Legal and Ethical Issues in Medicines Information
advertisement

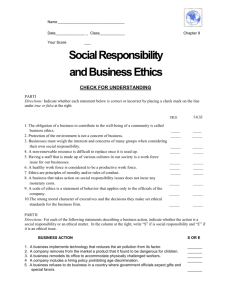
Legal and Ethical Issues in Medicines Information Maggie Fitzgerald Medicines Information Pharmacist 8th January 2008 Acknowledgements: Richard O’Neill; Advancing the Provision of Pharmacy Law and Ethics Teaching - APPLET (Nottingham University) Session aim Identify legal and ethical problems that may be encountered when providing medicines information. Plan Medical Heath Law & ethics Legal aspects Professional codes Ethics Legal aspects DEFINITIONS – Statutory law – Common (case) law – Public law and Private law – Criminal law and Civil law The concept of medical (health care) law A branch of law. Healthcare professionals (including institutes) and patients. Covers a lot of areas of law: tort, criminal, public and administrative law, and family law. Ethical issues are involved in all the problems that arise in medical law. Professional Negligence Negligence “We must take reasonable care to avoid acts and omissions which you can reasonably foresee would be likely to injure your neighbour ...” Lord Atkin in Donoghue v Stevenson (1932) Professional Negligence Requirements for proving negligence: – Duty – Breach – Causation Professional Negligence English Law The duty of a health care professional is to exercise reasonable care and skill. – What is reasonable? Bolam v Friern Hospital Committee 1957 “A person is not negligent if they acted in accordance with accepted practice at the time as decided by a responsible body of competent professional opinion.” Professional Negligence Gross negligence. Criminal prosecution. Prosecution must prove (beyond reasonable doubt) – Existence of duty – Breach of duty causing death – Gross negligence to justify a criminal conviction Data Protection Act 1998 DPA 1998 effective from March 2000. Provides a framework that governs the processing of personal data of the living. Seeks to strengthen the individual’s right to privacy in terms of data processing by applying 8 principles. Data Protection Act 1998 • • • • • • • • 1. Personal data shall be processed fairly and lawfully 2. Personal data shall be obtained for one or more specified lawful purposes and not further processed 3. Personal data shall be adequate, relevant and not excessive 4. Personal data shall be accurate and kept up to date 5. Personal data shall not be kept for longer than is necessary for that purpose 6. Personal data shall be processed in accordance with the rights of data subjects under this Act 7. Measures shall be taken against unauthorised or unlawful processing of personal data and against accidental loss or damage 8. Personal data shall not be transferred out of the European Economic Area Freedom of Information Act 2000 The Act gives right to access information held by public bodies including the NHS If patients wish to obtain information about themselves then the DPA 1998 applies. If the information is not about them but about a public authority then the FOI applies. Copyright Changes in NHS licence centrally negotiated NHS copyright agreement with CLA www.cla.co.uk What’s allowed Staying legal Outcomes of breaching Confidentiality Professional obligation – moral duty – Hippocratic oath • Whatever I see or hear, professionally or privately, which ought not to be divulged, I will keep secret and tell no one. – Geneva Declaration • I WILL RESPECT the secrets which are confided in me, even after the patient has died – Professional guidelines • Codes of Ethics & Practice Human Rights Act 1998 Establishes the right to respect for private and family life. Underscores the duty to protect the privacy of individuals and preserve the confidentiality of their health records. Information information confidential in nature information imparted in circumstances that impose/confer obligation on confident to respect confidentiality Breach of confidentiality Justifications: – Statutory requirements patient threatens harm to self patient threatens harm to others when required by law: – communicable disease – occupational diseases – suspected abuse Confidentiality in the NHS Ethics & Guidelines Statutes relating to patient information in health records professional ethical codes professional guidelines NHS guidelines contract of employment Caldicott Guardians Data Protection Act 1998 Access to Medical Reports 1988 Access to Health records Act 1990 Access to Personal Files Act 1987 Caldicott Principles – Principle 1 - Justify the purpose(s) for using confidential information – Principle 2 - Only use it when absolutely necessary – Principle 3 - Use the minimum that is required – Principle 4 - Access should be on a strict need-to-know basis – Principle 5 - Everyone must understand his or her responsibilities – Principle 6 - Understand and comply with the law Confidentiality breach in the NHS