埼玉医科大学総合医療センター 協力:川越市幸町自治会
advertisement

Journal Club
Turchin A, Matheny ME, Shubina M, Scanlon JV, Greenwood B, Pendergrass ML.
Hypoglycemia and Clinical Outcomes in Patients With Diabetes Hospitalized in the
General Ward
Diabetes Care 32:1153–1157, 2009
Uebele VN, Gotter AL, Nuss CE, Kraus RL, Doran SM, Garson SL, Reiss DR, Li Y,
Barrow JC, Reger TS, Yang ZQ, Ballard JE, Tang C, Metzger JM, Wang SP, Koblan KS,
Renger JJ.
Antagonism of T-type calcium channels inhibits high-fat diet-induced weight gain in
mice.
Clin Invest. 2009 Jun;119(6):1659-67. doi: 10.1172/JCI36954. Epub 2009 May 18.
2009年7月16日 8:30-8:55
8階 医局
埼玉医科大学 総合医療センター 内分泌・糖尿病内科
Department of Endocrinology and Diabetes,
Saitama Medical Center, Saitama Medical University
松田 昌文
Matsuda, Masafumi
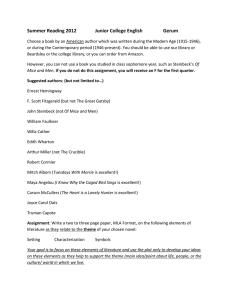
計画概要
世界糖尿病デー川越地区ブルーライトアップ
主催:世界糖尿病デー実行委員会(代表:堀田 饒,委員長:清野 裕)
後援:埼玉県糖尿病対策推進会議,川越市,川越市医師会,埼玉県医師会,JADEC埼玉県支部,
埼玉医科大学総合医療センター
協力:川越市幸町自治会,川越市大手町自治会
コーディネーター:埼玉医科大学総合医療センター内分泌・糖尿病内科(川越地区ブルーライトアップ実行委員会)
開催日:2009年11月14日(土曜日) 開催時間:17:00-22:00 (点灯式17:00-,点灯17:00-22:00)
問合せ先担当者e-mail:matsudam@saitama-med.ac.jp, mako@saitama-med.ac.jp
イベント:糖尿病撲滅のため川越市のシンボルである時の鐘をシンボルカラーの「ブルー」にライトアップ、啓
発ポスター作製 等の活動を通じ、糖尿病の予防を呼びかける。9月以降に行われる川越地区の糖尿
病関連の行事(講演会、健康相談など)でライトアップ実施に関連した情報を提供する。
時の鐘
点灯イメージ
1Brigham and Women’s Hospital, Boston, Massachusetts; the 2Clinical
Informatics Research and Development, Partners HealthCare System, Boston,
Massachusetts; 3Harvard Medical School, Boston, Massachusetts; the
4Vanderbilt Medical Center, Nashville, Tennessee; the 5Tennessee Valley
Healthcare System, Veteran’s Administration, Nashville, Tennessee; the
6Massachusetts College of Pharmacy and Health Sciences, Worcester,
Massachusetts; and 7Medco Health Solutions, Inc., Franklin Lakes, New
Jersey.
Diabetes Care 32:1153–1157, 2009
Background and Aim
Hypoglycemia is associated with
adverse outcomes in mixed populations
of patients in intensive care units. It is
not known whether the same risks exist
for diabetic patients who are less
severely ill. In this study, we aimed to
determine whether hypoglycemic
episodes are associated with higher
mortality in diabetic patients
hospitalized in the general ward.
Methods
This retrospective cohort study
analyzed 4,368 admissions of 2,582
patients with diabetes hospitalized in
the general ward of a teaching hospital
between January 2003 and August 2004.
The associations between the number
and severity of hypoglycemic (≦50
mg/dl) episodes and inpatient mortality,
length of stay (LOS), and mortality
within 1 year after discharge were
evaluated.
Results
Hypoglycemia was observed in 7.7% of
admissions.
In multivariable analysis, each additional day
with hypoglycemia was associated with an
increase of 85.3% in the odds of inpatient death
(P < 0.009) and 65.8% (P < 0.0003) in the odds of
death within 1 year from discharge.
The odds of inpatient death also rose threefold
for every 10 mg/dl decrease in the lowest blood
glucose during hospitalization (P < 0.0058).
LOS increased by 2.5 days for each day with
hypoglycemia (P < 0.0001).
Conclusion
Hypoglycemia is common in diabetic
patients hospitalized in the general
ward. Patients with hypoglycemia
have increased LOS and higher
mortality both during and after
admission. Measures should be
undertaken to decrease the
frequency of hypoglycemia in this
high-risk patient population.
Voltage-gated (dependent)
Calcium channel
a complex of several different subunits: α1, α2δ, β1-4, and γ. The α1
subunit forms the ion conducting pore while the associated
subunits have several functions including modulation of gating.
