+ HCO 3 - Technion moodle
advertisement

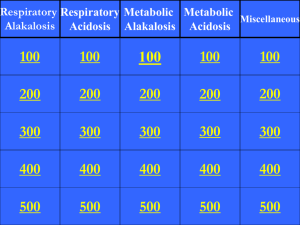
Acid Base Disorders הפרעות בסיס חומצה Karl Skorecki skorecki@tx.technion.ac.il Tel: 8543250 .1 asterisk indicates optional .2 you may contact me as noted above with questions Hey- What’s the peeH here anyway? Definitions and Equations 1. Medical definition of acid-base status of a patient refers to [H+] of the extracellular fluid. 2. Normal [H+]ECF is 40nM/Litre (equivalent to pH 7.40) 3. Acidemia is a state wherein the [H+]ECF > 40 (pH < 7.40) Alkalemia is a state wherein the [H+]ECF < 40 (pH > 7.40) (Euphemia is a state wherein the [H+]ECF is normal). Definitions and Equations (Cont.) 4. H+ + HCO340nM H2O+CO2 40 25mM H+nmol/L=25 40 H2CO3 • PCO2 = 40mmHg PCO2mmHg HCO3mmol/L 25 5. The ratio PCO2/HCO3 determines the [H+] (pH) Acidosis any process which increases PCO2/HCO3- ratio Alkalosis any process which decreases PCO2/HCO3- ratio Definitions and Equations (Cont.) PCO2 H+ = 25 • HCO3 6. Acidosis increases PCO2/HCO3 ratio Metabolic: by lowering HCO3 Respiratory: by raising PCO2 Alkalosis decreases PCO2/HCO3 ratio Metabolic: by raising HCO3 Respiratory: by lowering PCO2 מדינת ישראל הצעת חוק בסיסי החומצה שם החוק :חוק איסור השימוש ב ”Base Excess”-וחוק איסור שימוש בשמות הנדרסון ,הסלבך. הואיל וסטודנטים לרפואה בישראל כבר מספיק מסכנים ומבולבלים והואיל ואין מרצה או פרופסור בעולם שמבינ/ה בעצמו/ה את המונחים הנ"ל הצעת חוק זו באה לאסור לחלוטין את השימוש במונחים הנ"ל בכתב בעל-פה ,במצגת ,בביקור רופאים ,בבית ,בעבודה ,ובכל מקרה (למעט בהצעת החוק הנוכחית) עונש :המפר את החוק לא יוכל לעשות רוטציה בשום מחלקה לנפרולוגיה המכבדת את עצמה ,ויחוייב ללמוד את נושא בסיסי החומצה אך ורק במסגרת המחלקות הכירורגיות. נערך ונחתם היום ע"י השר לענייני בסיסי חומצה * Definitions and Equations (Cont.) PCO2 H+ = 25 • HCO3 7. The four primary acid-base disturbances are: Metabolic acidosis (primary decrease in HCO3) Metabolic alkalosis (primary increase in HCO3) Respiratory acidosis (primary increase in PCO2) Respiratory alkalosis (primary decrease in PCO2) 8. - Can have none, one, two, or three of the above in combination. - Can have any combination except? - The net result can leave [H+] normal/high (acidemia) or low (alkalemia) Metabolic Acidosis 15 year-old with three week history of polyuria, polydipsia and 2 day history of nausea, abdominal pain, and weakness progressing to extreme drowsiness. Physical exam remarkable for rapid breathing, low blood pressure, and decreased level of consciousness. Lab: Glucose [H+] PCO2 HCO3 Na+ K+ Cl- 220 62.5 (pH 7.2) 25 10 142 3.4 105 Metabolic Acidosis (Cont.) PCO2 H+ = 25 • HCO3 62.5 25 10 BUT: HCO3 is low PCO2 is also low [H+] is high (low pH; patient is acidemic) • Metabolic acidosis primary decrease in HCO3 • Maybe the patient has a metabolic acidosis • What about the PCO2 ? “Compensation” Rules • Each primary acid base disturbance is associated with an expected compensation • If the primary disturbance is metabolic (HCO3), the expected compensation is respiratory (PCO2) • If the primary disturbance is respiratory (PCO2), the expected compensation is metabolic (HCO3) • The compensation “tries” to restore the H+ (pH) toward normal, but never quite makes it (why ? see later) • The “expected” amount of compensation is different for each of the four primary acid-base disturbances and needs to be memorized • The direction of the expected compensation is always in the same direction as the primary disturbance Metabolic Acidosis PCO 2 + H = 25 • HCO 3 