PATHOPHYSIOLOGY COURSE - ENDOCRINE MODULE CHAPTER 1 Mechanisms of Hormone Action
advertisement

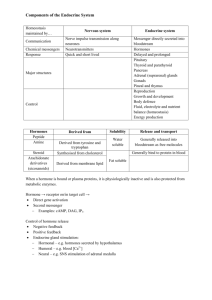
PATHOPHYSIOLOGY COURSE - ENDOCRINE MODULE CHAPTER 1 Mechanisms of Hormone Action Samuel Dagogo-Jack, M.D. Monday, November 30, 2009, 8:00-8:50am Objectives: 1. Define hormone and various forms of cellular communication (i.e., endocrine, paracrine, autocrine and juxtacrine) and endocrine rhythm. 2. Classify major hormones, their glandular source and their types. 3. Distinguish between the two classes of hormones, their characteristics, and site of action on target tissue. 4. Recognize various forms of hormone receptor-interaction and mechanisms of hormone action. 5. Define general principle of peptide hormone synthesis. 6. Explain negative and positive feedback in hormone physiology. 7. Assess various methodologies of hormone measurement and endocrine function tests. 8. Cite general classification of endocrine disorders. 9. Relate possible mechanisms of hormone resistant states. 10. Understand new concept on the role of fat tissue as a major endocrine organ. OVERVIEW Introduction Study of the pathophysiology of endocrine disorders requires basic knowledge of endocrine anatomy, physiology, and biochemistry, as well as pathology. In this course we assume adequate knowledge of the anatomy, physiology, and biochemistry of the endocrine glands. However, a brief review of the major concepts will be made to better understand the pathophysiology. Mechanisms of Hormone Action 1-1 As each major topic in the endocrine module will be prefaced by a review of the basic principles, this overview will not deal with individual glands, but rather it will emphasize the general principles of endocrine gland physiology and assessment of their functions. DEFINITION OF HORMONE The term “hormone” was introduced by Starling in 1905. It is derived from the Greek meaning “to arouse”. Hormones are chemicals that are produced by “ductless” glands, secreted into circulation in nanomolar concentrations and affect target tissues away from the site of their secretion. _____________________________________________________________________ TABLE 1 Concentration of Hormones in the Body (Compared to Glucose and K+) _____________________________________________________________________ Plasma Concentration Pancreas (10-9 M) Insulin Glucagon 1 20 Adrenal Cortisol Epinephrine 300 5 Plasma Glucose or K+ 5,000,000 _____________________________________________________________________ Various Forms of Cellular Communications Endocrine: “Transmitter” reaches the target tissue through circulation, e.g., ACTH stimulates cortisol production in adrenal. Paracrine: “Transmitter” reaches the target tissue in the vicinity of its secretion, e.g., Angiotensin II in the kidney. Juxtacrine: “Transmitter” in membrane of one cell can interact with receptor of a cell next to it, e.g., hematopoietic growth factor. Autocrine: “Transmitter” can act on the same cell that released it, e.g., Insulin from β cell can inhibit its own secretions. Mechanisms of Hormone Action 1-2 Figure 1 Targ et cell Targ et Cell H H H Autocrine Endocrine Paracrine Neuron Neuron Neuroendocrine Neurotransm itter Targ et Cell Endocrine Rhythm Essentially all hormones are secreted in rhythmic and cyclic pattern. These patterns may have various controlling mechanisms such as light, deep sleep or awakening and other external causes. There are three types of rhythm. 1. 2. 3. Circadian - 24 hour cycle Ultradian - shorter than 24 hour cycle Infradian - longer than 24 hour cycle (i.e. menstrual cycle in women) Mechanisms of Hormone Action 1-3 TABLE 2 The Major Endocrine Glands and Their Characteristic Hormones _____________________________________________________________________ Structural Gland Hormone Characteristics Hypothalamus and median eminence Anterior Pituitary TRH Somatostatin GNRH CRH GHRH Prolactin-inhibiting factor (dopamine) Peptide Biogenic amine TSH LH FSH Glycoprotein GH Prolactin ACTH Protein ADH (Vasopressin) Oxytocin Peptide Thyroid T4, T3 Calcitonin Tyrosine derivatives Peptide Parathyroid PTH Peptide Adrenal Cortex Aldosterone, Cortisol Androgens and estrogens Steroids Adrenal Medulla Epinephrine and Norepinephrine Catecholamines Stomach Gastrin GLP-1 Peptide Peptide Pancreas (islets of Langerhans) Glucagon (α cell) Insulin (β cell) Somatostatin (D cell) Pancreatic polypeptide (F cell) Amylin Duodenum and jejunum Secretin Cholecystokinin Protein Ovary Estrogen, progesterone Steroid Testis Testosterone Steroid Fat tissue Adipokines protein & cytokines Posterior Pituitary Mechanisms of Hormone Action Protein 1-4 Fat Tissue as a Major Endocrine Gland Although in previous years it was assumed that fat tissue, similar to bone, is not an active tissue, subsequent works have proven that both concepts about