FCD of normal and degraded bovine cartilage.
However, TI relaxation times of samples equilibrated in low concentrations of MS-325 (0.4
mM), showed a greater concentration of agent within the sample than in the bath which suggests
that that MS-325 distribution in cartilage is due to some sort of chemical binding in addition to
electrochemical attractions. Moreover, the process of washing MS-325 out of cartilage samples
took much longer than expected for simple diffusion of the agent into an infinite saline bath.
MS-325 was designed as an albumin-targeted contrast agent for MR angiography. 2 Thus, it is
suspected that MS-325 binds to albumin and/or other to proteins in cartilage.
83
INTRODUCTION
Articular cartilage is a strong and wear-resistant tissue in synovial joints that distributes stresses
while providing a low-friction articulating surface. The compressive stiffness of cartilage is
largely due to its proteoglycan (PG) proteins whose high negative charge densities confer a fixed
charge density (FCD) to the collagenous extracellular matrix. Mobile ions distribute in tissue to
reflect this FCD and attract water molecules into the matrix. Thus, articular cartilage stiffness
arises, in part, from Donnan osmotic swelling pressures associated with the PG and water content
of the tissue. The concentration of glycosaminoglycans (GAGs), PG side-chains, that are present
in articular cartilage has been shown to be a good indicator of cartilage FCD, compositional
integrity and health.'
Cartilage GAG content can be derived from magnetic resonance (MR) measurements of tissue in
the presence of a negatively charged contrast agent whose relaxivity (R) is known. Relaxivity is
a characteristic property of an agent that represents the agent's tendency to alter a sample's TI
relaxation time. MR measured spin-lattice relaxation rates (I/T 1 times) of tissue with and
without a contrast agent can be used with the known R to determine the concentration of agent
within the tissue. Donnan theory of electrochemical neutrality implies that negatively charged
contrast agents distribute in cartilage in concentrations inversely proportional to the local FCD.
Thus, measurement of the concentration of agent in the tissue will allow calculation of tissue
GAG.I
Accurate measurements of cartilage FCD and GAG based on this reasoning have been made with
the contrast agent Gd-DTPA 2 (Magnevist, Berlex Laboratories, Wayne, NJ). Magnevist is very
useful in MR imaging and spectroscopic studies of cartilage due to its relatively high relaxivity
(4.5 mMs'1) compared to that of tissue.' However, ideal Donnan-theory FCD predictions based
on tissue and bath concentrations of Magnevist have been shown to under-predict the actual
tissue FCD by a factor of 2.1 Therefore, an empirical scaling factor of 2 is needed to modify
Donnan-theory FCD predictions when using Magnevist. The empirical factor of 2 allows
accurate prediction of tissue FCD over a wide range of clinically relevant concentrations of
Magnevist.'
Recently, EPIX Medical has developed a new MR contrast agent, MS-325. 2 This agent, designed
for use in human blood pool imaging, has a dissociated charge of -3 and a relaxivity higher than
that of Magnevist at 0.47 Tesla. 2 The more negative valence and the higher relaxivity of MS-325
compared to Magnevist suggest that MS-325 has the potential to illuminate cartilage GAG loss
with even greater sensitivity than Magnevist. The purpose of this investigation is to evaluate
MS-325 as a potential alternative to Magnevist for cartilage FCD and [GAG] studies by MR.
84
MATERIALS AND METHODS
Contrast Agents
MS-325 (chemical name: trisodium-{(2-(R)-[4,4-diphenylcyclohexyl) phosphonooxymethyl]diethylenetriaminepentaacetato) (aquo) gadolinium (III))) was developed and supplied by EPIX
Medical (Cambridge, MA). 2 MS-325 has a molecular weight of 957 (assumed dissociated
wt.=891), a dissociated charge of -3, and a reported relaxivity of 6.6 mMs 1 at 0.47 T.2 GdDTPA (Magnevist) was obtained commercially (Berlex Laboratories, Wayne, NJ). Magnevist
has a molecular weight of 938 (dissociated wt.=548) and a dissociated charge of -2.2 Solutions
were prepared with 150mM saline (buffered to pH, 7.1) (Hanks' Balanced Salt Solution (IX);
Life Technologies, Rockville, MD).
