Functional Abilities Form - University of Western Ontario
advertisement

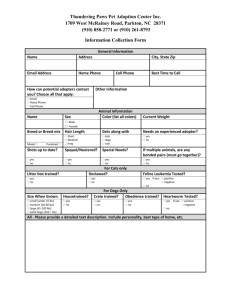
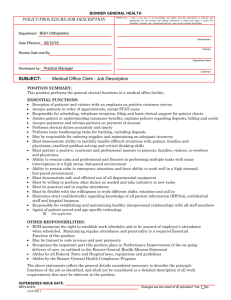
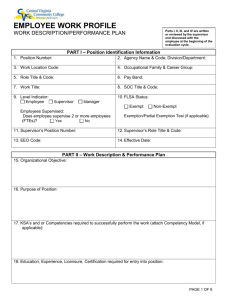
THE UNIVERSITY OF WESTERN ONTARIO Department of Epidemiology and Biostatistics 2003 Francine Lortie-Monette, MD, MSc, CSPQ, MBA Workers’ Compensation in Ontario: Workplace Safety and Insurance Board (WSIB) Roles of Physicians: Prevention Diagnosis Treatment/medical management Facilitating return to work Reporting WSIB/MOLTC Agreement Business continues to be conducted under an agreement that was reached in October 1990 between the WSIB and MOH FILING A CLAIM WITH WSIB Once a claim has been filed, a practitioner who has examined or treated the worker has a duty 1 to promptly disclose health-related information WSIB may need for adjudication purposes. Conversely, there is no legal obligation to release information if the patient does not wish to file a claim. _______ Section 37 (1) of the Workplace and Insurance Act, 1997. 1 FILING A CLAIM WITH WSIB For accidents on or after January 1, 1998, workers must file a claim for compensation: within 6 months from the date of accident or in the case of occupational disease, 6 months from the date at which the worker learns that s/he suffers from the disease. Difficult! incomplete medical information poor communication F.D. frequently misunderstands WSIB/employer/employee role Body Part Evidence for Causal Relationship between physical work factors and musculoskeletal disorders 1 Neck and Neck/Shoulder Repetition, Force, Posture Elbow Force Carpal Tunnel Syndrome Repetition, Force, Vibration Hand/Wrist Tendinitis Repetition, Force, Vibration Back Lifting/forceful movement Heavy physical work Awkward Posture Whole Body Vibration 1 Musculoskeletetal Disorders and Workplace Factors. US Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Institute or Occupational Safety and Health, July 1997. WSIB Statistics-2001(1) Accidents registered = 375,000 Allowed = 74% Abandoned = Denied = Pending = Amalgamated = 16% 3% 6% 1% Need for specific, objective information: objective medical findings treatment plans notification re: precautions (ie?) RANGE OF MOTION TESTING Active and Passive Multiple Directions RETURN-TO-WORK ISSUES Returning a patient to work after an absence due to sickness or injury is an issue that arises almost daily in any busy family practice. One of the main goals for treating an ill or injured individual is to restore the person, as much as possible, to their pre-injury level of function. Recovery is not linear. An experienced physician will have designed a treatment plan from the earliest days of the event, using the patient’s job demands as one of the treatment goals. Prolonged absence from one’s normal roles, including absence from the workplace, may be detrimental to a person’s mental, physical and social well-being. A FEW 1998 STATISTICS FROM WSIB: 725 Claims allowed per day, 37% with time lost from work. The average duration of short-term disability benefits: 57.7 calendar days. Of the 97,000 lost-time claims as of March 31 (1997-1998): 94% were for musculoskeletal injuries (sprain, strain, fractures). Of these: 30% were injuries of the back (including the neck) 24% were injuries of the upper extremities. 