compensation primary Metabolic Alkalosis PCO 2 + H = 25 • HCO 3 compensation primary Respiratory Acidosis PCO 2 + H = 25 • HCO 3 primary compensation Respiratory Alkalosis PCO 2 + H = 25 • HCO 3 primary compensation 15 year-old with diabetic coma H+ 62.5 (pH 7.2), PCO2 25, HCO3 10 PCO2 H+ = 25 • HCO3 62.5 25 10 If primary metabolic acidosis, does the decrease in PCO2 represent an “appropriate” expected compensation ? Metabolic acidosis: Rule: for every decrease of 1 mmol/Litre in HCO3 there should be a decrease of 1 mmHg PCO2 Did this happen ? PCO2 H+ = 25 • HCO3 62.5 25 pH = 7.2 10 HCO3 25 - 10 = 15 PCO2 40 - 25 = 15 Therefore: Respiratory compensation is appropriate * If respiratory compensation is appropriate, WHY is the patient still acidemic (p = 7.2) ? After all, most people could hyper-ventilate further, even down to PCO2 of < 10 Answer: * The capacity for “respiratory compensation” is what makes the bicarbonate buffer system so useful, even though the pK for H2CO3 is 6.8 (far from 7.4) CO2 HCO3- PCO2 H+ = 25 • HCO3 62.5 25 pH = 7.2 10 Perfectly compensated metabolic acidosis What if PCO2 remained “normal” ? PCO2 H+ = 25 • HCO3 40 H+ = 100 pH = 7.00 10 Metabolic acidosis + respiratory acidosis clinical example ? What if PCO2 fell to 16 ? PCO2 H+ = 25 • HCO3 16 H+ = 40 pH = 7.4 10 Metabolic acidosis + respiratory alkalosis clinical example ? Extracellular pH looks good, but patient is very sick Steps in Assessment of Metabolic Acidosis Step 1: Is metabolic acidosis present ? HCO3 low and PCO2 low (also occurs in respiratory alkalosis) But patient acidemic Step 2: Is the respiratory compensation… as expected (PCO2: HCO3 = 1:1) too much (PCO2: HCO3 > 1:1) (then also respiratory alkalosis) too little (PCO2: HCO3 < 1:1) (then also respiratory acidosis) Step 3: Differential diagnosis “anion gap” Metabolic Acidosis 15 year-old with diabetic coma and metabolic acidosis H+ 62.5 PCO2 25 HCO3 10 Na+ 142 K+ 3.4 Cl105 Anion Gap = [Na+] - ([Cl-] + [HCO3-]) = 142 - (105 +10) = 27 So what ? Differential Diagnosis of Metabolic Acidosis “anion gap” • Metabolic acidosis results from decrease in HCO3• There are two ways whereby HCO3(a) titration of HCO3- by an acid e.g. H+Ac + Na+HCO3- NaAc + H2O + CO2 (b) loss of NaHCO3 in urine or stool • Process (a) and process (b) leave different “imprints” in the plasma chemistries Process A titration of HCO3- by an acid H+X- + NaHCO3- NaX + H2O + CO2 • Designate Na+, Cl-, and HCO3- as electrolytes whose concentrations we chose to measure • Normally: Na+ - (Cl- + HCO3-) = “anion gap” 140 - (103 + 25) = 12 • Process A: We do not routinely measure X(we don’t know what it is at the beginning) • Therefore, for every “X-” gained, there is one “HCO3-” lost • Therefore, “anion gap” will rise by one for every HCO3 titrated away Metabolic Acidosis 15 year-old with diabetic coma and metabolic acidosis H+ 62.5 PCO2 25 HCO3 10 Na+ 142 K+ 3.4 Cl105 Anion Gap = 27 Normal anion gap is 12 anion Gap is 27 - 12 = 15 HCO3- has decreased by 40 - 25 = 15 Gap = HCO3Therefore: anion gap type metabolic acidosis Anion Gap Metabolic Acidosis Only 4 categories: Ketoacidosis Lactic - Diabetic - Alcoholic - Starvation - Type A (ischemia, anoxia) - Type B (metabolic) Uremic Poisons - Methanol - Ethylene glycol - Salicylic acid - Other Metabolic Acidosis 15 year-old with diabetes, coma and extensive vomiting H+ 62.5 (pH 7.2) PCO2 25 HCO3 10 Na+ 142 K+ 3.4 Cl95 Anion Gap = 142 - (95 + 10) = 37 Gap 37 - 12 = 25 HCO3- = 15 How can that