bone and fat tissue were wrong. It is now believed that fat tissue is an important endocrine organ and produces many compounds which play important roles in the body’s metabolic balance, which will be discussed in more detail (Chapter 5) Figure 2 provides the latest information on all the chemicals that are produced by fat cells, which are collectively call “adipokines”. Some of these are hormones; others are cytokines, some of which are important cardiovascular risk factors and are associated with insulin resistance (i.e. TNFα, IL6, Resistin, CRP, FFA, & PAI-1). Adipokines Visfatin is a newly discovered hormone isolated from fat tissue and has insulin-like activity (Science 307:366-7, 2005) Hormonal Classification In general, endocrine glands secrete one of two types of hormones in the circulation. These could be classified as (a) polypeptide hormones (and catecholamines), and (b) steroid hormones (and thyroid hormones). Each class has special characteristics which are summarized in the accompanying table. Mechanisms of Hormone Action 1-5 TABLE 3 General Classification of Hormones Properties Polypeptides Steroids MOLECULAR WEIGHT Large (i.e., >500) Small (i.e., <500) TIME OF ACTION Fast (minutes) Slow (hours) FORM IN CIRCULATION Free (unbound) Bound to blood HALF LIFE IN BLOOD Minutes Hours SITE OF ACTION ON THE TARGET TISSUE Specific receptor on cell membrane Specific receptor in the cytoplasm or nucleus MECHANISM OF ACTION Produce 2nd messenger Activation of the (transcription) MOLECULAR BASIS OF ACTION Phosphorylation or dephosphorylation of enzyme Synthesis of new protein in cytoplasm TRANSPORT AND SECRETION MECHANISM Vesicle-mediated transport, released by fusion of vesicle with plasma membrane nonvascular manner by specific transporter or diffusion Mechanism of Hormone Transport in the Blood 1. 2. 3. Bound (Steroids and Thyroid) Free (Peptides) Others Mechanisms of Hormone Action 1-6 TABLE 4 MECHANISM OF HORMONE-RECEPTOR INTERACTION A. Peptide Hormones and Neurotransmitter Receptor Family Type 1. NH Example Seven transmembrane domain β Adrenergic PTH GRH LH Glucagon TSH Dopamine ACTH TRH 2 Plasma Memb ran e Cy tosol CO H 2 2. One or two transmembrane domains Growth factor receptors 3. a. Group I - Receptor contains intrinsic enzyme i.e. tyrosine kinase Insulin IGF EGF b. Group II - no intrinsic tyrosine kinase GH Prolactin Erythropoietin Interleukin 2 Guanylyl Cyclase-linked receptors Natriuretic peptides B. Steroid Receptor Family Cytoplasmic receptor involving heat shock protein (HSP). When steroid hormone binds to the receptor, HSP dissociates. This initiates transport of the receptor into the nucleus. C. Thyroid Receptor Family Includes thyroid receptor, retinoic acid receptor, vitamin D receptor. They are bound to chromatin in the cell nucleus. Mechanisms of Hormone Action 1-7 Figure Figure 32 MECHANISM OF SYNTHESIS OF PEPTIDE HORMONE TATA Ex on Intron Exon Intron Exon Gene-DNA 5'end 3'end Start Stop Promoter STRUCTURAL GENE Transc ription Pre-mRNA Post trans cription Mature m RNA Translation Pre-hormone (Prepeptide) Post-trans lation Hormone (peptide) Mechanisms of Hormone Action 1-8 Figure 43 FIGURE EXAMPLES OF NEGATIVE AND POSITIVE FEEDBACK IN ENDOCRINOLOGY STRESS STIMULI Negativ e Hy pothalam us C RH Posterior Pituitary Positiv e Oxy tocin Negativ e Anterior Pituitary Cerv ic al Rec eptor Oxy tocin ACTH Positiv e Feedbac k (terminates with deliv ery of f etus) Adrenal Cortex Cortis ol Negativ e Feedback Mechanisms of Hormone Action 1-9 Feedback Control (Figure 4) Negative - Most common type of control. Signal stimulates release of hormone which in turn feedbacks to the gland to reduce the signal and decrease hormone production. (Example: adrenal, thyroid, parathyroid, pancreas) Positive - Rare mechanism. Original signal for hormone production is further stimulated by the signal to produce more hormone. Example: oxytocin release from PosteriorPituitary with labor pain. This activates cervical receptor to stimulate more oxytocin release to accommodate expulsion of the fetus, but terminates with the delivery of the fetus. Hormone Measurements and Assessment of Endocrine Function Evaluation of endocrine function in clinical medicine requires, above all else, a thorough history and physical examination of the patient which should form the basis of further investigation and elucidation of pathogenesis. Without such a basic assessment, the physician may subject the patient to unnecessary tests resulting in excess discomfort, pain, and even harm, as well as financial burden. Following is the list of methods for hormonal measurement: Bioassay: A means of eliciting a specific physiologic response in an animal or living biological preparation by a crude or purified hormone. This method usually is not sensitive and requires large amounts of blood. Chemical