Relaxivity
The relaxivity of MS-325 in saline at 8.45 T was measured using six solutions of MS-325 of
different, known concentrations (0, 0.2, 0.4, 0.6, 1.0 and 2.0 mM). Proton TI relaxation times
for the solutions at room temperature were measured by an inversion-recovery pulse sequence
(12 inversion delays, standard 5 mm RF probe) on a Bruker spectrometer (Bruker Instruments,
Billerica, MA). Strictly speaking, agent relaxivity and concentration are related through a
difference in the T1 relaxation rates of a sample (solution or tissue) with and without agent.
Here, the relaxation rate of solution (saline) without agent is constant so only the relaxation rate
(1/TI) of saline with agent and solution concentration are needed to determine relaxivity.
Relaxivity is inferred from the inverse of the slope of plot of MS-325 concentration verses TI
relaxation rate of solution with agent.
Cartilage TI Relaxation Time Measurements
Normal Cartilage: Young bovine cartilage plugs (3mm diameter, 2mm thick), harvested from
the femoropatellar groove (n=4), were equilibrated in saline and stored at -20'C until use.
Before each experiment, the plugs were thawed and equilibrated
for varying lengths of time (1.5 to 24 hrs) in the test solution. Proton TI relaxation times were
measured by an inversion-recovery pulse sequence (12 inversion delays, standard 5 mm RF
probe) on a Bruker spectrometer (Bruker Instruments, Billerica, MA).
Trypsin-degradedCartilage: Young bovine cartilage plugs (n=2, 3mm diameter, 2mm thick;
and n=3, 9mm diameter, 2mm thick), harvested from the femoropatellar groove, were
equilibrated in saline and stored at -20*C until use. Two small and one large plug, were placed
in 0.25mg/ml trypsin baths for 5 hours then washed twice in fetal bovine serum for 30 min/wash.
All of the plugs were then equilibrated in MS-325 for a least 24 hrs: all three large plugs were
placed in 0.4mM solutions, and the two small plugs were placed in 2.0mM and 1.0mM solutions.
TI relaxation times were measured (as above) for each plug before and after the addition of MS325.
85
FCD Determinations
First, the concentration of contrast agent in the tissue was derived from the measured TI data by
finding the difference between tissue relaxation rates with and without contrast agent and
dividing by agent relaxivity, Equation 1. (The relaxivity of Magnevist in tissue is known, R=4.5
mMsI. It was assumed that the relaxivity of MS-325 in tissue is the same as was measured in
saline.)
1 1
1
[Agent]Ti.=Eq. 1
R T
Tissue+Agent
Tissue
Next, the fixed charge density (FCD) of each plug was calculated using the known concentration
of Magnevist in the bath, the derived concentration of Magnevist in the tissue and a previously
validated quasi-theoretical computation based on a modified Donnan-theory for ions in
electrochemical equilibrium.' Note the modifying factor of 2 on the right side of Equation 2.
FCD=2x[Na+],x
GdDTpA2i,
[Gd
-DTPA-],
[Gd-DTPA 2 ib
[Gd -DTPA 2 ],
Eq.2
An ideal Donnan-theory (with no modifying factor) was similarly developed for MS-325, a
compound with a dissociated charge of -3, Equation 3.
FCD = [Na+]b
X
[MS - 3253-I
[MS - 3253- ]E.
'3
3-]
[MS - 325'- ]b
[MS - 3253-
],
Eq. 3
FCDs determined by the ideal Donnan-theory for MS-325 were scaled to match the FCDs
determined by the modified Donnan-theory for Magnevist. The average scale factor required to
make the MS-325 ideal FCD match the modified FCD of Magnevist was calculated for 1mM
MS-325 solutions.