be ? Answer: • Occult metabolic alkalosis • If no metabolic acidosis, HCO3 would have been 35 • Metabolic acidosis is much more severe than reflected in HCO3 of 10 (35 10 Vs. 25 10) • Consistent with vomiting • More on metabolic alkalosis and vomiting after lunch Metabolic Acidosis Anion Gap • Ketoacidosis • Lactic • Uremic • Poison Non-Anion Gap • Rare: HCl poisoning • Primary loss of HCO3renal - complicated external (diarrhea, uretero-sigmoidostomy) 42 year-old presents with a 5-day history of severe watery diarrhea beginning 10 days after completing antibiotics for pyelonephritis H+ 62.5 (pH 7.2) PCO2 25 HCO3 10 Na+ 140 K+ 3.4 Cl118 Anion gap 140 - (118 + 10) = 12 * Why doesn’t the anion gap rise in a non-anion gap acidosis? Anion gap = Na+ - (Cl- + HCO3-) By definition, the HCO3- has decreased. Therefore, if the anion gap hasn’t changed: • Either the Na+ has decreased • Or, the Cl- has increased Answer: The Cl- rises (hyperchloremic metabolic acidosis) * How does the Cl- know to increase ? Anion gap = Na+ - (Cl- + HCO3-) In a non-anion gap metabolic acidosis there is either: Gain of HCl (rare HCl poisoning) • So each HCO3- lost is accompanied by a Cl- gained • Therefore no change in anion gap Primary loss of Na+ with HCO3• So each HCO3- lost is accompanied by a Na+ lost • If the Na+ really decreased 1:1 with the HCO3-, then the anion gap wouldn’t change • But, that doesn’t happen (the body defends its volume and osmolality and hates hypo Na+) • Therefore, the kidney reabsorbs Na+ with Cland the Cl- increases Non Anion Gap (Hyperchloremic) Metabolic Acidosis • HCl gain • HCO3- loss Extraneal Renal Diarrhea Uretero-sigmoidostomy Renal Acidosis Renal Vein Na+HCO3- 5,070mmol/day Kidney’s Job: 1) Reclaim all of filtered HCO32) Generate new HCO3corresponding to HCO3- lost with dietary acid 3) Each new HCO3generated corresponds to NH4+ excreted Na+HCO35,000mmol/day Renal Artery NH4+ Zero HCO3- Renal Tubular Acidosis Proximal • Failure to reclaim HCO34,000 HCO35,000 4,000 genesis • bicarbonaturia • urine pH > 7 Distal • Failure to excrete H+(NH4+) and hence generate HCO3- HCO34,000 steady-state • no bicarbonaturia • urine pH < 6 Metabolic Acidosis 70 year-old with glaucoma treated with acetazolamide (carbonic anhydrase inhibitor) presents with weakness. Physical examination: BP 100/50 (baseline 150/90) H+ 75 (pH 7.12) PCO2 45 HCO3 15 Na+ 139 K+ 2.1 Cl108 Anion gap 12 Urine pH 8 • Bicarbonate low, patient very acidemic • Respiratory compensation respiratory acidosis • Anion gap normal Diagnosis: acetazolamide proximal RTA Hypokalemia respiratory muscle weakness Mixed Anion Gap + Non Anion Gap Metabolic Acidosis 70 year-old with glaucoma treated with acetazolamide (carbonic anhydrase inhibitor) presents with fever, severe abdominal pain (RUQ), jaundice and collapses. BP 60 systolic extremities; breathing: distressed. Lab: WBC 24,000 92% neutrophils H+ 100 (pH 7.00) PCO2 20 HCO3 5 Na+ 140 Cl113 Anion gap 22 Urine pH 8 Acid-base diagnosis: Likely scenario: An anion gap metabolic acidosis can turn into a non-anion gap metabolic acidosis HOW ? If the anion accumulated in the plasma is excreted in the urine Example: 15 year-old DKA treated with saline (isotonic NaCl) initial: H+ 62.5 (pH 7.2; glucose 220) PCO2 25 HCO3 10 Na+ 142 Cl103 Anion gap 27 gap = 15 HCO3 = 15 Post Rx: H+ 62.5 (pH 7.2) PCO2 25 HCO3 10 Na+ 138 Cl110 Anion gap 18 gap = 6 HCO3 = 15 Where have all the extra unmeasured anions gone ? Answer: Pissed away as a result of