The Rowan Sexual Assault Referral Centre (SARC)
advertisement

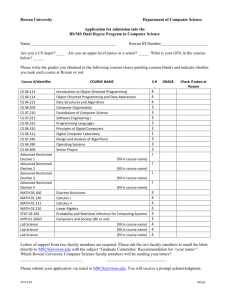
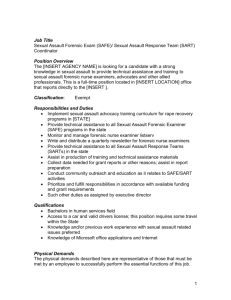
What is a S.A.R.C.? A one stop centre which will deliver a comprehensive and coordinated inter-agency response to all victims of sexual assault and rape, irrespective of their age, gender, sexual identity /orientation, ethnicity, or geographical location. The Rowan Sexual Assault Referral Centre (SARC NI) Nota Sexual Violence in Pre-Pubertal Children 25.11.15. Dr Olive Buckley OBE olive.buckley@northerntrust.hscni.net The Rowan Team Service Manager (wte) Clinical Director & Lead Forensic Medical Officer (0.4) Consultant Paediatrics (0.4) Consultant in Genitourinary Medicine (0.2) Registered (Band 7) Lead Nurse (wte) Registered Rowan Nurses (Band 5) (2.2) Administrator(Band 4) (wte) Administrator (Band 2) (0.5) Rota of Forensic Medical Officers Rota of Registered Rowan Nurses (Band 5) Rota of Consultant Paediatricians ISVAs – to be developed 50% PSNI 50% Department funding The Rowan The Rowan Team has offered support, advice and direct care to over 1688 individuals since we went live on 7th May 2013. Year 2 saw an increase in referrals by 18%. Year 3 has seen to date, five months in, a 23% increase. 1330 individuals were referred into the Rowan for support services, with a further 358 individuals seeking support, information and signposting onwards only. 49% of referrals were received within normal business hours i.e. Monday - Friday 9am 5pm, and 51% out of hours. Source of referral: 77% (n=971) came from the police, with 12% (n=156) being made by the individual affected him/herself; and the remaining 11% (n=134) came from 3rd parties. The Rowan 39% of those referred into the Rowan were children and young people i.e. <18 years; 61% were adults. Sexual violence and sexual abuse affects people across all age ranges, from infants to the very elderly. In relation to gender breakdown: the majority of individuals referred were female 87%; 13% were male. 4% of individuals identified as BAME. For a number of individuals and families who have engaged with the service English was their second language (2.4%). 43% attending The Rowan presented with complex and / or additional needs: living with chronic and enduring mental ill-health, physical ill-health and/or learning disabilities. 8% report of sexual violence related to intimate partner violence. 75% were reporting acute assaults i.e. an assault which had occurred within 7 days, usually ≤ 72 hours. The Rowan A number of individuals (n=24) have re-presented to The Rowan with a further and separate incident of sexual assault. Drug-facilitated sexual assault (DFSA) remains low at 5%. Individuals and families reporting sexual abuse and sexual violence have come from across the region, and a small number from outside the jurisdiction. The vast majority of victims knew their perpetrator(s). The Rowan Sexual Health Clinic: 64% of individuals aged 13+ have attended; 81% of children and young people (< 13 years) have been brought to their paediatric sexual health appointments. Rowan Year 1 Statistics (May 2013/14) 0-7 8-12 13-17 18-25 26-35 36-45 46-55 56-65 65+ Total Female 53 13 107 110 67 55 31 5 5 446 Male 18 12 9 8 8 10 4 5 0 74 Total 71 25 116 118 75 65 35 10 5 520 Rowan Year 2 Statistics May 2014/15 0-7 8-12 13-17 18-25 26-35 36-45 46-55 56-65 65+ Total Female 61 15 90 120 80 57 34 7 5 469 Male 16 13 6 9 10 5 3 0 0 62 Total 77 28 96 129 90 62 37 7 5 531 Figure 4 Number of Referrals per Trust Other BHSCT NHSCT SEHSCT SHSCT WHSCT Total Adults 92 72 45 61 56 3 329 Children & Adolescents 41 63 35 25 38 0 202 Total 133 135 80 86 94 3 531 Figure 5 Number of Child & Adult Referrals per Trust Republic of Ireland Annual report y/e Dec 2014 Cork *SATU: Numbers seen= 103 > 14yr Mullingar SATU : Numbers seen=85 >14yrs Donegal SATU: Numbers seen = 40 >14yrs Rotunda SATU: Numbers seen= 286 > 14yrs ( >14yr service but 8 12-14ys attended) Galway SATU: Numbers seen= 48 >14yr Waterford SATU: Numbers seen =66 > 14yrs Galway **CASATS : Numbers seen = 43 Limerick ( HSE mid west sexual assault advisory group): Numbers seen=19 > 14yrs *SATU= Sexual Assault Treatment Unit **CASATS=The Child and Adolescent Sexual Assault Treatment Service The Rowan Services Emotional support; Assessment of Hep B risk and rapid immunisation schedule/ immunoglobulin's when indicated Assessment for and administration of Emergency Contraception; Risk Assessment of HIV, and immediate access to PEPSE (<72 hours post-assault) to reduce likelihood of contracting HIV (by 80%); A Forensic and Medical Assessment by a Forensic Medical Officer (≤ 7 days for forensic swabs); For children <13 years, a joint Forensic Medical assessment with a Consultant Paediatrician; Risk Assessment for self harm, vulnerability, and safeguarding; The Rowan Services cont… For those adults who self-refer and have not reported