Hui-Min Lee and James Cole Galloway 2012; 92:935-947. doi: 10.2522/ptj.20110196
advertisement

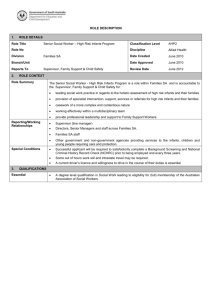
Early Intensive Postural and Movement Training Advances Head Control in Very Young Infants Hui-Min Lee and James Cole Galloway PHYS THER. 2012; 92:935-947. Originally published online March 30, 2012 doi: 10.2522/ptj.20110196 The online version of this article, along with updated information and services, can be found online at: http://ptjournal.apta.org/content/92/7/935 Online-Only Material Collections http://ptjournal.apta.org/content/suppl/2012/06/21/ptj.201 10196.DC2.html http://ptjournal.apta.org/content/suppl/2012/06/21/ptj.201 10196.DC1.html This article, along with others on similar topics, appears in the following collection(s): Motor Control and Motor Learning Motor Development Therapeutic Exercise e-Letters To submit an e-Letter on this article, click here or click on "Submit a response" in the right-hand menu under "Responses" in the online version of this article. E-mail alerts Sign up here to receive free e-mail alerts Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 Research Report Early Intensive Postural and Movement Training Advances Head Control in Very Young Infants Hui-Min Lee, James Cole Galloway Background. Daily experiences are thought to play an important role in motor development during infancy. There are limited studies on the effect of postural and movement experiences on head control. Objective. The purpose of this study was to quantify the effects of postural and movement experiences on head control through a comprehensive set of measurements beginning when infants were 1 month old. Design. This was a prospective, longitudinal, 2-cohort study. Methods. Twenty-two full-term infants who were healthy were randomly assigned to either a training group or a control group. Infants were observed every other week from 1 to 4 months of age. Head control was assessed using a standardized developmental assessment tool, the Test of Infant Motor Performance (TIMP), as well as behavioral coding and kinematics of infants’ head postures and movements in a supported sitting position. Caregivers performed at least 20 minutes of daily postural and movement activities (training group), or social interaction (control group) for 4 weeks. Results. The training group had higher TIMP scores on head control–related items during the training period and after training stopped compared with the control group. Starting from the during training phase, the training group infants had their heads in a vertical and midline position longer compared with the control group infants. After training stopped, the training group infants actively moved their heads forward more often and for larger distances. H-M. Lee, PT, PhD, was a graduate student in the Department of Physical Therapy, University of Delaware, Newark, Delaware, at the time this study was conducted. Address all correspondence to Dr Lee at: noralee0724@ yahoo.com. J.C. Galloway, PT, PhD, Infant Motor Behavior Laboratory, and Biomechanics and Movement Sciences Graduate Program, Departments of Physical Therapy and Psychology, Center for Biomedical Engineering Research, University of Delaware. [Lee H-M, Galloway JC. Early intensive postural and movement training advances head control in very young infants. Phys Ther. 2012;92:935–947.] © 2012 American Physical Therapy Association Published Ahead of Print: March 30, 2012 Accepted: March 23, 2012 Submitted: June 13, 2011 Limitations. The experiences outside daily training were not monitored, and the results may be specific to the experimental setup for infants with typical development. Conclusions. Young infants are able to take advantage of postural and movement experiences to rapidly advance their head control as early as 4 to 6 weeks of postnatal life. Infant positioning, caregiver handling, and caregiver-infant interactions were likely contributing factors. This database of comprehensive measures may be useful in future trials focused on head control in infants with special needs. Post a Rapid Response to this article at: ptjournal.apta.org July 2012 Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 Physical Therapy f 935 Early Intensive Postural and Movement Training in Very Young Infants T he development of head control begins during the prenatal period. Head movement is one of the first fetal movements observed as early as 7 to 8 weeks of postmenstrual age, with increasing movement varieties seen by the 11th week.1 Infants display dramatic changes in their head control during the first months of their postnatal life. Not surprisingly, head control is critical for a range of early behaviors, including those involving vision, oromotor skills, and the trunk and arms. For example, a dynamically stable head may provide less mechanical perturbation to the trunk and arms and may support the function of vision.2 Less perturbation and improved use of vision, in turn, may allow for better body control, which, in turn, assists infants in learning more complex behaviors. Conventional wisdom, based on studies that typically involve infants raised in Western cultures, holds that a newborn’s neck muscles are rela- tively weak and poorly controlled. Thus, newborns often are provided external support when they are held. By 3 months old of age, infants typically maintain their heads in an upright, midline position when held upright. Clinically, this upright, midline position has been considered an important basic level of head control,3,4 which continues to increase throughout the first year and beyond.5–9 The above description of the “natural” timing of the emergence of head control should not be taken as universal and immutable. Cross-cultural studies on the handling of young infants by non-Western cultures suggest that the above descriptions strongly reflect culture norms. One implication of these studies is that early head control is influenced by the degree to which infants are provided with postural and movement opportunities (reviewed in Adolph et al10). As outlined below, systemic investigations of the effect of early The Bottom Line What do we already know about this topic? For infants with typical development, movement experiences play an important role in motor development. For example, infants provided with additional advanced postural or movement experiences reach earlier than infants provided with additional social experiences. experiences on head control, however, are rare. The general purpose of the current study was to address the need for a longitudinal investigation of the effect of postural and movement experiences on head control during early infancy. Head control is the first major motor milestone on most assessments of early skills.11–14 Head control impairments often are cited as an early risk factor for future developmental delays.15 For example, head control on the Test of Infant Motor Performance (TIMP) in the first months of life is a factor in predicting which children will be diagnosed with cerebral palsy by 2 years of age.16 In several studies, infants born prematurely or developing cerebral palsy at a later age displayed poorer head control compared with infants with typical development.17–22 Delayed head control greatly influences many aspects of a child’s life.23–25 Despite the importance of head control in early intervention,4 comprehensive studies are limited and are typically cross-sectional investigations of infants at term age.17–22,26 The assessment of head control usually was conducted as a part of larger, more general neuromotor or neurobehavioral evaluation.11,13,14 Therefore, results often were composed of general posture control or What new information does this study offer? This study provides the first longitudinal quantification of the effect of postural and movement experiences on the development of head control. Very young infants with typical development who were provided with additional experiences rapidly displayed advanced head control. If you’re a caregiver, what might these findings mean for you? The daily experiences that families provide to their infants during play or therapy may influence the emergence of even the earliest skills such as head control. Daily play involving a range of positions and movements may influence the motor development of infants with special needs. 