Tissue GAG content was calculated by assuming -2 moles of charge per mole of GAG in the
tissue with GAG molecular weight, 502.5 g/mole, Equation 4.
[GAG] = FCD 5*02.5
2
10-3
Eq. 4
RESULTS
Relaxivity in Saline
A plot of TI relaxation rate vs. MS-325 concentration in 150 mM saline solution was found to be
approximately linear over the range of concentrations tested indicating that MS-325 relaxivity
was constant over this range. The relaxivity of MS-325 was inferred from the slope in figure 1 to
be 5.2 mMs'. See Appendix A for raw data.
86
Fig.
1.8
-
1.6
-
1.4
-
1
[MS-325] vs.
1/TI
0.8
R = 1/1.922
0.6
-
0.4
-
=5.20 mil Ms
0.2 00
6
4
12
10
8
1/I 1, (sec)
TI Relaxation Time Measurements and FCD Calculations
Normal Cartilage:Table 1 shows measured TI relaxation times for each plug in each test
solution. The measured TI's are listed in chronological order from left to right, and equilibration
time in each test solution is noted.
Table 1 Measured T1 Relaxation Times (sec) at 8.45 Tesla
Plug
Equilibrati
on Time
150 mM
hmM
1mM
1mM
150 mM
1mM
2mM
1mM
Hanks
MS-325
Magnevist
Magnevist
Hanks
Magnevist
MS-325
Magnevist
2 hr eq
3 hr eq
1.5 hr eq
3 hr eq
6 hr eq
24 hr eq
24 hr eq
24 hr eq
__
Small 1
Small 2
1.83
1.8
0.432
0.48
0.168
0.952
0.422
1.09
1.81
1.8
0.399
0.433
0.234
0.247
0.235
0.195
Small 3
1.89
0.491
0.416
0.432
1.86
0.399
0.325
0.124
Small 4
1.94
0.492
0.873
0.812
Small 5
1.85
0.494
0.409
0.419
1.78
0.414
0.22
0.206
Average
1.8
0.48
0.56
0.65
1.8
0.41
0.26
0.19
Determining the actual FCD of each plug was confounded by the fact that the average TI
relaxation time for the plugs in imM Magnevist varied depending on the preceding equilibrating
solution. However, Table 1 shows that the second set of T1 data in saline, measured following a
6 hr equilibration in 150 mM saline, agreed well with initial saline Tis. Furthermore, Figure 2
(below) indicates that the average FCD predicted by the Magnevist measurements immediately
following the second saline wash is within the expected range of FCDs for normal articular
cartilage. Therefore, the Magnevist TI's measured immediately following a 6-hr saline wash-out
(Table 1, column 6) were chosen as the reference measurements for subsequent FCD
calculations. The average reference T1 relaxation time for Magnevist was found to be 410
87
msec. The reference Ti's in Magnevist, a relaxivity of 4.5 mMs' and an empirical scaling factor
of 2 were used to calculate the FCD of each plug. The average calculated (and assumed
accurate) FCD for the plugs was found to be -280 mmol/L.
The average TI relaxation time for the same plugs in MS-325 also differed depending on the
preceding equilibrating solution. Thus, the MS-325 Ti's measured immediately following the
initial saline equilibration were chosen as reference for subsequent MS-325 FCD calculations
(Table 1, column 2). The average reference TI relaxation time for MS-325 time was found to be
about 470ms. Using the reference Ti's in MS-325, a relaxivity of 5.2 mMs' (where tissue
relaxivity was assumed equal to that in saline) and no empirical scaling factor, the average MS325 "FCDs" were calculated to be
-120 mmol/L. In order to achieve a match of the "FCDs"
predicted by MS-325 and those determined with Magnevist, the MS-325 "FCD" calculations
were scaled up by an average factor of 2.4.