measurement: Determination of hormones by chemical method. It is more sensitive than bioassay, but drugs may interfere with its measurement. Radioimmunoassay (RIA): A specific antibody is harvested in an animal which will be used in this test to bind the hormone in question. The amount of hormone in a biological specimen (usually plasma) may then be quantitated by altering the extent of displacement of trace amounts of the radioactively-labeled (e.g., 131I) hormone by the nonradioactive hormone in a sample to be tested. This method is extremely sensitive and can detect physiologic levels of hormones with as little as 0.05 ml of blood. However, the RIA method does not distinguish between active or inactive hormones. Enzyme-Linked ImmunoSorbent Assay (ELISA): ELISA, also called Enzyme ImmunoAssay or EIA, is similar in hormone detection principle to RIA, except that a nonradioactive (chemical) signal is used. In a typical ELISA test, an unknown amount of antigen is affixed to a surface, and exposed to a specific antibody so that it can bind to the antigen. The antibody is linked to an enzyme, and in the final step a substance (conjugate) is added that the enzyme can convert to some detectable signal. For example, in fluorescence ELISA, the antigen/antibody complex fluoresces upon exposure to light of the appropriate wavelength. Mechanisms of Hormone Action 1-10 Radioreceptor assay: This method is similar to RIA, but uses highly specific receptors on cells or subcellular constituents rather than antibodies to measure biologically active hormones. It is highly sensitive. In certain cases all the above tests may be utilized. However, the most common and frequently used method for hormone assay is RIA. 1. Stimulation test: A hormone is used to elicit response from a target tissue, i.e., ACTH stimulation test to elicit glucocorticoid secretion from the adrenal glands. 2. Suppression test: A physiologic or pharmacologic dose of a hormone is used to assess feedback regulation of a hormone from the gland, i.e., in the dexamethasone suppression test, the administration of potent exogenous glucocorticoiddexamethasone (which does not interfere with cortisol measurement) suppresses endogenous production of the natural glucocorticoid (hydrocortisone-cortisol) from the adrenal gland, under physiological conditions. 3. Secretion rate: Amount of hormone secreted/unit time. 4. Production rate: Hormone produced outside of the gland. 5. Half life in blood: Time for hormone in the blood to fall to half of its original level or concentration. 6. Protein-bound fraction: The part of the hormone bound to a plasma-binding protein (inactive hormone). 7. Free or unbound fraction: The part of the hormone circulating free in the blood (active hormone). General Classification of Endocrine Disorders Endocrine disorders may be classified under two general categories: (1) Hyperfunction or (2) Hypofunction, each with the following subclassifications: a. Primary: increased (hyperfunction) or decreased (hypofunction) secretion from the target gland (e.g., cortisol from adrenals). b. Secondary: increased or decreased secretion of trophic hormone (e.g., ACTH from pituitary) with resistant increase in target hormone (e.g. cortisol). c. Tertiary: increase or decrease of releasing hormone (e.g., CRH from hypothalamus) with resistant increase in the trophic and thence the target hormone. Mechanisms of Hormone Action 1-11 Hormone Receptor Interaction and Possible Mechanism of Hormone Resistant States As important as hormone hyper- and hyposecretion is in the pathogenesis of hormone disorders, equally important is an abnormality of the hormone receptor which could be the result of: 1. decreased receptor number or affinity on the target tissue (decreased sensitivity); 2. decreased receptor responsiveness (postreceptor defect); 3. combination of 1 and 2 (decreased sensitivity and decreased responsiveness). Mechanisms of Hormone Action 1-12 120 ____ % Maximal Response __ 100 Normal Response ____ __ 80 Decreased Sensitivity ____ __ 60 Decreased Responsiveness ____ __ 40 ____ Decreased Sensitivity and Responsiveness __ 20 ____ __ 0 0.01 0.1 1 10 100 Hormone Concentration (nM) Figure 5: Types of resistance to hormone action. In hormone -resistant states there may be a rightward shift of the dose -response curve (decreased sensitivity), a decrease in maximal response (decreased re sponsiveness), or a combination of the two. Decreased sensitivity indicates a defect at a non -ratelimiting step (often the receptor), whereas decreased responsiveness indicates a defect at a rate-limiting step (usually post receptor). (Adapted from Kahn CR). Insulin resistance, insulin insensitivity and insulin unresponsiveness: a necessary distinction. Metabolism 1978; 27 [Suppl 2]: 1893 -1902.) Mechanisms of Hormone Action 1-13