936 f Physical Therapy Available With This Article at ptjournal.apta.org • eAppendix: Training Activities for the Training Group (20 Minutes Total per Day) • eTable: Summary of the Effects of Postural and Movement Training on Head Control • Demonstration Video of Infants in the Control Group and the Training Group During Chair Play Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 July 2012 Early Intensive Postural and Movement Training in Very Young Infants posture response scores, with few specifics on head control. Furthermore, results on specific head control impairments were not always consistent, such as in the case of impairments in pull-to-sit and sitting tasks.17–22,26 The above review points out that most studies on very young infants determined the presence or absence of milestones, which do not provide information on the process by which these infants develop impaired head control or what factors lead to impaired head control. Without a detailed understanding of these factors, there is little evidence from which to build early interventions. This is the current situation with respect to treating infants with head control impairments. The current study addressed the need for a more comprehensive and longitudinal investigation on the development of head control from 1 to 4 months of age with multilevel measures. As a first step, this study focused on building a normative database using infants with typical development. If very young infants were receptive to additional postural and movement experiences, this receptiveness would provide support for the study of the effects of these experiences as “training” for infants with poor head control. In general, daily experience is critical for the emergence of basic motor skills in early childhood.7,27,28 Studies of infants who were developing typically have shown the effects of postural and movement experiences on a range of behaviors, including stepping, kicking, reaching, sitting, crawling, and postural muscle responses.27,29 –37 These studies demonstrated positive effects of training after as well as before a behavior initially emerged. Training after a behavior is displayed can advance the quality of the practiced behavior.33,35,36 Although less July 2012 studied, training before the onset of a behavior can advance the emergence and the quality of the practiced behavior.27,31,32,37 For example, infants had earlier onset of crawling after receiving 3 weeks of training.31 Six-week-old infants who received 7 weeks of sitting training displayed longer upright sitting duration immediately posttraining.37 We know of no empirical investigation of the training effects on head control in typical development. In pediatric intervention, postural and movement training are generally well-accepted strategies for promoting behaviors for young infants.38,39 Few studies, however, have focused on the effect of specific training for head control in young infants, and none were comprehensive and longitudinal. As mentioned previously, cross-culture research on motor development supports the use of physical activities and active handling as a potentially effective intervention for head control impairments.40 – 44 These studies suggest that child-rearing practices through daily formal training (eg, training to sit or walk) or informal handling (eg, how infants are carried) affect the onset ages of many motor milestones, including the development of head control. The specific purpose of the current study, therefore, was to test the hypothesis that daily postural and movement experiences would significantly influence the development of early head control. Results from this study of infants with typical development could be useful for future intervention studies of infants at risk for long-term impairments in head control. Method Participants Twenty-four full-term infants with no known sensory or motor impairments were recruited after their parents signed informed parental consent forms approved by the University of Delaware Human Subjects Review Board. Due to scheduling conflicts, 2 infants did not continue the study. Twenty-two infants were randomly assigned to either a training group (n⫽11, 6 male and 5 female) or a control group (n⫽11, 8 male and 3 female). Two infants were Asian, 2 were African American, and the remaining infants were Caucasian. Procedures Infants were seen for testing every other week for 3 months, from 1 to 4 months of age. There was no significant difference in averaged age at each testing session between groups (P⫽.67–.95). There were a total of 9 testing sessions, including 2 home testing sessions and 7 laboratory testing sessions (see Table for the summary of procedures). Home Testing Sessions One experimenter visited infants at their home when they were 1 and 1.5 months old. During the home sessions, a standardized developmental test (ie, TIMP) was conducted. When infants were 2 to 4 months old, the TIMP was conducted in the laboratory (see “Laboratory Testing Sessions” section for details), and there were no more home testing sessions. The TIMP is a sensitive, predictive, and valid tool for detecting the changes and differences in motor performance in young infants.45,46 In previous studies, the TIMP discriminated among infants with different degrees of risk for poor motor impairments at the time of initial testing,46 – 48 as well as predicted future motor impairments.16,49 –53 The TIMP scores also were sensitive to detect changes in development in infants with typical development over a 2-week period.48 In our study, we used specific TIMP items related to head control to quantify the development of head control in full-term Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 Physical Therapy f 937 Early Intensive Postural and Movement Training in Very Young Infants Table. Summary of Study Proceduresa Variable Results Age of infants (mo) 1 Average age in each group (wk) Study week 2 CG: 4.57 TG: 4.48 1 1 CG: 8.78 TG: 8.69 3 3 5 2.5 ... CG: 10.71 TG: 10.70 7 4 CG: 16.73 TG: 16.69 ... 