Fig. 2 Calculated FCD
500 450
-
400
350
300
250
200
--
150 100
50 -
0
MS-325
MS-325*
Gd-"
Gd-2
Gd-2
MS-325
MS-325*
Gd-2
FCDs are presented in chronological order of measurement from left to right. Black bars represent MS-325 "FCD" with no scale factor. Striped
bars are simply scaled versions of preceding black bars. The striped MS-325* FCDs are calculated by ideal Donnan-theory and then scaled up
by an empirical factor of 2.4. Grey bars illustrate Magnevist FCD calculations using an empirical factor of 2.
Fig. 2 illustrates average FCDs calculated for each average TI listed in Table 1.
Magnevist FCDs are calculated using an empirical factor of 2. MS-325 FCDs are calculated
with no scale factor. Additional scaled MS-325* FCD's averages are shown to the right of their
unscaled counterparts (striped bars). Error bars indicate ±SD in each FCD calculation.
Table I and Figure 2 indicate that the first 2 sets and the last set of the TI measurements with
Magnevist lead to physically unlikely FCD calculations for normal articular cartilage. The
average measured T1 relaxation times of the first two sets were much shorter than TIs generally
measured in normal articular cartilage indicating a higher concentration of agent in the tissue
than in the bath. The last set of Magnevist Tis gave rise to physically impossible positive FCD
values for the cartilage plugs. Each of these measurements were made following after 1.5 hrs,
4.5 hrs (3 hrs plus the preceding 1.5 hrs), and 24 hrs equilibration in Magnevist respectively.
88
These equilibration periods served to "wash-in" Magnevist while simultaneously "washing-out"
MS-325, where the respective MS-325 concentrations were 1mM, 1mM, and 2mM.
Trypsin-DegradedCartilageExperiment: Table 2, shows the TI relaxation times for the plugs in
saline and then with the addition MS-325 and the calculated FCDs.
Table 2. Measured T1 Values and Calculated FCDs for Normal and Degraded
Cartilage
T1 in MS-325
[MS-325]
T1 in Hanks
Plug
(sec)
mmol/L
(sec)
Large 1
1.7
0.4
0.215
FCD*
Large 2
1.5
0.4
Large-Trypsin
1.8
0.4
Small Trypsin 1
1.5
2.0
0.229
FCD*
+245
0.117
FCD*
1.3
+ 139
0.161
FCD*
Small Trypsin 2
+ 155
1.0
- 68
0.163
FCD*
- 77
Note: All TI values are measured in seconds, all FCDs are given in mmol/L.
Note: MS-325 FCD* values represent FCDs calculated by Eq. 2 and then multiplied by a factor of 2.4.
The Ti relaxation times of the small degraded plugs in 1.0mM and 2.0mM solutions were very
short (0.163s and 0.117s respectively) and predicted very small FCDs for the tissue. The T1
relaxation times of the large plugs (two normal and one degraded) in 0.4mM MS-325 solutions
were extremely short (<0.25s) and lead to positive FCD values indicating a greater concentration
of MS-325 in the tissue than in solution.
DISCUSSION
Cartilage GAG concentration can be measured in vitro using magnetic resonance spectroscopy in
the presence of a negatively charged ionic contrast agent.1 Magnevist, a gadolinium based
contrast agent with a dissociated charge of -2, has been shown to accurately quantify [GAG] in
both normal and degraded tissues, and its use is becoming more common among cartilage MR
researchers. "3 In the presence of a negatively charged contrast agent, cartilage GAG content can
be visualized and quantified by proton MR with greater spatial resolution and sensitivity than by
sodium MR techniques.
MS-325, an MR contrast agent developed by EPIX Medical, has a higher relaxivity and a more
negative charge than that of Magnevist. 2 Consequently, MS-325 has the potential to provide a
more sensitive measurement of cartilage GAG concentration with greater resolution than
Magnevist. Due to its -3 charge, MS-325 is expected to permit [GAG] quantification by MR
with roughly twice the sensitivity of Magnevist at 8.45 T, (see Appendix B for theoretical
calculations).