18% were injuries of the lower extremities. Benefits paid: $2.2 billions. CONSEQUENCES OF AN ILLNESS OR INJURY The World Health Organization International Classification of Impairments, Disabilities, and Handicaps provide a framework for describing the consequences of an illness or injury: Impairment (an organ-based concept) – any loss or abnormality of psychological, physiological, or anatomical structure or function. Impairment is described according to the body organ or system, e.g. visual impairment (myopia, blindness), musculoskeletal impairment (knee instability, shoulder impingement) or respiratory impairment (loss of FVC or FEV1). Disability (a task-based concept) – any restriction or lack of ability to perform an activity in the manner or within the range considered for a human being. Disability is described according to a specific task, posture, or work environment, e.g. difficulty with floor-to-waist lifting, prolonged sitting, or working in the cold. In the view of the CMA & the OMA: It is not the treating physician's responsibility or role to determine whether the patient’s condition meets the insurer’s definition of disability ie the justification for the patient to be off work especially as the physician is not aware of all jobs available in the workplace “Injury/Illness & Return To Work/Function: A Practical Guide for Physicians” Prepared by the Physician Education Project in Workplace Health in conjunction with the OMA and the WSIB What is the Functional Abilities Form (FAF)? Highlights limitations Optional tool completed at the request of either of the workplace parties Who can complete the Form? This form can only be completed by a health professional who is treating the worker (ie a member of the College of Health Profession as defined in The Regulated Professions Act, 1991) Health professionals do not initiate this form. Functional Abilities Form: The legislation requires physicians and other treating health professionals to complete the Functional Abilities form only if requested to do so by the worker or employer. Some workplaces may prefer to use a form designed for their specific environment. These workplaces are welcome to use their own from to gather functional abilities information but the WSIB does not pay health professionals for completing these variations. NO MEDICAL OR DIAGNOSTIC INFORMATION should be requested or provided WSIB information hotline: 1-800-465-5606 in a workplace-specific functional abilities form. The Functional Abilities Form Employer Requests from the worker a copy of the Form 2647A Worker Having signed consent, brings a copy of it along and a copy of the worker’s consent allowing the health professional to release functional abilities information to the employer. May send a copy of the form and of the consent directly to the health professional. with Form 2647A to the attending health professional. Asks the professional to complete the form. Completes the form, gives the employer the canary Health Professional yellow copy, gives the worker the pink copy and sends the white copy to the WSIB. The white copy also serves as the professional’s invoice for payments. The FAE form may be faxed. Physical Demands Material Handling: Lifting Carrying Pushing Pulling Non-Material Handling: Stand/sit/walk Stoop/kneel/crouch Reaching Fingering Handling Grasp / Pinch Tool Use Physical Demand Characteristics of Work Physical Demand Characteristics of Work (Dictionary of Occupational Tiles, Vol. II, 4th Edition, Revised 1991) PHYSICAL DEMAND LEVEL OCCASIONAL 0-33% OF WORKDAY FREQUENT 34-66% OF WORKDAY CONSTANT 67-100% OF WORKDAY TYPICAL ENERGY EXPENDITURE Sedentary 1-10 lbs. Negligible Negligible 1.5-2.1 METS Light 11-20 lbs. 1-10 lbs. Negligible 2.2-3.5 METS Medium 21-50 lbs. 11-25 lbs. 1-10 lbs. 3.6-6.3 METS Heavy 51-100 lbs. 26-50 lbs. 11-20 lbs. 6.4-7.5 METS Very Heavy Over 100 lbs. Over 50 lbs. Over 20 lbs. Over 7.5 METS Material Handling Characteristics of Work (U.S. Dept. of Labor D.O.T. 1996) Occasional (0 to 33% of the workday) 1 lift/carry every 15 min Frequent (34 to 66% of the workday) 1 rep every 5 min Constant (67 to 100% of the workday) >1 rep every 5 min Non-Material Handling Characteristics of Work Occasional (0 to 33% of the workshift) 1-100 reps over 8hr Frequent (34 to 66% of the workshift) 100-500 reps over 8hr Constant (67 to 100% of the workshift) >500 reps over 8hr Consistency