Ligand-gated
国内発売のカルシウム拮抗薬と
交感神経への作用からみた世代分類
交感神経系への
作用からみた
世代分類
Ⅰ
Ⅱ
交感神経
機能
一般名
Ⅳ
:活性化,
商品名
NE遊離に
対する作用
(摘出血管)
降圧時の
血漿中NE濃度
(SHR)
塩酸ベラパミル
(1965)
ワソラン
塩酸ジルチアゼム
(1974)
ヘルベッサー
ニフェジピン
(1976)
アダラート
作用なし
上昇(+++)
塩酸ニカルジピン
(1981)
ペルジピン
作用なし
上昇(+++)
ニルバジピン
(1989)
ニバジール
塩酸マニジピン
(1990)
カルスロット
ニトレンジピン
(1990)
バイロテンシン
ニソルジピン
(1990)
バイミカード
塩酸ベニジピン
(1991)
コニール
塩酸バルニジピン
(1992)
ヒポカ
(1995)
ランデル
フェロジピン
(1995)
ムノバール
アラニジピン
(1996)
サプレスタ
ベシル酸アムロジピン
(1993)
ノルバスク
アムロジン
アゼルニジピン
(2003)
カルブロック
(1995)
アテレック
塩酸エホニジピン
Ⅲ
発売年
シルニジピン
L/T型
L/N型
:抑制,NE:ノルエピネフリン,SHR:自然発症高血圧ラット
上昇(++)
上昇(++)
作用なし
上昇(+)
抑制
変化なし
高原 章 他. Mebio 2005; 22: 89-100
J. Clin. Invest. 119:1659–1667 (2009). doi:10.1172/JCI36954
BACKGROUND AND FINDINGS
The epidemics of obesity and metabolic disorders
have well-recognized health and economic
burdens. Pharmacologic treatments for these
diseases remain unsatisfactory with respect to
both efficacy and side-effect profiles. Here, we
have identified a potential central role for T-type
calcium channels in regulating body weight
maintenance and sleep. Previously, it was shown
that mice lacking CaV3.1 T-type calcium channels
have altered sleep/wake activity. We found that
these mice were also resistant to high-fat diet–
induced weight gain, without changes in food
intake or sensitivity to high-fat diet–induced
disruptions of diurnal rhythm.
METHODS
All animal procedures were approved by, and conducted according to the standards of, the Merck IACUC.
KO mice. Cacna1g KO mice were obtained from Deltagen on a mixed C57B6/Sv129 background and bred in a heterozygous
× heterozygous manner at Taconic. Male Cacna1g KO mice and WT littermates were placed on a HFD (D12492; Research
Diets Inc.) for 11 days. Body weight was monitored weekly.
Core body temperature and ambulatory activity was monitored continuously in adult Cacna1g homozygote KO animals, WT
littermates, and C57BL/6 mice through radio telemetry transmitters (TA10TA-F20; Data Sciences International) implanted
peritoneally. Temperatures for individual subjects were averaged over a 30-minute interval, while activity, expressed as
animal movements in the xy plane over the home cage radio receiver, was calculated as the sum of active movements over
the 30-minute epoch. Plotted values for each group are averages of these 30-minute measures.
Compound identification and selectivity assessment. The potency of TTA-A2 [2-(4-Cyclopropylphenyl)-N-((1R)-1-{5-[(2,2,2trifluoroethyl)oxo]pyridin- 2-yl}ethyl)acetamide] in depolarized and hyperpolarized FLIPR assay conditions was evaluated
as described previously (37). We further tested TTAA2 for functional potency against CACNA1C (CaV1.2, L-type), CACNA1A
(CaV2.1, P/Q-type), CACNA1B (CaV2.2, N-type), and CACNA1E (CaV2.3, R-type) calcium channels as described previously
(51). Finally, an array of 170 additional targets was screened in functional and binding assays at MDS Pharma Services
according to standard protocols.
Electrophysiological verification. Whole-cell patch-clamp recordings on HEK-293 cells expressing human CaV3.1 were
performed at room temperature. Currents were recorded using either a HEKA EPC-9 or an Axopatch 200B patch-clamp
amplifier. Data were stored on a personal computer equipped with acquisition software HEKA Pulse version 8.5 and
analyzed using Pulsefit (HEKA), Igor Pro version 4.0, and GraphPad Prism version 4 (for EPC-9 amplifier) or using Clampex
9, Clampfit (Axon Instruments), and Origin 7.0 (for 200B amplifier). Patch pipettes were made from borosilicate glass tubing
(Warner Instruments) and fire polished, and had a resistance of 1–5 MÙ. Series resistance was compensated, and the
capacitance artifact was canceled using the amplifier’s built-in circuitry. Leak current was corrected with a P/4 protocol.
Patch pipettes contained 125 mM CsCl, 10 mM TEA-Cl, 10 mM HEPES, 8 mM NaCl, 0.06 mM CaCl2, 0.6 mM EGTA, 4 mM MgATP, and 0.3 mM GTP, and pH was adjusted to 7.2 with CsOH. Extracellular solution was based on Tyrode solution and
contained 130 mM NaCl, 4 mM KCl, 30 mM glucose, 20 mM HEPES, 1 mM MgCl2, and 2 mM CaCl2, and pH was adjusted to
7.4 with NaOH. Baseline T-type calcium currents were elicited by depolarizing to –20 mV for 70 milliseconds, cycling every
10 seconds from a holding potential of –100 mV and every 20 seconds from a holding potential of –80 mV.