saline volume expansion Hint: Can measure gap in urine The “Normal” or “Baseline” Anion Gap * “unmeasured” 6 K++Ca2++Mg2+ gap “measured” 140 albumin phosphate sulfate HCO3 Na+ ClALL CATIONS = “unmeasured” 18 “measured” 128 ALL ANIONS Gap: Measured Cations (Na+) - Measured Anions (Cl- + HCO3-) Equals Unmeasured Anions - Unmeasured Cations Example: Hypoalbuminemia lowers the baseline anion gap Metabolic Acidosis • Look at [H+] (pH) HCO3PCO2 PCO2 + H = 25 • HCO 3 • [H+] high (pH low) metabolic acidosis HCO3- low • Look at PCO2 to assess respiratory compensation • Calculate anion gap • Compare anion gap to bicarbonate * 1. 2. 3. pH [H+] – not really necessary Table on PALM Between 7.25 7.50 for every deviation of one pH unit from 7.40, the [H+] deviates correspondingly by 1mmol/litre in the opposite direction Rule of 80% 7.00 100 7.10 80 7.20 8 X 80 = 64 7.30 8 X 64 = 51 7.40 8 X 50 = 40 7.50 8 X 40 = 32 7.60 8 X 32 = 26 7.70 8 X 26 = 21 * H+ (mMol/Litre) pH . . . . . . . . . . . . . . . Table [H+] pH * Causes of Metabolic Acidosis Inability to excrete the dietary H+ load A. Diminished NH4+ production 1. Renal failure 2. Hypoaldosteronism (type 4 renal tubular acidosis) B. Diminished H+ secretion 1. Type 1 (distal) renal tubular acidosis Increased H+ load or HCO3- loss A. Lactic acidosis B. Ketoacidosis C. Ingestions 1. Salicylates 5. Sulfur 2. Methanol or formaldehyde 6. Toluene 3. Ethylene glycol 7. Ammonium chloride 4. Paraldehyde 8. Hyperalimentation fluids D. Massive rhabdomyolysis E. Gastrointestinal HCO3- loss 1. Diarrhea 3. Ureterosigmoidostory 2. Pancreatic, billiary or intestinal fistulas 4. Cholestyramine F. Renal HCO3- loss type 2 (proximal) renal tubular acidosis Most common causes shown in purple Anion Gap in Major Causes of Metabolic Acidosis * High anion gap A. Lactic acidosis: lactate, D-lactate B. Ketoacidosis: -hydroxybutyrate C. Renal failure: sulfate, phosphate, urate, hippurate D. Ingestions 1. Salicylate: ketones, lactate, salicylate 2. Methanol or formaldehyde: formate 3. Ethylene glycol: glycolate, oxalate E. 4. Paraldehyde: organic anions 5. Toluene: hippurate (usually presents with anion gap) 6. Sulfur: SO42Massive rhabdomyolysis The substances after the colon represent the major retained anions in the high anion gap acidosis * Anion Gap in Major Causes of Metabolic Acidosis (cont.) Normal anion gap (hyperchloremic acidosis) Gastrointestinal loss of HCO31. Diarrhea Renal loss of HCO31. Type 2 (proximal) renal tubular acidosis C. Renal dysfunction 1. Some cases of renal failure 2. Hypoaldosteronism (type 4 renal tubular acidosis) 3. Type 1 (distal) renal tubular acidosis Ingestions: 1. Ammonium chloride 2. Hyperalimentation fluids E. Some cases of ketoacidosis, particularly during treatment with insulin Respiratory Acidosis PCO 2 + H = 25 • HCO 3 • Primary increase in PCO2 (hypoventilation) • Compensatory increase in HCO3 (metabolic) • In metabolic acidosis the compensation is respiratory and occurs instantly • In respiratory acidosis the compensation is metabolic and it takes time and can be divided into acute/chronic • The combination of increased PCO2 and increased HCO3can also be seen in metabolic alkalosis with respiratory compensation, but don’t be fooled because… Metabolic Compensation for Respiratory Acidosis Primary PCO2 Compensation HCO3- Acute 10mmHg 1mmol/L Chronic 10mmHg 3mmol/L (memorize) Mechanisms of Metabolic Response Enhanced HCO3 reclamation H+ Na+ H+ PCO2 Causes of Respiratory Acidosis (Hypoventilation) Brain Airway Chest wall + diaphragm Lungs * Causes of Acute and Chronic Respiratory Acidosis Inhibition of the medullary respiratory center A. Acute 1. Drugs: opiates, anesthetics, sedatives 2. Oxygen in chronic hypercapnia 3. Cardiac arrest 4. Central sleep apena B. Chronic 1. Extreme obesity (Pickwickian syndrome) 2. Central nervous system lesions (rare) 3. Metabolic alkalosis (although hypercapnia is an appropriate response to the rise in pH in this setting) * Causes of Acute and Chronic Respiratory Acidosis (cont.) Disorders of the respiratory muscles and chest wall A. Acute 1. Muscle weakness: crisis in myasthenia gravis, periodic paralysis, aminoglycosides, Guillain-Barré syndrome, severe hypokalemia or hypophosphatremia B. Chronic 1. Muscle weakness: spinal cord injury, poliomyelitis, amyotrophic lateral sclerosis, multiple sclerosis, myxedema 2. Kyphoscoliosis 3. Extreme obesity Upper airway obstruction A. Acute 1. Aspiration of foreign body or vomitus 2. Obstructive sleep apena 3. Laryngoispasm * Causes of Acute and Chronic Respiratory Acidosis (cont.) Disorders affecting gas exchange across the pulmonary capillary A. Acute 1. Exacerbation of underlying lung disease (including Increased CO2 production with high-carbohydrate diet) 2. Adult respiratory distress syndrome 3. Acute cardiogenic pulmonary edema 4. Severe asthma or pneumonia 5. Pneumothorax or hemothorax B. Chronic 1. Chronic obstructive pulmonary disease: bronchitis, emphysema 2. Extreme obesity Mechanical ventilation 28 year-old brought into ER because of found stuporous on the floor at home with an empty bottle of diazepam and a suicide note. Previously healthy. Physical examination: stuporous, but otherwise unremarkable. Lab: H+ 60 (pH 7.22) PCO2 68 HCO3 28 PO2 80 • Patient acidemic with elevated PCO2 and HCO3 must at least have respiratory acidosis • Compensation PCO2 28 appropriate for acute HCO3 3 respiratory acidosis • • • • • • 28 year-old overdose has been lying on the floor for two days. Physical examination reveals extensive edema on the right side of the body. No urine in bladder Lab: H+ 100 (pH 7.00) PCO2 68 HCO3 17 Na+ 138 gap: 138 - (98+17) = 23 Cl98 + K 5.6 Creat 4.8 CK 68,000 I.U. Patient very acidemic, with high PCO2 and low HCO3Combined respiratory and metabolic acidosis Respiratory acidosis from drug overdose Expected compensation: HCO3- 28, but in reality: HCO3- 17 HCO3 11 Anion gap 23: gap = 11 Anion gap metabolic acidosis: rhabdomyalysis + renal failure 62 year-old with stable COPD Lab: H+ 50 (pH 7.3) PCO2 60 HCO3 30 PO2 60 • Patient acidemic with elevated PCO2 elevated bicarbonate • Chronic respiratory acidosis • Expected compensation: PCO2 20 HCO3 6 62 year-old with stable COPD and 1-day history of worsening cough, fever and dyspnea with drowsiness Lab: H+ 60 (pH 7.22) PCO2 80 HCO3 33 PO2 45 • Acute worsening of respiratory acidosis • Expected compensation: Chronic as before HCO3 to ~31 Acute further smaller HCO3 to ~33 • What is the most dangerous intervention, and if you make this mistake, what should you do ? 62 year-old with COPD and acute worsening reaches respiratory failure and is ventilated. ABG’s measured immediately after Lab: H+ 30 (pH 7.5) PCO2 40 HCO3 33 PO2 380 • What happened ? • How will this affect weaning from ventilator ? • What will her ABG’s look like if she extubates herself ? 