13 Visit number Home 1 Laboratory 1 Home 2 Laboratory 2 Laboratory 3 Laboratory 4 ... Laboratory 7 Location Home Laboratory Home Laboratory Laboratory Laboratory ... Laboratory Weeks of training 0 (pretraining) 0 (pretraining) (training was introduced right after this visit) 2 2 4 Posttraining K B K B K B ... K B TIMP TIMP ... TIMP Measures Chair play Developmental test a 1.5 CG: 4.47 TG: 4.46 K B TIMP TIMP Posttraining CG⫽control group, TG⫽training group, K⫽kinematics, B⫽behavioral coding of head postures and movements, TIMP⫽Test of Infant Motor Performance. infants who were healthy (see the “Behavioral Coding” section for details). Most of these items have been shown to be key characteristics for identifying differences between children with and without cerebral palsy.16 During the second home testing session, caregivers were asked to demonstrate training activities introduced at the end of the first laboratory testing session. The experimenter checked for proper training and answered trainingrelated questions. Laboratory Testing Sessions Caregivers brought their infants to the Infant Motor Behavior Laboratory, Department of Physical Therapy, University of Delaware, every 2 weeks while the infants were 1 to 4 months of age. There were 2 com- ponents: chair play and the TIMP. When infants were 1 and 1.5 months old, only the chair play was performed in the laboratory. Starting from the session at 2 months of age, the TIMP was added to laboratory procedures. Chair play. Motion capture procedures (see “Kinematic Data Acquisition” section for details) were conducted during the chair play. Infants were seated in a customized infant chair reclined 30 degrees (Fig. 1) with their trunk secured with a wide cloth band. Two synchronized video cameras recorded right front and bird’s-eye views of the infants for behavioral coding. Three experimental conditions were conducted: no-toy arm-free (NTAF), no-toy armheld (NTAH), and toy (TOY). The NTAF and TOY conditions were used to test for differences in head control with and without a midline toy present. The NTAF and NTAH conditions were used to test for differences in head control during free and restricted arm movements. Experimental conditions were randomly ordered across infants and sessions. Figure 1. The setting of chair play. The picture shows the TOY condition. 938 f Physical Therapy Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 July 2012 Early Intensive Postural and Movement Training in Very Young Infants There were six 15-second trials for each condition. For each trial, the experimenter held the infant’s head in a neutral (midline and upright) position before the start of a trial and then gently released the head right after a trial start. The starting position of infants’ arms was not restricted for the NTAF and TOY conditions. TIMP. The TIMP was conducted and videotaped to quantify the general motor development with specific focus on the development of head control. Kinematic Data Acquisition A 6-camera (120-Hz) Vicon motion capture system (Pulnix TM6701-120 Progressive, Vicon Motion Systems Inc, Los Angeles, California) was used to obtain 3-dimensional (3D) position-time data of the infants’ head movements. The cameras were arranged in a circular fashion, with 2 cameras on each side and 2 in the front and in the back of the infant. Infants were seated within a calibrated volume of 160 cm ⫻ 160 cm ⫻ 200 cm. The average range of calibration residuals was no larger than 0.35 mm for the given calibrated volume. Arrays of three 8-mmdiameter, retroreflective, nonlinear markers were placed on the center of the forehead. Two single markers were placed on the toy in line. The array positions were kept the same between a static trial that defined the reference position of the arrays and the movement trials. The static trial data were collected with the head and trunk maintained in a neutral (upright and midline) position. Training Group Infants in the training group received postural and movement activities provided by their caregivers for 20 minutes daily for 4 weeks starting when they were 1 month of age. The specific training activities were selected based on our previous July 2012 studies27,32,54 using various types of training for young infants, including both postural training, requiring increased use of neck, shoulder girdle, and trunk muscles, and movement training, requiring increased use of arm movements for reaching (see eAppendix, available at ptjournal.apta.org, for detailed information on training activities). In our previous studies, infants received the 2 types of training separately, either postural or movement training, and began at an older age (8 weeks of age or older). To provide infants with additional upright experience, caregivers were instructed to carry their infant for an additional 20 minutes daily with a front carrier (BabyBjörn, Bredaryd, Sweden) provided to families of the training group infants. Control Group To control for the increased social interaction that infants in the training group experienced during training, infants in the control group received structured, face-to-face communication with their caregivers for 20 minutes daily for 4 weeks. Caregivers were asked to place their infants in a supine position and interact with their infants visually and verbally without physically contacting their infant or presenting toys. Daily activity journals were provided to caregivers in both groups to track the amount of activities performed each day. The percentage of training completed for the daily 20-minute activities was similar between groups (training group: X⫽103.2 %, SD⫽43.1%; control group: X⫽102.1%, SD⫽10.3%; z⫽⫺0.413, P⫽.68). On average, the use of the front carrier was completed for more than 85% of the required time in the training group. Data Analysis Kinematics. Standard kinematic analysis was conducted for head movements during chair play. A stan- dard low-pass, recursive filter (Butterworth filter) with a cutoff frequency of 4 Hz reduced highfrequency noise. The position of the head in 3D space was computed by the singular value decomposition method.55 A loss of no more than 10 frames consecutively was interpolated using cubic spline interpolation. A customized MATLAB program (The Mathworks Inc, Natick, Massachusetts) was used to calculate the head kinematics. Variables of head kinematics were analyzed based on the data concatenated across trials in each condition. The kinematic dependent variables were: (1) maximum lateral displacement (in millimeters), defined as the maximum displacement from the midline along the x axis; (2) maximum anterior-posterior displacement (in millimeters), defined as the maximum displacement along the y axis; (3) speed of head movement (in millimeters per second), defined as the average 3D speed of head movement; and (4) variability of head 3D speed, defined as the coefficient of variation of head 3D speed. Behavioral coding. Videotapes were coded for head postures and movements during chair play and the TIMP. The following behavioral coding dependent variables for head control behaviors were chosen based on observations from a pilot study showing that infants frequently display these behaviors when seated in the infant chair: (1) percentage of time in lean, defined as amount of time infants laterally tilt their heads from the midline more than 15 degrees; (2) percentage of time upright, defined as amount of time infants keep their heads in an upright, midline position and faced forward; (3) percentage of time in turn, defined as amount of time infants turn their heads to the right or left over 15 degrees from the mid- Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 Physical Therapy f 939 Early Intensive Postural and Movement Training in Very Young Infants Total Scores of the TIMP Group CG 150 * TG * * 125 Raw Score line with their head in an upright, midline position; (4) percentage of time in pop-up, defined as amount of time infants move their head forward and away from the back of the infant chair with their head in an upright, midline position; and (5) percentage of time with other postures and movements, defined as amount of time infants show head postures and movements other than lean, upright, turn, or pop-up. Each variable was coded frame by frame (1 frame⫽1/ 120 second) and normalized with respect to time for group comparisons. 