METHODS
Central exposure of TTA-A2. TTA-A2 was administered to male Sprague- Dawley rats (n = 3) by oral gavage at a dose of 10
mg/kg (10% Tween in 0.5% methylcellulose). Blood, brain, and CSF samples were collected upon sacrifice at 1 hour after
dosing. The blood samples were collected into tubes containing EDTA, and plasma was prepared by centrifugation. Brain
samples were homogenized in water (25% w/w) with a SPEX Certiprep 2000 Geno/Grinder. CSF samples were collected into
tubes containing acetonitrile, and all samples were stored at –20°C until analysis. Samples were prepared for analysis
using a protein precipitation method and analyzed by LC-MS/MS under a validated protocol.
Compound effects on active wake. Sprague-Dawley rats (n = 8) were implanted with electrocorticogram (ECoG) and
electromyogram (EMG) telemetry monitors and recorded in a 7-day crossover dosing paradigm and scored for sleep stage
as previously described (52). At 5 hours after lights off, 3, 10, or 30 mg/kg TTA-A2 or vehicle (0.5% methylcellulose) was
administered by oral gavage. The results for all 8 animals were averaged by treatment over 7 administration nights.
Growing diet-induced obesity. WT C57BL/6NTac mice (Taconic) were acclimated to reverse lighting, handling, and dosing;
divided into 4 cohorts; and weighed weekly. Animals received vehicle (10% Tween in 0.5% methylcellulose) or 10 mg/kg
TTA-A2 and were fed either normal chow (7912; Harlan Teklad) or the high-carbohydrate HFD (D12492; Research Diets Inc.).
Food intake was measured by weighing food weekly. Body composition was measured by qNMR at 0, 8, and 13 weeks of
treatment. This study was performed at Taconic (Germantown, NY).
For studies in which core temperature and activity were monitored before and after the transition to HFD, body weight and
food consumption was measured at 12-hour intervals at the dark-to-light and light-todark transitions. Chow spillage and
hoarding was minimized by using food jars, providing access to food through lids perforated with 1.5-cm openings, and
care was taken to include any displaced chow fragments in food weight measurements.
Established diet-induced obesity. C57BL/6NTac diet-induced obese mice (Taconic) were maintained on HFD and acclimated
to single housing, handling, and dosing prior to study initiation. Once body weights were stable (2 weeks of acclimation),
animals were dosed with either vehicle (10% Tween in 0.5% methylcellulose) or 10 mg/kg TTA-A2 2 hours prior to lights on
for 2 weeks with daily monitoring of body weights.
Diet-induced obese rats were obtained from Charles River, maintained on HFD, and acclimated to housing, handling, and
dosing prior to study initiation. Study started with 135-day-old rats weighing 607 ± 7.6 g. Animals were dosed by oral
gavage 1 hour prior to the sleep period with vehicle or with 10 or 30 mg/kg TTA-A7 daily for 14 days (n = 8 per group). An
additional cohort of animals was dosed with 3 mg/kg fenfluramine as a positive control in this study. Body composition
was evaluated by DexaScan (QDR 4500A; Hologic) 14 days prior to dosing and again at the end of the study.
METHODS
Statistics. Data are expressed as mean ± SD for in vitro and pharmacokinetic experiments and as mean ± SEM for in vivo
pharmacodynamic studies. Endpoint comparisons with 2 groups of equal size were compared with a paired 2-tailed
Student’s t test (Excel 2003; Microsoft). Where the group sizes differed, significant endpoint differences were determined
using an unpaired 2-tailed Student’s t test (Prism, version 5; GraphPad). For parallel repeated-measures studies, 2-way
ANOVA was used with Bonferroni posthoc evaluations to determine the significance for individual time points (Prism;
GraphPad). Active wake data were analyzed using linear mixedeffect models to account for repeated measures (R for
Windows, version 2.8.1; http://www.r-project.org). A P value less than 0.05 was considered significant for all studies.
HFDiet
Normal chow
Cacna1g KO
Light off
TTA-A2
Lean mice
obese mice
depolarized
hyperpolarized
rat
blocked
Dose dependency
Rat
TTA-A2:open
HFDiet
Normal chow
TTA-A2:open
mice
Diet induced obese mice
Rat
RESULTS
Administration of a potent and selective antagonist
of T-type calcium channels, TTA-A2, to normalweight animals prior to the inactive phase acutely
increased sleep, decreased body core temperature,
and prevented high-fat diet–induced weight gain.
Administration of TTA-A2 to obese rodents reduced
body weight and fat mass while concurrently
increasing lean muscle mass.
These effects likely result from better alignment of
diurnal feeding patterns with daily changes in
circadian physiology and potentially an increased
metabolic rate during the active phase.
CONCLUSION
Together, these studies reveal what we
believe to be a previously unknown role
for T-type calcium channels in the
regulation of sleep and weight
maintenance and suggest the potential
for a novel therapeutic approach to
treating obesity.