62 year-old with COPD and respiratory failure on ventilator is treated with antibiotics and develops severe watery diarrhea Lab: H+ 62.5 (pH 7.2) PCO2 50 HCO3 20 Na+ 142 (gap 12) Cl- 110 • Respiratory acidosis appropriately ventilated to PCO2 50 • Expected HCO3- is 25 + 3 = 28 Observed HCO3- is 20 Therefore: Metabolic acidosis 28 20 • Anion gap not elevated: antibiotic induced diarrhea Respiratory Alkalosis PCO 2 + H = 25 • HCO 3 • Primary decrease in PCO2 (hyperventilation) • Compensatory decrease in HCO3 (metabolic) • The metabolic compensation can be divided into acute (minutes) and chronic (hours to days) • The compensation for chronic respiratory alkalosis is the most complete, and nearly normalizes the pH • The combination of low PCO2 and HCO3 was also seen in metabolic acidosis, but don’t be fooled, because… Metabolic Compensation for Respiratory Alkalosis Primary PCO2 Compensation HCO3- Acute 10mmHg 2mmol/L Chronic 10mmHg 5mmol/L (memorize) Mechanism for Metabolic Compensation • Low PCO2 in proximal tubule • Inhibition of Na+-H+ exchanger • Decreased proximal reabsorption of filtered HCO3• Bicarbonaturia It’s always easier to lose something then to win something – that’s why this compensation is so complete * Causes of Respiratory Alkalosis Hypoxemia A. Pulmonary disease: pneumonia, interstitial fibrosis emboli, edema B. Congestive heart failure C. Hypotension or severe anemia D. High-altitude residence Pulmonary disease Direct stimulation of the medullary respiratory center A. Psychogenic or voluntary hyperventilation B. Hepatic failure C. Gram-negative septicemia D. Salicylate intoxication E. Postcorrection of metabolic acidosis F. Pregnancy and the lutheal phase of the menstrual cycle (due to progesterone) G. Neurologic disorders: cerebrovascular accidents, pontine tumors Mechanical ventilation 58 year-old hypertensive man presents to ER with abrupt loss of consciousness and paralysis. Pex: hypertension, rapid breathing (hyperpnea), unresponsive, pinpoint pupils. CT reveales pontine hemorrhage After one week in hospital: H+ 37 (pH 7.43) PCO2 30 HCO3 20 • Patient mildly alkalemic with low PCO2 and low HCO3, therefore: respiratory alkalosis • Compensation PCO2 10 HCO3 5 perfect compensation 58 year-old man from previous slide has a bladder catheter and develops fever and WBC’s noted in urine Repeat ABG’s H+ 28 (pH 7.52) PCO2 20 HCO3 18 • Patient more alkalemic with further fall in PCO2 by additional 10 and compensating further fall in HCO3 by additional 2 • Acute on chronic respiratory alkalosis 58 year-old man from previous slide now develops hypotension and shock Repeat ABG’s and chemistry H+ 50 (pH 7.30) PCO2 20 HCO3 10 Na+ 140 Cl110 20 ( 8) • L-lactate 8mmol/L • Superimposed anion gap metabolic acidosis from septic shock lactic acidosis • What if not aware of prior history and no prior ABG’s and given these values for the first time H+ 50 (pH 7.30) PCO2 20 HCO3 10 Na+ 140 Cl110 20 • Patient acidemic with low bicarbonate metabolic acidosis • Expected PCO2 25 Observed PCO2 20 Therefore respiratory alkalosis • Anion gap 20 gap 8 Anion gap metabolic acidosis • But HCO3 15 > gap 8 • Therefore: non anion gap metabolic acidosis or compensation for respiratory alkalosis 58 year-old man from previous slide experiences cardiopulmonary arrest. After some initial confusion he is intubated and ventilated. Repeat lab tests H+ 100 (pH 7.00) PCO2 40 HCO3 10 Na+ 140 (gap 20) Cl110 • Why has pH dropped ? • Essentially behaving as uncompensated metabolic acidosis Anion gap component: sepsis and lactate Non-anion gap component: “post compensation for