100 75 50 The total score of the TIMP was the summed score of all of the 42 items of the TIMP. The summed score of the head control–related items was separated out from the total score to quantify head control from 1 to 4 months of age. Selected head control items reflected the infants’ ability to hold their head in midline or an upright position without additional visual or auditory stimulation in different body orientations (ie, supine, prone, and sitting). The following 10 items were selected: item 1 (head in midline in supine); items 15, 16, 17, and 18 (head control: supported sitting, posterior neck muscle, anterior neck muscle, lower from sitting); item 21 (head in midline without visual simulation [supine]); item 32 (pull to sit); item 36 (head lift in prone position); and items 41 and 42 (lateral head turning to the right and left). Reliability of behavioral coding. The primary experimenter (H-M.L.) was not blinded to group assignment. To promote coding score reliability, 2 blinded coders were first trained to code with interrater reliability of greater than 90% for variables measuring head postures and movements using 2 randomly selected infants in each group. Two random sessions were selected for testing the reliability of head pos940 f Physical Therapy Baseline After Training After Training Phase 1 Phase 2 During Training Phase Figure 2. The box plots for the total scores of the Test of Infant Motor Performance (TIMP) between the control group (CG) and the training group (TG) in each phase. The median for each group is represented by the single line in the box. The boxes represent the distribution of data from the 2 middle quartiles. The error bars represent the maximum and minimum values and the top and bottom quartiles of data distribution. Asterisk signifies a group difference (P⬍.05) based on the Mann-Whitney U test. tures and movements coding. Following training, each coder was assigned half of the infants to code for head postures and movements. The infants each coder received were randomly selected from the 2 groups. Head control–related items in the TIMP were scored by a third coder for all infants. The interrater reliability of TIMP items then was tested with the scoring of 2 randomly selected infants coded by a fourth coder. The reliability ([amount of agreement/(amount of agreement ⫹ amount of disagreement)] ⫻ 100) for the coding of head postures and movements was greater than 90%: upright (⬎90%), lean (⬎91%), turn (⬎91%), and pop-up (⬎95%). Interrater reliability, calculated as intraclass correlation coefficient between 2 coders for the head control–related items in the TIMP, was .943. Statistical Analysis The focus of the current study was to determine the training effects on the development of head control by testing for differences between infants in the training and control groups. Preliminary analysis did not show consistent patterns of significant differences among the 3 experimental conditions across the 7 experimental sessions. That is, certain conditions were significantly different for certain ages, but there was no clear pattern of results across conditions and sessions. Thus, these 3 conditions were combined for the final analysis. The 7 experimental sessions were combined into 3 phases for the final analysis based on when sessions occurred relative to the training period: the baseline phase (1-month-old session), the during training phase (1.5- and 2-month-old sessions when the training was being performed), Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 July 2012 Early Intensive Postural and Movement Training in Very Young Infants As the data did not follow a normal distribution and the nonkinematic data were rank orders or proportions, a nonparametric analysis (Mann-Whitney U test) was used to analyze all of the variables for group differences in each phase. The MannWhitney U test was conducted using SPSS software (SPSS Inc, Chicago, Illinois) with Pⱕ.05. The effect size (r) was calculated using the equation: Z/(N)1/2, in which Z is the z score and N is the total number of participants.56 Results Total Scores of the TIMP Results of total scores of the TIMP showed that the training group had higher scores in the during training phase (z⫽⫺3.309, P⫽.001, r⫽⫺.71) and the after training phases (phase 1: z⫽⫺3.514, P⫽.000, r⫽⫺.75; phase 2: z⫽⫺1.977, P⫽.048, r⫽⫺.42) compared with the control group (Fig. 2). TIMP Scores of Head Control– Related Items Results of the TIMP scores of head control–related items showed that the training group had higher scores during the training period and after training stopped compared with the control group. Figure 3 shows that training group infants had higher scores on head control–related items in the TIMP compared with control July 2012 TIMP Scores of Head Control–Related Items Group 50 CG TG * * 40 Raw Score and the after training phase. The after training phase was split into 2 phases—after training phase 1 (2.5and 3-month-old sessions), and after training phase 2 (3.5- and 4-monthold sessions)—to match the length of the during training phase. We combined data from 2 sessions into phases to decrease the number of comparisons and ease interpretation in this initial study of head control. Data from each of the 2 sessions per phase were averaged. Future studies may build on our results to use noncombined data. * 30 20 10 Baseline During Training After Training After Training Phase 1 Phase 2 Phase Figure 3. The box plots for the summed scores of head control–related items in the Test of Infant Motor Performance (TIMP) in each phase between the control group (CG) and the training group (TG). Asterisk signifies a group difference (P⬍.05) based on the MannWhitney U test. group infants in all phases (during training phase: z⫽⫺3.715, P⫽.000, r⫽⫺.79; after training phase 1: z⫽⫺3.909, P⫽.000, r⫽⫺.83; after training phase 2: z⫽⫺3.367, P⫽.001, r⫽⫺.72), except for the 1-month-old baseline session. In the during training phase (age 1.5–2 months), the training group infants had significantly higher scores on all 10 individual head control–related items except item 1 (z⫽⫺3.447 to ⫺2.009, P⫽.001 to .045, r⫽⫺.73 to ⫺.42) compared with control group infants. In after training phase 1 (age 2.5–3 months), the training group had significantly higher scores in 6 of the 10 items (items 15–18, 32, and 42: z⫽⫺3.811 to ⫺2.591, P⫽.000 to .010, r⫽⫺0.81 to ⫺.55). In after training phase 2 (age 3.5– 4 months), the training group had significantly higher scores in 5 of the 10 items (items 15, 18, 32, 36, and 41: z⫽⫺3.330 to ⫺2.186, P⫽.001 to .029, r⫽⫺.71 to ⫺.47). Behavior Coding of Head Postures and Movements Results of behavior coding of head postures and movements showed that starting from the training phase, training group infants had their heads in a vertical and midline position longer compared with control group infants. Training group infants continued to display advanced head control in the phases after training stopped. The percentage of the types of head postures and movements infants displayed when they were seated in the infant chair is shown in Figure 4A–D. In the baseline phase (age 1 month, Fig. 4A), 3 main behaviors characterized both training and control group infants’ head postures and movements in our infant chair: lean, Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 Physical Therapy f 941 Early Intensive Postural and Movement Training in Very Young Infants A Percentage of Types of Head Postures and Movements B Percentage of Types of Head Postures and Movements in the During Training Phase 100 100 90 90 80 80 70 70 Percentage Percentage in the Baseline Phase 60 50 40 30 50 30 20 10 Group 