89
Other potential advantages of MS-325 include its prolonged plasma half-life and its lack of tissue
retention. 2 MS-325 has been reported to exhibit an in vivo half-life of approximately 1 hr which
allows a long window of imaging time for in vivo studies. 2 Moreover, MS-325 strongly yet
reversibly binds to human serum albumin such that "a small amount of unbound MS-325 is
always present, ensuring efficient renal excretion." 2 Gadolinium compounds like Magnevist are
known to bind to large polymeric structures and thus remain in the liver and bones "for weeks." 2
In comparison, biodistribution studies of MS-325 in the rat have indicated no appreciable
retention of the agent in any organ.2 However, for the purposes of cartilage studies, the fact that
MS-325 binds to albumin in the blood may be an overall disadvantage because it may also bind
to proteins that exist in cartilage. If this were the case, MS-325 distribution in cartilage would
altered such that it distributed due to both protein binding and to satisfy electroneutrality
consequently confounding FCD measurements.
The results of this study suggest that bovine cartilage GAG concentration can be measured and
quantified in vitro using MR spectroscopy in the presence of sufficiently large concentrations of
MS-325. At concentrations of 1mM, MS-325 and a modified Donnan-theory (ideal Donnantheory for -3 valence scaled up by a factor of 2.4) may be used to determine cartilage FCD and
GAG content in both normal and trypsin-degraded cartilage. The accuracy of such
determinations is based on the assumption that FCDs predicted by measured TI values in
Magnevist are correct. It is noted, however, that the Magnevist data are inconsistent (Table 1),
thus the accuracy their FCDs is questionable.
At low bath concentrations of MS-325 (0.4mM), measured TI relaxation times were shorter than
expected suggesting that the concentration of agent within the tissue was greater than that of the
bath (i.e. tissue [MS-325]>0.4mM). Furthermore, the fact that washing MS-325 out of cartilage
samples took much longer than could be expected by simple diffusion, suggests that bonds more
energetic than electrochemical attractions held the MS-325 in the tissue (see Appendix A for
estimated diffusion time). Such results may be interpreted as a chemical binding of MS-325 to
the tissue in addition to the expected electrochemical diffusive distribution. Unfortunately, MS325's affinity for human serum albumin may also permit the agent to bind to proteins present in
cartilage which may, themselves, be inhomogeneously distributed in cartilage further impeding
FCD measurements.
If, indeed, MS-325 distributes in cartilage according to its charge and the availability of albumin
(or other) binding sites, then it is understandable that the total MS-325 tissue concentration
would be higher than in the bath at low bath concentrations. For cases in which the
concentration of MS-325 binding sites in tissue is close to or higher than the concentration of
MS-325 in the surrounding bath, equilibration of tissue in the agent would result in saturation of
all MS-325 binding sites in addition to its electrochemical distribution. For cases in which the
concentration of binding sites is insignificant compared to the bath concentration, then,
presumably, the concentration of bound MS-325 in tissue would be insignificant relative to the
concentration of MS-325 electrochemically distributed in the tissue. Therefore, TI relaxation
time of MS-325 in tissue only offers a meaningful measure of cartilage FCD when the MS-325's
distribution is dominated by electrochemical attractions (i.e. high bath concentrations relative to
binding site concentration).
90
CONCLUSION
MS-325 likely binds to albumin and/or other to proteins in cartilage, thus its utility as a contrast
agent in cartilage FCD determinations is limited to situations in which the concentration of the
agent in the bath is significantly higher than the concentration of MS-325 binding sites in the
tissue. In the present experiment, it was found that MS-325 in concentrations of 1mM or higher
predicted cartilage FCD and GAG content when combined with a modified Donnan-theory. The
relaxivity of MS-325 in this study was found to be 5.2 mMs-1, and the average Donnanmodifying scale factor for 1mM MS-325 was found to be 2.4. The advantages of using MS-325
instead of Magnevist in cartilage studies include greater sensitivity to GAG content and a lack of
tissue retention.
REFERENCES
[1]
Bashir, A., Gray, M.L., Harke, J., Burstein, D. Nondestructive Imaging of Human
Cartilage Glycosaminoglycan Concentration by MRI. Magnetic Resonance in Medicine.