Possible consequences • complaint to the Information Commissioner for breach of the Data Protection Act 1998 • professional disciplinary proceedings (misconduct) • employer disciplinary proceeding (breach of contract of employment) • civil court action - breach of confidence • criminal court action where breach of statute Case Study: Confidentiality You’re in MI and have completed an enquiry due for 5.30pm. It’s now 5.25pm and the caller really wanted the answer by the end of the day. You call the enquirer on their landline and get voicemail. It’s the only contact number you have for them. Their answer phone activates. Gillick Competence - Consent Special cases – children • with capacity– obligation of confidence • without capacity– law requires ‘best interests’ approach Case Study: Consent A patient doesn’t speak English and is receiving chemotherapy at the hospital. Her family translate to her what the hospital staff say. You tell the family that this particular chemo can cause hair loss as a side effect. The family decide not to tell the patient this since they know it will upset her. The patient has to sign the consent form for chemo. Professional codes DEFINITIONS – Accountability – Character traits – Ethical code – Professional etiquette – Responsibility Code of ethics Codes of Ethics Professional responsibilities • duties and obligations Professional relationships • professional behaviour • good communication Accountability Guidance • General – Medicines, Ethics and Practice Guide: a guide for pharmacists • Act in the interest of patients and other members of the public • Ensure knowledge, skills and practice are up to date • Demonstrate integrity and probity, adhere to accepted standards of conduct and do not bring the profession into disrepute • Specific – UKMi Guidance • Police, media, third party, legal proceedings….. Ethics DEFINITIONS – Values – Morals – Ethics – Ethical dilemma THE CONCEPT OF ETHICS – ‘ethics’ is derived from the Greek term ethos, which means customs, habitual usage, conduct, and character Common ethical (moral) theories Teleology - actions are ‘right’ or ‘wrong’ according to the balance of their good or bad consequences Utilitarianism is a teleological theory that judges acts based on their utility or usefulness Deontology - actions are performed out of duty or moral obligation; every person is an end and not solely a means to another person’s end. Virtue theory - places value on the moral character of the actor rather than acts or outcomes of acts Consequentialism – considers the consequence of the action with a view to doing the greatest good for the greatest number. Bioethical principles Four Major Bioethical Principles in Healthcare The Principle of Autonomy The Principle of Non-Malficence The Principle of Beneficence The Principle of Justice The Principle of Autonomy Principle of self-rule right to participate in and decide on a course of action; freedom to act independently competent adult’s informed decision to refuse (even life-saving) treatment supersedes offer of treatment The Principle of NonMaleficence Principle of avoiding harm to the patient justification for ‘acts and omissions’ distinction in law (withholding/withdrawing treatment that is not benefiting patient) The Principle of Beneficence Principle of doing what is best for the patient promotion of patient’s best interests prevent or remove harm encompasses sanctity of life principle when in conflict, non-malficience supersedes the principle of beneficence. The Principle of Justice Principle based on fairness, equity and equality treat similar cases in similar ways distribute health care resources (goods and service) fairly proper distribution of benefits and burdens Ethical decision-making within healthcare Autonomy, non-malficience; beneficence; and justice. Principles for ethical decision-making: - respect the autonomy of the individual - avoid harm - where possible achieve benefit - consider, fairly, the interests of all those affected Case Study : Ethics What should you say to a patient who phones the Helpline to ask how many tablets of drug X they need to take to kill themselves? Framework for ethical decisionmaking Begin by learning to recognise a moral issue Step 1: Gather all relevant information Step 2: Identify and clarify the ethical problem(s) Step 3: Analyse the problem by considering the various ethical theories or approaches Step 4: Explore the range of options or possible solutions Step 5: Make a decision Step 6: Implement and then reflect on the decision Guiding principles when dealing with dilemmas respect for autonomy of the patient (self- determination) beneficence (do good) non-malficience (do no harm) fidelity (truthfulness and confidentiality) veracity (honesty) justice (equitable distribution of benefits/burdens) There is often no right answer Any questions?