of Effort Testing A combination of tests / no “one indicator” Kinesio-physical Approach Normal expectations ie Push > pull, shoulder height values < bench height abilities Consistency in testing of same variable with different tests Objective physiological responses to activity HR & BP monitoring ++Clinical observations *Static Coefficients of Variation (>50% CV > 15%) *Jamar Grip (Expected Bell Curve* / CV*) Controversial if solely used *Caution-Ref. Shechtman, Journal Hand Therapy, July 2001 Canadian Classification and Dictionary of Occupations Definitions Sedentary Lifting 10 lbs maximum. Occasional lifting and/or carrying. Primarily sitting, with occasional walking or standing. Light Lifting 20 lbs maximum. Frequent lifting and/or carrying up to 10 lbs. May require significant standing or walking. May involve sitting with pushing and pulling of the arms and/or leg controls. Medium Lifting 50 lbs maximum. Frequent lifting and/or carrying up to 20 lbs. May involve sitting with pushing and pulling of the arms and/or leg controls. Heavy Lifting 100 lbs maximum. Frequent lifting and/or carrying up to 50 lbs. Very Heavy Occasional lifting in excess of 100 lbs. Frequent lifting and/or carrying in excess of 50 lbs. OCCUPATIONAL Health Stressors: Work monotony low job control mental stress perception about work lack of flexibility UE Specific Recommendations Ability / force level for sustained grip/pinch or torquing Job & task rotations Comment on frequency of repetitions Comment on high reps with recovery times needed Avoid vibration Limit exposure to cold / intolerance Use of gloves Comments on use of tools (built-up handles) Awkward or sustained postures Graduated RTW schedules The provision of the right health care at the right time. Return to best possible health The prevention of recurrences & of worker impairment ADDITIONAL RESOURCES AVAILABLE IN THE MANAGEMENT OF OCCUPATIONAL INJURIES / DISEASES - continued Regional Evaluation Center (RECs): Regional Evaluation Centers focus on musculoskeletal injuries. They do help clarify the diagnosis, prognosis and therapeutic options as necessary. There are RECs in the following areas: Ottawa, Kingston, Peterborough, Oshawa, Toronto, Hamilton, St. Catharines, Kitchener, London, Windsor, Sudbury, Timmins, Kenora, Sault Ste.Marie, and Thunder Bay. RECs are obligated to schedule appointments within 10 days of receiving the referrals, and must provide a report within 10 days of the examination. ADDITIONAL RESOURCES AVAILABLE IN THE MANAGEMENT OF OCCUPATIONAL INJURIES / DISEASES - continued Specialty Clinics: Injured workers may be referred to Specialty Clinics through The Workplace Safety and Insurance Board (WSIB). These Specialty clinics provide expert assessments in the following areas: Amputations and Burns, Upper Extremities, Neurology (Head Injury or severe neck injury), Prosthetics, Psychotraumatic Disorders, Chronic Pain/Functional Restoration. These clinics were initially centralized in the Toronto-Mississauga hospitals but further decentralization is taking place. Specialized opinions may also be obtained from individual experts in specific disciplines. ADDITIONAL RESOURCES AVAILABLE IN THE MANAGEMENT OF OCCUPATIONAL INJURIES / DISEASES The Occupational Health Clinics for Ontario Workers (Hamilton, Toronto, Windsor and Sudbury): Do specialized assessments, Review the literature as needed, Comment on possible work-relatedness of condition, etc. Contacts (1) Health Professional Access Line 416-344-4526 or Toll Free 1-800-569-7919 Provider Registration Section 200 Front St West, 4th Floor Toronto ON M5V 3J1 Toll Free 1-800-387-0750 Fax 416-344-2955 Contacts (3) Website www.wsib.on.ca For health care professionals http://www.wsib.on.ca/wsib/wsibsite.nfs/Public/HealthProfessionals To download forms http://www.wsib.on.ca/wsib/wsibsite.nfs/public/Forms