1999; 41:857-865.
[2]
Lauffer, R.B. MS-325: Albumin-targeted Contrast Agent for MR Angiography.,
Radiology. 1998; 207:529-538.
[3]
Wagner, M., Werner, A., Grunder, W. Visualization of Collagenase-Induced Cartilage
Degradation Using NMR Microscopy. Investigative Radiology. 1999, 34; 10:607 -614.
[4]
Burstein, D. Diffusion of Small Solutes in Cartilage as Measured by Nuclear Resonance
Spectroscopy and Imaging. Journal of Orthopaedic Research. Vol. 11, no. 4, pp. 465478, July 1993.
91
APPENDIX 1: MS-325 RELAXIVITY IN SALINE
Plug #
TI (sec)
1/TI, (1/sec)
1
2
3
4
5
6
2.927
0.626
0.348
0.279
0.186
0.091
0.34
1.60
2.88
3.59
5.38
10.95
[MS-325],
(mM)
0.0
0.2
0.4
0.6
1.0
2.0
DIFFUSION OF MS-325
Estimated Time to Equilibrium:
-Plug dimensions: 3mm diam X 2mm tall
shortest distance to diffuse = / (height)=lmm
-Assume MS-325 diffusivity on the order of Magnevist diffusivity, D~10A6 cmA2/sec
The dissociated molecular weight of MS-325 is about 50% greater than that of
Magnevist (858 compared to 547) which would tend to slow its diffusion. However,
the magnitude of the valence of MS-325 is greater than that of Magnevist (1-31
compared to 1-21) which would tend to speed its "drift" due to electrochemical
attractions. For this analysis, it is assumed that these effects are of the same order of
magnitude and cancel each other out so that the effective diffusivity of MS-325 in
cartilage is on the order of that of Magnevist.
-Effective diffusivity of solute through cartilage is approximately 60% the diffusivity
through solution.4
Therefore, expected time to reach diffusive equilibrium:
T = (LA2)/[2*D*(60%)] ~ (0.1cm)A2/[2*(10A-6)cmA2/sec*(60%)] = 2.3 hrs
Thus, MS-325 is expected to take approximately 2.3 hrs to reach diffusive equilibrium in the
plug.
92
Thesis3
Ashley Williams, 01/08/01
APPENIIX 2: COMPARISON OF GAG SENSITIVITIES
[GAG]
(mmol/L)
T1 (sec) in 1mM
Magnevist
100
75
60
50
40
30
25
10
<1
0.541
0.438
0.381
0.345
0.311
0.279
0.264
0.222
0.198
% drop from
T1 without
agent
70
76
79
81
83
85
85
88
89
T1 (sec) in 1mM
MS-325
0.914
0.691
0.559
0.476
0.399
0.329
0.298
0.217
0.170
% drop from
T1 without
agent
49
62
69
74
78
82
83
88
91
Note: Assume TI of tissue without agent 1.8 sec. Assume an FCD scale factor of 2.4 for 1mM MS-325.
Note: The "% drop from TI without agent" quantifies how much the TI of the tissue will be shortened due to the
presence of the agent. For example, the TI of "healthy" tissue (i.e. [GAG] = 100 mmol/L) is expected to be
approximately 1.8 sec with no contrast agent. With the addition of 1mM Magnevist, the TI of the same sample is
expected to be only 0.541 sec which is 30% of the TI with no agent, or a 70% drop from the TI with no agent.
Theoretical T1 Sensitivty to [GAG]
1
C
0
X
a
Z
0.8
E
*0
0.6
* 1mM Magnevist
0.4
*1mM
MDS-325
0.2
0
0
20
40
60
[GAG] (mmol/L)
80
100
Theoretical Relaxation Rate Sensitivity to [GAG]
6-m
5C
0
41mM Magnevist
0 3 --
1mM MS-325
0
Z
0r
1
00
20
40
60
[GAG] (mmol/L)
80
100