respiratory acidosis” 58 year-old man from previous slide with pontine hemorrhage, septic shock and ventilated, is given 3 ampules of NaHCO3 for acidemia Repeat values H+ 40 (pH 7.40) PCO2 40 HCO3 25 Na+ 150 Cl100 Anion gap 25 • pH, PCO2 and HCO3 are normal • Is there an acid-base disturbance ? • Was it right to give this much bicarbonate ? • What would have been the right treatment ? Metabolic Alkalosis Probably the worst thing to have and most complicated to understand PCO 2 + H = 25 • HCO 3 • Primary increase in HCO3• Compensatory increase in PCO2 Compensation • Not very consistent or reliable • Approximately: for every 1 HCO3 0.7 PCO2 • What limits this compensation and how could you prove it? Pathogenesis • Complicated and variable • Two major categories: Boring Interesting Boring Bicarbonate load to someone with no kidneys converse: if renal function is normal, the presence of metabolic alkalosis severe (interesting) homeostatic disturbance Pathogenesis of Interesting Metabolic Acidosis • “Contraction” around HCO3- space • KCl depletion states Volume expansion • mineralo corticoid excess Volume contraction • GI loss - vomiting - GI suction - chloridorrhea (rare) • Diuretics - loop - thiazide “Contraction” Around HCO3 Space Normal 70Kg TBW 42L ECF 14L [HCO3] HCO3 ICF 28L 25mmol/L 350 10mmol/L 280 Total: 630 “Contraction” Around HCO3 Space Heart failure: ECF expansion ECF 14 22L [HCO3-] 25 Total 500 Treat with diuretics to ECF ECF 15 15 Litres [HCO3-] 37 550/15 = Shrink 7L More to it! • Diuretics also remove K+ with Cl- • Where does the K+ come from ? • Total body K+ ICF ECF [150] X 28 4,200meq 4 X 14 56meq • Patient on diuretic usually has a 300-800mmol K+ deficit Key Role of K+Cl- Depletion in Metabolic Alkalosis ICF K+ AnionECF Na+ K+ lost from ICF Cl- lost from ECF Cl- H+ + K+ HCO3 Anion- H2O + CO2 K+ lost in urine with Cl Gain of intracellular H+ (intracellular acidosis) Gain of extracellular HCO3(metabolic alkalosis) No in total body buffer H2O + CO2 H2CO3 H+ + HCO3- Why do we care about acid-base disturbances ? Clue to underlying disease But are they bad in their own right ? Answer: YES ! WHY ? Main Reason: Metabolic acidosis Respiratory acidosis Metabolic alkalosis Intracellular acidosis - Intracellular Acidosis H+ buffered in Histidines - H+ histidine • Met acidosis • Resp acidosis • met alkalosis Intracellular protein function-conformation Changed conformation and function Summary of Diuretic-Induced Metabolic Alkalosis 1. Contraction 2. K+ depletion 3. Cl- depletion 4. Mineralocorticoid secondary to volume depletion Two Most Common Causes of Metabolic Alkalosis (with hypokalemia) 1. Diuretics (loop, thiazide) 2. Vomiting (GI suction) * Key Ion transport Protein in the Nephron * Principal Cell * Transport of Na+ in the Principal Cell of the Cortical Collecting Duct * Secretion of H+ in the Intercalated Cell of the Cortical Collecting Duct * Secretion of HCO3- in the Intercalated Cell of the Cortical Collecting Duct Key Ion transport Proteins Relevant to Metabolic Alkalosis Luminal fluid * Cl HCO3 Cl + HCO - 3 - Reabsorbed proximally due to: Volume AII Aldo Na+ 1. Negative potential 2. Low Cl3. High K+ favours H+secrection H+ATPase H+-K+ATPase paradoxical acid urine Cl--HCO3- exchanger * Renal ion transport Derangements and Metabolic Alkalosis 45 year-old male smoker repeats reports one week of intractable profuse vomiting H+ 31 (pH 7.49) PCO2 55 HCO3 45 PO2 68 PCO2 and HCO3- • Metabolic alkalosis with respiratory