0 TG C Percentage of Types of Head Postures and Movements * 40 10 CG CG Group TG D Percentage of Types of Head Postures and Movements After Training Phase 1 After Training Phase 2 100 100 * 90 90 80 80 70 70 Percentage Percentage Lean Upright Pop-up Turn Others 60 20 0 * 60 50 40 30 20 60 50 40 30 * 20 * 10 10 0 CG Group TG 0 * CG Group TG Figure 4. The percentage of types of head postures and movements between the control group (CG) and the training group (TG) in the baseline phase (A), the during training phase (B), and after training phases 1 (C) and 2 (D) when infants were seated in an infant chair. Asterisk signifies a group difference (P⬍.05) based on the Mann-Whitney U test. upright, and turn. Infants in both groups spent most of the time (approximately 50%) leaning their head in various directions. The percentage of time infants kept their heads in upright and turn was the second and third highest, respectively. There was no significant group difference in any of the coded head postures and movements during the baseline phase. In the during training phase (age 1.5–2 months, Fig. 4B), infants in both groups spent the majority of the time keeping their heads in upright, lean, and turn, in the order of the highest to lowest percentages, respectively. The training group infants demonstrated less lean (z⫽⫺3.016, P⫽.03, r⫽⫺.64) and more upright (z⫽⫺2.043, P⫽.041, 942 f Physical Therapy r⫽⫺.44) behaviors compared with the control group infants. There were no significant differences between groups for turn and pop-up behaviors during the training phase. In after training phase 1 (age 2.5–3 months, Fig. 4C), infants in both groups spent the majority of the time with their heads upright, but the order of the percentage of time in the other head postures and movements varied between groups. The training group infants demonstrated less lean (z⫽⫺2.017, P⫽.044, r⫽⫺.43) and more pop-up (z⫽⫺ 2.753, P⫽ .006, r⫽⫺.59) of their heads in the chair compared with the control group infants. There was no significant difference in upright and turn behaviors between groups during after training phase 1. In after training phase 2 (age 3.5– 4 months, Fig. 4D), infants in both groups demonstrated upright, popup, and turn as the main behaviors characterizing their head postures and movements in an infant chair. The training group infants had more pop-up (z⫽⫺3.354, P⫽.001, r⫽⫺.72) and less turn (z⫽⫺3.243, P⫽.001, r⫽⫺.69) of their heads in the chair compared with the control group infants. (See a demonstration video of infants in the control group and the training group during chair play, available at ptjournal.apta.org.) There was no significant difference in lean and upright behaviors between groups during after training phase 2. Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 July 2012 Early Intensive Postural and Movement Training in Very Young Infants B Maximum Head Displacement Along A Maximum Head Displacement Along the y Axis the x Axis Group 250 300 CG TG * Displacement (mm) Displacement (mm) 200 150 100 * * After Training Phase 1 After Training Phase 2 250 200 150 50 100 Baseline 0 Baseline During Training After Training Phase 1 After Training Phase 2 During Training Phase Phase C Average Speed of Head Movements 100 * Speed (mm/s) 80 * 60 40 20 0 Baseline During Training After Training Phase 1 After Training Phase 2 Phase Figure 5. The box plots for head kinematics between the control group (CG) and the training (TG) in each phase: the maximum head displacement along the x axis (A), the maximum head displacement along the y axis (B), and the average speed of head movements (C). Asterisk signifies a group difference (P⬍.05) based on the Mann-Whitney U test. Head Kinematics Results showed measurable quantitative differences in head control ability between the training and control groups, especially during the phases after the training stopped. Head kinematics with significant differences between groups are shown in Figure 5A–C. July 2012 In the baseline phase (age 1 month), the training group infants had smaller maximum head displacement along the x axis (z⫽⫺2.084, P⫽.037, r⫽⫺.44, Fig. 5A) and slower average speed of head movements (z⫽⫺2.097, P⫽.036, r⫽⫺.45, Fig. 5C) compared with the control group infants. In the during training phase (age 1.5–2 months), there was no significant difference in any of the measured head kinematics between groups. In after training phase 1 (age 2.5–3 months), the training group infants had larger maximum head displacement along the y axis (z⫽⫺2.121, P⫽.034, r⫽⫺.45, Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 Physical Therapy f 943 Early Intensive Postural and Movement Training in Very Young Infants Fig. 5B) compared with the control group infants. In after training phase 2 (age 3.5– 4 months), the training group infants had larger maximum head displacement along the y axis (z⫽⫺2.626, P⫽.009, r⫽⫺.56, Fig. 5B) and faster average speed of head movements (z⫽⫺3.668, P⫽.000, r⫽⫺.78, Fig. 5C) compared with the control group infants. There was no significant difference between groups in the coefficient of variation of head movement speed in all phases. Discussion trol. Two major findings from the during training phase are: (1) the speed with which training experiences led to advances in head control and (2) the rapid changes across multiple measures. First, changes in head control began within weeks of providing infants with additional postural and movement experiences. Our data showed that within the first 2 weeks of daily training, the training group infants displayed significant differences from the control group infants. Specifically, the training group infants had higher scores for all head control–related items except item 1, which is an easy item on which most infants in both groups achieved the highest score during the baseline phase.48 Second, training effects were not only rapid but also were seen across multiple measures. Specifically, training altered both the quality and the quantity of infants’ performance on the TIMP, as well as how they used their head during seated play (Fig. 4C and D). Taken together, the training group infants scored higher on head control items in prone, supine, and sitting positions and during activities that required active participation. Training Advances Head Control in Infants Developing Typically Results from the multiple measures suggest that enhanced postural and movement experiences (ie, training) advanced the development of head control. The training group infants showed more advanced head control compared with the control group infants during the 4-week training period, as well as months after training. Moreover, advances displayed by training group infants showed an interesting additive pattern with advanced behavioral measures in the during training phase, then advanced behavioral and spatial kinematics (ie, maximum displacement) in after training phase 1, followed by advances in behavioral, spatial, and temporal kinematics (eg, average speed) in after training phase 2. Findings from total TIMP scores indicated that the training group infants were more advanced in their general motor development compared with the control group infants. A summary of the results of training effects on head control is provided in the eTable (available at ptjournal.apta.org). The results of each phase are further discussed in the following sections. These changes, combined with the cross-cultural research on caregiver handling,10,40 – 44 strongly suggest that a young infant’s head and neck are neither as muscularly weak nor as poorly controlled as traditionally