to the Police, forensic samples can be stored securely for ≤ 7 years to give the victim an opportunity to consider reporting to the Police; Support in meeting with a Police officer from a specialist unit: Public Protection Unit (PPU) or Rape Crime Unit (RCU) to discuss engaging with the criminal justice system; Rowan Sexual Health Clinic: testing and treatment (where required) for Sexually Transmitted Infections (STIs); Referral into local counseling and support services e.g. Victim Support NI; Referrals into other support / acute services: Emergency Department, Mental Health Services, Social Services (Gateway / Regional Out of Hours); Liaison with existing support agencies / professionals; Follow-up support from the Rowan Team: telephone, face-to-face contact. Challenges: Lack of Disclosure 80% of victims do not report the offence(s) to the Police 72% of sexually abused children do not tell anyone at time 1 in 3 victims will never tell ANYONE National UK Prevalence Study of Child Abuse (Cawson et al, 2000) Barriers to Disclosure Fear of perpetrator Fear of disbelief Fear of being blamed Fear for family No one to tell Shame/Guilt Loyalty to Perpetrator Minimise or not recognise its wrong Myths and Stereotypes CSE Language/ pre-verbal Challenges: Managing “No complaint” The likelihood or otherwise, of a prosecution is NOT the criterion for a joint investigation. Children who have been the victim of ‘abuse’ will not always support an investigation or want to proceed through the criminal justice system. This does not remove the responsibility of Police and Social Services to conduct a thorough, effective and timely investigation” Why does a child refuse to support a criminal investigation? What happens where a child refuses to support a criminal investigation? What happens when a child is pre-verbal? What happens to children who do not have the capacity and do not really understand the process and do not engage? What about children with capacity, who refuse to engage with police but who agree to forensic samples being taken so they can decide in future if they want to engage in the criminal process? Are the child's therapeutic needs always considered when there is no engagement with the CJS? Examination CSA– why? Has alleged act occurred? Has any other act occurred? Is there medical evidence? Is there scientific proof? Are there safeguarding issues? What are the therapeutic needs? Challenges: New way of working! The challenges and benefits of working together to implement change Improving insight and understanding the roles of other professionals Working with “curious people” Reflective Case Study Role of GP GP may identify risk factors for abuse in children/families and take steps to prevent May recognise signs and symptoms opportunistically May be asked by agencies to see signs which are possibly due to abuse but more likely due to other causes GP will refer children on to SW/Paediatrician for specialised assessment Sharing of information with agencies On-going support for family during process Role of FMO Employed by PSNI To look for evidence of abuse by taking a history and examining the child Record Injury and Interpretation of Take forensic swabs/photos Collection of medico-legal evidence and maintaining a chain of evidence Samples for drug and alcohol from parents/carers Prepare a report for PSNI Give evidence in Court Role of Paediatrician May identify risk factors for abuse in children/families and take steps to prevent May recognise signs and symptoms opportunistically On referral will take a history from parents (and child) with consent (from person with PR) Assess/examine the child Arrange photographic documentation of any injuries- PSNI/medical photographer or Paediatrician Look for occult injury, disease process/exclude organic causes Carry out investigations e.g. blood Arrange further medical opinion if required e.g. ophthalmology, orthopaedics, radiology, dermatology, plastic surgery Look for co-morbidity/consequences or sequelae of abuse Prepare a medical report for referrer – SW/PSNI or Court Assess siblings if required Participate in Safeguarding Proceedings/give evidence in Court Follow up of child as required Combined Role of Paediatrician/FMO Assessment and treatment of injuries Check for Sexually Transmitted Infections Pregnancy assessment and Emergency Contraception Support Reassurance when appropriate Opinion Investigative Role of PSNI Respond to Incident Suspect Management Victim and Witness Management Forensic Management PPS Management Investigation Process Initial report Suspect management.. Arrest Medical examination Interviews Evidence gathering.... Medical examination of victim Victim and witness interviews; Scene examination Written statements and video recorded accounts Premises searches CCTV checks House to House enquiries Seizure of items for forensic examination Court Process Case evaluation... Charge/ Report Report to Public Prosecution Service • Magistrates Court • Preliminary Enquiry • Crown Court • Arraignment • Trial Challenges: Strategy Discussion Consider: “Protocol for Joint Investigations by Social Workers and Police Officers of Alleged and Suspected Cases of Child Abuse” AND “The Rowan Children and Young People Pathway” Protocol for Joint Investigations by Social Workers and Police Officers of Alleged and Suspected Cases of Child Abuse 1.8 Principles underpinning the Protocol for Joint Investigation (page 8) ‘the child’s welfare must always be paramount and this overrides all other considerations’ 2.27 (page 18) ‘The initial strategy discussion/ meeting will always include Police and Social Services and, as appropriate, may include a Forensic Medical Officer, GP, Paediatrician …’ 2.30 (page 19) ‘The initial Strategy Discussion/Meeting should address the following points: …should a forensic medical examination be undertaken and if so, by whom? Is a joint medical appropriate? If forensic medical examination is considered necessary form PJI6 must be completed by the relevant doctor …’ Rowan Children and Young People Pathway Challenges: Strategy Discussion Who should be involved? Strategy discussion with SW/PSNI/FMO/Paediatrician-who should examine, when and where? Joint FMO + Paediatrician or singly? Discussion should be with paed consultant not junior staff Escalate if don’t agree Challenges: Strategy Discussions Does child need examined? Do we think the unthinkable? Who and when should examine the child and where? Do STI tests need to be done now? Does child need hepatitis B prophylaxis? Is child at risk of HIV and if so, is PEPSE indicated? Does young person need emergency contraception? ? CSE Child and family anxiety Co-operation of child, aim to see in normal children wakening hours Should forensic samples be taken from child? Do forensic samples need to be taken of suspect? Safeguarding arrangements? Strategy Discussion: Who should be examined? Indications For A Paediatric Forensic Medical Assessment (Rowan) – FMO and Paediatrician Allegation / disclosure Witnessed event Genital Injuries – unexplained (Urgent)- may need EUA Sexually transmitted infections Behavioural Disturbance – self-harm, inappropriate sexualised behaviour Contact with a sexual offender Sibling / friend of another child suspected / confirmed as having been sexually abused Combination of concerns Strategy Discussion: Who should examine? Joint Paediatric Forensic Medical Assessment (FMO and Paediatrician) Best Practice Guidelines from RCPCH/ACPO Consider in all children/young people < 16 years Rowan Aim - all children < 13 years Discuss all children 13-18 years with “vulnerability factors” (Guidelines on Paediatric Forensic Examinations in Relation to Possible Child Sexual Abuse FFLM, Oct 2012) Strategy Discussion: When should examination take place? NB: Unexplained genital bleeding needs urgent (same day) assessment Forensic sampling up to 7 days Forensic examination up to 21 days for injury assessment No time line for historic reporting if h/o genital injuries Collection of other forensic material eg nappies, sheets Collection of early evidence Samples from suspects Timing of ABE Aim to see in wakening hours ( FFLM guidance) Challenges: Myths re Medical Examination Lack of understanding regarding what examination entails (Examination is inspection only i.e.“ no internals, no speculum”). Never say: “Don’t want to put the child through it” Unrealistic expectation regarding examination (Examination is only part of the jig-saw. No injury does not mean no assault) Never say: “The doctor will tell you what happened and will be able to tell if the child was abused ” The Challenge of Criminal Law (NI) Act 1967 Under Section 5 of the Criminal Law (NI) Act 1967, a person who has knowledge of and fails to report to the police an offence that carries a possible punishment of 5 years or more imprisonment commits an offence punishable by up to 5 years imprisonment. http://www.legislation.gov.uk/apni/1967/18/section/5 Challenges: Children who display sexually harmful behaviour Rowan victims had identified 12% of those who perpetrated sexual offences as being <18 years. Challenges in identifying normal, concerning and harmful behavior Suspects do not attend Rowan for forensic examinations Galway CASATS Annual Report 2014 Referrals from counties Galway , Clare , Sligo , Limerick , Westmeath , Kildare , Roscommon , Mayo , Tipperary , Offaly 43 (and 5 for follow up) 34 female 7 male 7 months to 20 yrs. Old Mean age 7.8 12 were acute 8 cases involved child assailants , 7 were male 13 alleged assailant was father 7 mothers partner 3 stranger 1 mother Galway CASATS Annual Report 2014 Of the 8 child assailants: 4 were under 12yr, 7 were male and 1 female Age unknown of 2 2 between 13yr and 18yr Sexual Assault Referral Centre (SARC) Northern Ireland Thank You