compensation • Respiratory acidosis with metabolic compensation Two ways to figure out: 1. Calculate A-a O2 gradient = PIO2 – 1.25PCO2 – PaO2 = 150 – 69 – 68 = 13 Normal: lung disease not sufficient to cause chronic respiratory acidosis 2. Treat presumed metabolic alkalosis and expect PCO2 to normalize (and PO2 to rise) Pathogenesis of Metabolic Alkalosis • Diuretics • Vomiting (or NG suction) Vomiting Normal H+ ClNaCl + H2O + CO2 Na+ HCO3Na+ HCO3 H+ Cl- Na+ HCO3- to kidney Pathogenesis of Metabolic Alkalosis and Hypokalemia of GI Origin 1. 2. 3. 4. HCl- loss accompanied by NaHCO3 gain Excess of NaHCO3 excreted in urine Equivalent to NaCl (volume) depletion Hypovolemic stimulus to Na+ reabsorption and aldosterone secretion 5. No Cl- to accompany Na+ 6. Na+ reabsorption accompanied by urinary excretion of H+ and K+ Urine Electrolytes in Vomiting Time Na+ K+ Cl- HCO3 Days 1-3 > 6.8 Late < 5.5 • Low urine chloride is key • K+ loss in vomiting is urinary pH * Causes of Metabolic Alkalosis Loss of hydrogen A. Gastrointestinal loss 1. Removal of gastric secretions - vomiting or nasogastric suction 2. Antacid therapy, particularly with cation-exchange resin 3. Chloride-losing diarrhea B. Renal Loss 1. Loop or thiazide-type diuretics 2. Mineralocorticoid excess 3. Postchronic hypercapnia 4. Low chloride intake 5. High-dose carbenicillin or other penicillin derivative 6. Hypercalcemia, including the milk-alkali syndrome C. H+ movement into cells 1. Hypokalemia 2. Refeeding (?) Most common causes shown in blue * Causes of Metabolic Alkalosis (Cont.) Retention of bicarbonate A. Massive blood transfusion B. Administration of NaHACO3 C. Milk-alkali syndrome Contraction alkalosis A. Loop or thiazide-type diuretics B. Gastric losses in patients with achlorhydia C. Sweat losses in cystic fibrosis * A 63 year old man with a 15 year history of chronic obstructive lung disease developed ankle edema one year prior to admission and therapy was instituted with salt restriction, digoxin and furosemide. He complained of increasing weakness and drowsiness and was admitted for evaluation. On admission, the patient was slightly drowsy, cyanotic and in mild respiratory distress. The chest demonstrated the findings of chronic bronchitis and emphysema. There was no ankle edema and periods of bigeminal rhythm were confirmed by ECG. pH Pco2 Po2 HCO3 7.43 (H+ 37) 70 mm Hg 50 46 mmol/L Urine: Sodium Potassium Chloride 2 mmol/L 30 1 Sodium140 mmol/L Potassium 2.5 Chloride 74 Acid – Base Diagnoses? Relation to potassium? Urine electrolytes? * The patient’s diuretic was discontinued, he was given supplemental KCl by mouth, and within four days his rhythm and ECG had normalized, and he felt stronger and more alert. Repeat evaluation showed: pH Pco2 Po2 HCO3 7.32 65 mm Hg 60 33 mmol/L Sodium Potassium Chloride 140 mmol/L 4.4 100 Is he better or worse now with the lower pH? What treatment helped him? Match Clinical Histories with Lab Results 1. 2. 3. 4. 5. H+ 66 52 56 32 31 pH 7.18 7.29 7.25 7.48 7.49 PCO2 40 60 27 46 20 HCO3 15 29 12 36 16 ___ Other________ gap 12, K+ 2.0 gap 24, L-lactate 1 PK+ 1.9, UCl- 2 gap 21 a. 30 year old with Crohn’s disease and intestinal blind loop resumes enteral intake b. 58 year old, dyspnea and hypotension after long air travel c. 21 year old woman, BMI 19, amenorrhea, weakness d. 28 year old status asthmaticus requiring intubation and sedation e. 70 year old started one month ago on a new tablet to treat glaucoma pHank You! * Bon Apetit!