thought. Moreover, young infants are able to take advantage of postural and movement experiences to advance their head control as early as 4 to 6 weeks of postnatal life, if not much earlier. The clinical implications will be discussed in a later section. Training Effects in the During Training Phase Training had an immediate and significant effect on infants’ head con- Training Effects in After Training Phases 1 and 2 In the weeks and months after training stopped, the training group 944 f Physical Therapy infants continued to show greater head control and more advanced head behaviors. Interestingly, these training effects differed from those noted during the training period. The after training phase results suggest that training has a lasting, positive effect on the development of head control. First, the training group infants not only achieved a basic level of head control but also were able to perform basic behaviors for longer durations or with larger degrees of movement than the control group infants. For example, in after training phase 2, the training group infants had higher scores in 5 of the 10 head control–related items. These particular items are of interest, as a Rasch analysis suggested they were more difficult items to perform.48 Second, the training group infants continued the advanced head control from the during training phase and displayed advanced movement strategies while engaging in activities in the infant chair in the weeks and months after training stopped. For example, in after training phase 1, for the first time, the training group infants moved their heads off the back of the chair (eg, pop-up) longer than the control group infants (Fig. 4C). Interestingly, in after training phase 2, although the training group infants had more time in pop-up behavior, the control group infants continued to spend more time in turn behavior (Fig. 4D). Pop-up behavior may be an especially interesting measure to follow in future studies, given that it clearly shows purposeful intent and requires significant effort. It is important to note, however, that pop-up behavior may require supported sitting in a reclined seat. Lastly, kinematic and behavioral results during the after training phases suggest that the training group infants continued to gain strength and advanced control compared with the control group infants Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 July 2012 Early Intensive Postural and Movement Training in Very Young Infants in the months after training. For instance, the training group infants not only held their heads off the back of the chair for longer durations but also moved with greater excursions (Fig. 5B) and moved their heads faster than the control group infants (Fig. 5C). During the baseline phase, when infants’ head control was generally poor, the faster speed of head movements likely resulted from insufficient control to counteract gravity or a lack of motivation to maintain an upright position. In after training phase 2, head control in both groups was beyond the basic level such that the training group infants were likely purposefully producing faster movement speeds through greater muscle activation levels, for example.57 How Early Postural and Movement Experiences Advanced Head Control Results from the current study provide empirical evidence that the emergence of head control can be advanced through early intensive postural and movement training. In addition, these results join those of other studies to strongly suggest that postnatal experience is an important factor in typical development of head control.30,35 To better understand how our training had rapid and significant effects during the training period and continued effects months after training, 3 training components—positioning, handling, and infant-caregiver interaction—are discussed next. Infant positioning. In the during training phase, the training group infants received positioning experiences that were advanced for infants during the first months of their life. Typically, in Western cultures, young infants spend much of their waking hours in a supine position.58,59 More than 30% of 4-montholds never experienced a prone position while awake, and 75% spent less July 2012 than 20 minutes daily in a prone position.60 Based on the training activities in the current study, the training group infants spent an additional 6 minutes in a prone position and 12 minutes in an upright position, which are body positions typical of older, more mobile infants. Prone and upright positions would be expected to increase the muscle performance and coordination of an infant’s neck, shoulders, and upper trunk; provide a new view of the environment; and provide novel vestibular stimulation, all of which have been associated with increased alertness and motor development.61– 68 Caregiver handling. In addition to the positions that infants were placed in for play activities, the activities themselves altered the typical manner in which caregivers handled their infants. As stated previously, in Western cultures, caregivers tend to hold young infants carefully, supporting their heads for at least the first months of their life (reviewed in Adolph et al10). In the current study, caregivers of the training group infants were instructed to perform activities that facilitated head control and were encouraged to handle their infants daily with less passive support of the head and in a much more active manner overall. The gains in head control in the current study fit with the cross-cultural research showing active handling advances head control. Infant-caregiver interaction. Lastly, the training may have influenced infant-caregiver interaction beyond physical handling. During daily training time, caregivers of the training group infants likely encouraged their infants to actively control their head appropriately. As infants developed better head control ability, their caregivers likely continued to offer additional opportunities to facilitate advanced head control even outside of the prescribed “train- ing time.” Future studies can now build on these foundation data to develop valid and reliable methods to track the type and duration of infant-caregiver interaction both during and after the daily training period. Clinical Implications One major principle of early intervention is to provide activities to advance behaviors in infants and children at risk for a developmental delay before the delay is directly observed. Several recent reviews, including a meta-analysis, however, have not found strong effects of traditional early intervention strategies on motor development during infancy, preschool age, or school age.69 Authors highlighted the need for comprehensive, sensitive measures to quantify both the short-term training period and longer-term follow-up period for intervention programs for functional abilities.38,70 As discussed above, we know of no longitudinal study with sensitive measurements on the effectiveness of interventions focused on head control. The dependent variables and training program from the current study were specifically chosen to provide a framework for future trials with pediatric populations at risk for lifelong motor impairments. The head control measures in the current study are appropriate for longitudinally tracking the development and effectiveness of intervention for head control ability during early infancy. These measures are multilevel, which provides a comprehensive view of infants’ performance of head control, and can be conducted on infants as young as 1 month old. Results from the current study suggest these measures successfully detected the training effects on head control from general behavioral changes to specific kinematic differences. Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 Physical Therapy f 945 Early Intensive Postural and Movement Training in Very Young Infants Limitations Given that this is the first comprehensive, longitudinal study of the training effect on the emergence of head control, there are several limitations that need to be considered when generalizing these results and planning for future studies. First, the experiences outside the daily training sessions were not monitored. Caregivers likely altered the infants’ daily experiences outside of the formal training time, which would be expected to influence head control. Such procedural validity will be important in future studies interested in actual intervention dosage. Second, only head behaviors were assessed. The development of head control involves not only the head, but also the limbs and trunk, as well as sensory-perceptual and cognitive development. It will be necessary to investigate the range of related systems to fully understand the development of head control. Third, data were analyzed and reported as group effects. Individual infants likely responded to the training differently. Identifying subgroups and individual patterns would assist the detection of infants with head control impairments who often form subgroups based on the distribution and degree of motor involvement. Fourth, our primary analysis focused on between-group studies. Secondary analysis of withingroup comparisons is equally important. Fifth, the results are specific to the experimental setup. Typical head control emerges within multiple, dynamic environments. Investigations that include different physical and social contexts, including a range of cultures, are necessary to fully understand head control. Sixth, this study focused on infants with typical development as a first step. In terms of clinical implications, the key effects of training will not be known until after studying infants with special needs. Future studies 946 f Physical Therapy can build on these findings but will need to tailor the methods and hypotheses to the patient population, age, and level of experience of the cohort of these clinical trials. Both authors provided concept/idea/research design, writing, and project management. Dr Lee provided data collection and analysis. Dr Galloway provided fund procurement, facilities/equipment, institutional liaisons, and consultation (including review of the manuscript before submission). The authors thank all of the infants and their parents for their effort and enthusiasm for participation. They also thank many undergraduate assistants for their help with data collection and processing. Preliminary data from this study were presented at PT 2009: Annual Conference and Exposition of the American Physical Therapy Association; June 10 –13, 2009; Baltimore, Maryland. Parts of the manuscript were presented at the XVIIth Biennial International Conference on Infant Studies; March 10 –14, 2010; Baltimore, Maryland; and the North American Society for the Psychology of Sport and Physical Activity (NASPSPA) Annual Conference; June 10 –14, 2010; Tucson, Arizona. DOI: 10.2522/ptj.20110196 References 1 Prechtl H. Prenatal and early postnatal development of human motor behavior. In: Kalverboer A, Gramsbergen A, eds. Handbook of Brain and Behaviour in Human Development. Norwell, MA: Kluwer Academic Publishers; 2001:415– 428. 2 Bertenthal B, Von Hofsten C. Eye, head and trunk control: the foundation for manual development. Neurosci Biobehav Rev. 1998;22:515–520. 3 Bobath K. A Neurophysiological Basis for the Treatment of Cerebral Palsy. 2nd ed. London, England: William Heinemann Medical Books Ltd; 1980. 4 Kramer JF, Ashton B, Bander R. Training of head control in the sitting and semi prone positions. Child Care Health Dev. 1992; 18:365–376. 5 Gassier J. A Guide to the Psycho-Motor Development of the Child. New York, NY: Churchill Livingstone Inc; 1984. 6 Gesell A, Thompson H. The Psychology of Early Growth. New York, NY: The Macmillan Company; 1938. 7 McMraw MB. The Neuromuscular Maturation of the Human Infant. London, United Kingdom: Haffner Publishing; 1943. 8 World Health Organization, Multicentre Growth Reference Study Group. WHO Motor Development Study: windows of achievement for six gross motor development milestones. Acta Paediatr Suppl. 2006;450:86 –95. 9 Woollacott MH, Shumway-Cook A. Changes in postural control across the life span: a system approach. Phys Ther. 1990; 7:779 – 807. 10 Adolph KE, Karasik LB, Tamis-LeMonda CS. Moving between cultures: crosscultural research on motor development. In: Bornstein MH, ed. Handbook of CrossCultural Development Science. Hillsdale, NJ: Lawrence Erlbaum Associates; 2009: 61– 88. Domains of Development Across Cultures; vol 1. 11 Bayley N. Bayley Scales of Infant and Toddler Development. 3rd ed. San Antonio, TX: Harcourt Assessment Inc; 2006. 12 Campbell SK, Girolami GL, Kolobe THA, et al. The Test of Infant Motor Performance. Chicago, IL: Infant Motor Performance Scales LLC; 1993. 13 Folio MR, Fewell RR. Peabody Developmental Motor Scales: Examiner’s Manual. 2nd ed. Austin, TX: Pro-ED; 2000. 14 Piper MC, Darrah J. Motor Assessment of the Developing Infant. Philadelphia, PA: WB Saunders Co; 1994. 15 Scherzer AL, Tscharnuter I. Early Diagnosis and Therapy in Cerebral Palsy: A Premier on Infant Developmental Problems. 2nd ed. New York, NY: Marcel Dekker; 1990. 16 Barbosa VM, Campbell SK, Smith E, Berbaum M. Comparison of Test of Infant Motor Performance (TIMP) item responses among children with cerebral palsy, developmental delay, and typical development. Am J Occup Ther. 2005;59: 446 – 456. 17 Aylward GP, Hatcher RP, Leavitt LA, et al. Factors affecting neurobehavioral responses of preterm infants at term conceptional age. Child Dev. 1984;55:1155– 1165. 18 Forslund M, Bjerre I. Neurological assessment of preterm infants at term conceptional age in comparison with normal fullterm infants. Early Hum Dev. 1983;8: 195–208. 19 Jeng S, Tsou Yan K, Teng R. Neurobehavioral development at term in very low birthweight infants and normal term infants in Taiwan. Early Hum Dev. 1998; 51:235–245. 20 Palmer PG, Dubowitz LMS, Verghote M, Dubowitz V. Neurological and neurobehavioural differences between preterm infants at term and full-term newborn infants. Neuropediatrics. 1982;13:183– 189. 21 Mercuri E, Guzzetta A, Laroche S, et al. Neurologic examination of preterm infants at term age: comparison with term infants. J Pediatr. 2003;142:647– 655. 22 Ricci D, Romeo DM, Haataja L, et al. Neurological examination of preterm infants at term equivalent age. Early Hum Dev. 2008;84:751–761. Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 July 2012 Early Intensive Postural and Movement Training in Very Young Infants 23 Leiper CI, Miller A, Lang J, Herman R. Sensory feedback for head control in cerebral palsy. Phys Ther. 1981;61:512–518. 24 Mital MA, Belkin SC, Sullivan MA. An approach to head, neck and trunk stabilization and control in cerebral palsy by use of the Milwaukee brace. Dev Med Child Neurol. 1976;18:198 –203. 25 Wooldridge CP, Russell G. Head position training with the cerebral palsied child: an application of biofeedback techniques. Arch Phys Med Rehabil. 1976;57:407– 414. 26 Cameron EC, Maehle V. Comparison of active motor items in infants born preterm and infants born full term. Pediatr Phys Ther. 2006;18:197–203. 27 Lobo MA, Galloway JC, Savelsbergh GJ. General and task-related experiences affect early object interaction. Child Dev. 2004;75:1268 –1281. 28 Shumway-Cook A, Woollacott MH. Motor Control: Translating Reach Into Clinical Practice. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007. 29 Angulo-Kinzler RM, Ulrich B, Thelen E. Three-month-old infants can select specific leg motor solutions. Motor Control. 2002;6:52– 68. 30 Hadders-Algra M, Brogren E, Forssberg H. Training affects the development of postural adjustments in sitting infants. J Physiol. 1996;493:289 –298. 31 Lagerspetz K, Nygard M, Strandvik C. The effects of training in crawling on the motor and mental development of infants. Scand J Psychol. 1971;12:192–201. 32 Lobo MA, Galloway JC. Postural and object-oriented experiences advance early reaching, object exploration, and meansend behavior. Child Dev. 2008;79:1869 – 1890. 33 Needham A, Barnett T, Peterman K. A pick-me-up for infant’s exploratory skills: early simulated experiences reaching for objects using “sticky mittens” enhances young infants’ object exploration skills. Infant Behav Dev. 2002;25:279 –295. 34 Rovee CK, Rovee DT. Conjugate reinforcement of infant exploratory behavior. J Exp Child Psychol. 1969;8:33–39. 35 Sveistrup H, Woollacott MH. Practice modifies the developing automatic postural response. Exp Brain Res. 1997;114:33– 43. 36 Thelen E. 3-month-old infants can learn task-specific patterns of interlimb coordination. Psychol Sci. 1994;5:280 –285. 37 Zelazo NA, Zelazo PR, Cohen KM, Zelazo PD. Specificity of experience effects on elementary neuromotor patterns. Dev Psychol. 1993;29:686 – 691. 38 Blauw-Hospers CH, Hadders-Algra M. A systematic review of the effects of early intervention on motor development. Dev Med Child Neurol. 2005;47:421– 432. 39 Damiano DL. Rehabilitative therapies in cerebral palsy: the good, the not as good, and the possible. J Child Neurol. 2009;24: 1200 –1204. July 2012 40 Hopkins B. Culturally determined patterns of handling the human infant. Journal of Human Movement Studies. 1976;2:1–27. 41 Hopkins B, Westra T. Maternal handling and motor development: an intracultural study. Genet Soc Gen Psychol Monogr. 1988;114:379 – 408. 42 Hopkins B, Westra T. Motor development, maternal expectations, and the role of handling. Infant Behav Dev. 1990;13:117– 122. 43 Rabain-Jamin J, Wornham WL. Practice and representations of child care and motor development among West Africans in Paris. Early Development and Parenting. 1993;2:107–119. 44 Super CM. Environmental effects on motor development: the case of “African infant precocity.” Dev Med Child Neurol. 1976; 18:561–567. 45 Campbell SK, Kolobe THA. Concurrent validity of the Test of Infant Motor Performance with the Alberta Infant Motor Scale. Pediatr Phys Ther. 2000;12:1– 8. 46 Campbell SK, Kolobe THA, Osten ET, et al. Construct validity of the Test of Infant Motor Performance. Physi Ther. 1995;75: 585–596. 47 Campbell SK, Hedeker D. Validity of the Test of Infant Motor Performance for discriminating among infants with varying risk for poor motor outcome. J Pediatr. 2001;139:546 –551. 48 Campbell SK, Levy P, Zawacki L, Liao P-J. Population-based age standards for interpreting results on the Test of Infant Motor Performance. Pediatr Phys Ther. 2006;18: 119 –125. 49 Campbell SK, Kolobe THA, Wright B, Linacre JM. Validity of the Test of Infant Motor Performance for prediction of 6-, 9-, and 12-month scores on the Alberta Infant Motor Scale. Dev Med Child Neurol. 2002; 44:263–272. 50 Barbosa VM, Campbell SK, Sheftel D, et al. Longitudinal performance of infants with cerebral palsy on the Test of Infant Motor Performance and on the Alberta Infant Motor Scale. Phys Occup Ther Pediatr. 2003;23:7–29. 51 Flegel J, Kolobe THA. Predictive validity of the Test of Infant Motor Performance as measured by the Bruininks-Oseretsky Test of Motor Proficiency at school age. Phys Ther. 2002;82:762–771. 52 Kolobe THA, Bulanda M, Susman L. Predicting motor outcome at preschool age for infants tested at 7, 30, 60, and 90 days after term age using the Test of Infant Motor Performance. Phys Ther. 2004;84: 1144 –1156. 53 Lekskulchai R, Cole J. Effect of a developmental program on motor performance in infants born preterm. Aust J Physiother. 2001;47:169 –176. 54 Heathcock J, Lobo MA, Galloway JC. Movement training advances the emergence of reaching in infants born less than 33 weeks gestational age. Phys Ther. 2008; 88:310 –322. 55 Soderkvist I, Wedin PA. Determining movements of the skeleton using wellconfigured markers. J Biomech. 1993;26: 1473–1477. 56 Rosenthal R. Effect sizes: Pearson’s correlation, its display via the BESD, and alternative indices. Am Psychol. 1991;46: 1086 –1087. 57 Thelen E, Corbetta D, Spencer J. Development of reaching during the first year: role of movement speed. J Exp Psychol Hum Percept Perform. 1996;22:1059 –1076. 58 Mildred J, Beard K, Dallwitz A, Unwin J. Play position is influenced by knowledge of SIDS sleep position recommendations. J Paediatr Child Health. 1995;31:499 –502. 59 Salls JS, Silverman LN, Gatty CM. The relationship of infant sleep and play positioning to motor milestone achievement. Am J Occup Ther. 2002;56:577–580. 60 Majnemer A, Barr RG. Influence of supine sleep positioning on early motor milestone acquisition. Dev Med Child Neurol. 2005;47:370 –376. 61 Bly L. The Components of Normal Movement During the First Year of Life and Abnormal Motor Development. Chicago, IL: Neuro-Developmental Treatment Association; 1983. 62 Clark D, Kreutzberg J, Chee F. Vestibular stimulation influence on motor development in infants. Science. 1977;196:1228 – 1229. 63 Neal M. Vestibular stimulation and developmental behavior of the small premature infant. Nurs Res Rep. 1968;3–5. 64 Fredrickson WT, Brown JV. Posture as a determinant of visual behavior in newborns. Child Dev. 1975;46:579 –582. 65 Gregg CL, Haffner ME, Korner AF. The relative efficacy of vestibularproprioceptive stimulation and the upright position in enhancing visual pursuit in neonates. Child Dev. 1976;47:309 – 314. 66 Pederson D, TerVrugt D. The influence of amplitude and frequency of vestibular stimulation on the activity of two-monthold infants. Child Dev. 1973;44:122–128. 67 Pin T, Eldridge B, Galea MP. A review of the effects of sleep position, play position, and equipment use on motor development in infants. Dev Med Child Neurol. 2007;49:858 – 867. 68 TerVrugt D, Pederson D. The effect of vertical rocking frequencies on the arousal level in two-month-old infants. Child Dev. 1973;44:205–209. 69 Orton J, Spittle A, Doyle L, et al. Do early intervention programmes improve cognitive and motor outcomes for preterm infants after discharge? A systematic review. Dev Med Child Neurol. 2009;51: 851– 859. 70 Ketelaar M, Vermeer A, Helders PJM. Functional motor abilities of children with cerebral palsy: a systematic literature review of assessment measures. Clin Rehabil. 1998; 12:369 –380. Volume 92 Number 7 Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012 Physical Therapy f 947 Early Intensive Postural and Movement Training Advances Head Control in Very Young Infants Hui-Min Lee and James Cole Galloway PHYS THER. 2012; 92:935-947. Originally published online March 30, 2012 doi: 10.2522/ptj.20110196 References This article cites 57 articles, 11 of which you can access for free at: http://ptjournal.apta.org/content/92/7/935#BIBL Subscription Information http://ptjournal.apta.org/subscriptions/ Permissions and Reprints http://ptjournal.apta.org/site/misc/terms.xhtml Information for Authors http://ptjournal.apta.org/site/misc/ifora.xhtml Downloaded from http://ptjournal.apta.org/ at APTA Member on July 25, 2012