Ticks & Mites
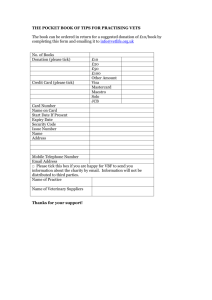
advertisement

Ticks, Mites and Associated Pathogens Overview: • Characteristics of the subclass Acari (ticks and mites) • Metastigmatid mites = ticks • Ticks and tick-borne pathogens • All other mites…. • Mites and mite-borne pathogens 1 Ticks and Mites (Subclass Acari) 1. Class Arachnida (Also includes spiders and scorpions 2. Characteristics of Acari (mites and ticks): a. sac-like, unsegmented body b. highly specialized mouthparts, capitulum w/ hypostome c. phytophagous, predatory, parasitic d. larvae 6 legs, nymph & adult 8 legs e. 4-stage life cycle, egg-larva-nymph-adult 2 Ticks and Mites - Classification Class Arachnida Subclass Acari Order Ixodida (= Metastigmata) (ticks) Order Mesostigmata (free-living, predaceous, and parasitic mites) Order Prostigmata (chiggers, follicle mites) Order Astigmata (house dust, storage & scabies mites) 3 Ticks - Classification Class Arachnida Ticks (3 families): Ixodidae Argasidae Subclass Acari Superorder Parasitiformes Nuttalliellidae Order 4 Source: http://tolweb.org/tree/phylogeny.html Mites - Classification Class Arachnida Subclass Acari Mesostigmatid Mites Superorder Parasitiformes Order 5 Source: http://tolweb.org/tree/phylogeny.html Mites – Classification (2) Class Arachnida Prostigmatid and Astigmatid Mites Subclass Acari Superorder Acariformes 6 Source: http://tolweb.org/tree/phylogeny.html Ticks and Mites - Classification • Recent validation of Acari suborders (ticks are ticks and mites are mites) • Recent reorganization within the ticks J. S. H. Klompen, William C. Black IV, James E. Keirans, and Douglas E. Norris. 2000. Systematics and Biogeography of Hard Ticks, a Total Evidence Approach. Cladistics 16, 79–102. Ivan G. Horak, Jean-Louis Camicas and James E. Keirans. 2002. The Argasidae, Ixodidae and Nuttalliellidae (Acari: Ixodida): a world list of valid tick names. Experimental and Applied Acarology 28: 27–54. 7 8 TICKS MITES 9 TICKS Characteristics of Ixodida (ticks) - approx. 900 species a. largest of acarines - larger than mites b. toothed hypostome c. Haller's organ (sensory pit on tarsi of first pair of legs) d. absence of claws on palps e. evolved as parasites of reptiles, adaptation to mammals associated with general reduction in body size Tick Families: Ixodidae - Hard Ticks, Argasidae – Soft Ticks, Nuttalliellidae - rare, S. Africa (single 10 species) Soft tick Hard tick (Family Argasidae) 11 (Family Ixodidae) Family Ixodidae Hard Ticks (approx. 683 species, 12 genera) Features: a. sexual dimorphism, male - enlarged scutum, female - shield b. mouthparts (capitulum) visible dorsally c. feed only once during each stage, often diurnal, males show little size increase d. range parasites, questing from vegetation, one large egg batch 12 Female hard tick Male hard tick 13 Typical Life History of Hard Ticks (most three-host): a. One-Host: Rhipicephalus (Boophilus) annulatus (Texas Cattle Fever Tick), all stages on same host, but leave host to molt, control using pasture rotation b. Three-Host: Dermacentor variabilis (American Dog Tick), each stage uses a different host - larva on small rodents, nymph on larger mammal, adult on another large mammal. Other three host: Rhipicephalus sanguineus (Brown Dog Tick) Amblyomma americanum (Lone Star Tick) 14 Description of medically-important hard ticks: Genus Approx. # Species World U.S. Amblyomma 100 Dermacentor 31 Hyalomma 30 Nosomma 1 Rhipicephalus 68 (includes Boophilus) Haemaphysalis 155 Ixodes 217 Margaropus 2 Bothriocroton 5 7 7 0 0 3 2 40 0 0 Distribution worldwide, mostly tropical worldwide Africa, Asia India, SE Asia Ethiopian / tropicopolitan worldwide worldwide southern, east Africa Austrailia 15 Genus Ixodes: Largest genus of hard ticks • Ixodes ricinus/persulcatus complex - Lyme Disease, HGE • I. ricinus (European Sheep tick) through Europe, Turkey, Iran • I. persulcatus (Taiga tick) Eurasian • I. scapularis (Black-legged tick) eastern US • I. pacificus (Western Black-legged tick) western US. • I. holocyclus Australia (tick paralysis) • I. rubicundus (Karoo tick) South Africa 16 Genus Haemaphysalis: Small, both sexes similar, important in enzootic cycles • H. leporispalustris (Rabbit tick) western hemisphere distribution (important maintenance vector for tularemia and RMSF) Genus Hyalomma: Large unornamented ticks • H. marginatum Russian states, southern Europe (Crimean-Congo hemorrhagic fever) 17 Genus Rhipicephalus: African origin, but several species worldwide in the tropics (now includes previous species of Boophilus, non-ornamented, one-host ticks) • R. sanguineus (Brown Dog tick) cosmopolitan distribution (RMSF, boutonneuse fever) • R. (Boophilus) annulatus (Cattle Fever tick) southern US, Mexico (Texas Cattle fever, field rotation for control) • R. (Boophilus) microplus (Southern cattle tick) Australia, Mexico, S. America 18 Genus Dermacentor: Ornate ticks • D. variabilis (American dog tick) eastern US, Canada, Mexico (tularemia, RMSF) • D. andersoni (Rocky Mountain wood tick) western North America (tularemia, RMSF, Colorado tick fever) • D. albipictus (Winter tick) across Canada • D. occidentalis (Pacific coast tick) Oregon, California 19 Genus Amblyomma: Large ornate ticks • A. americanum (Lone Star tick) central/eastern US - S. American (RMSF, tularemia) • A. cajennense (Cayenne tick) Texas, S. America, Caribbean • A. hebraeum (Bont tick) S. Africa 20 Family Argasidae Soft Ticks (183 species, 4 genera) Features: a. slight sexual dimorphism, only slight swelling from feeding b. scutum absent c. capitulum not visible dorsally d. palpi leg-like and flexible e. intermittant "rapid" feeder, nocturnal f. sometime several nymphal instars, some non-feeding larvae g. lair parasites, several egg batches, dry adverse environments 21 Soft tick Hard tick (Family Argasidae) 22 (Family Ixodidae) Typical life history of soft ticks: a. Many-host cycle. Often one larval host and several nymphal and adult hosts. Adult female lays eggs after each feeding Argas persicus (Fowl Tick) chicken houses, bird nests, cosmopolitan Ornithodoros moubata (African Relapsing Fever Tick) feeds on sleeping humans, southern Africa Otobius megnini (Spinose Ear Tick) adult nonfeeding, nymph problem 23 Description of medically-important soft ticks: Genus Approx. # species Distribution Argas 55 worldwide Ornithodoros 38 worldwide Otobius 3 western hemisphere Carios 84 worldwide 24 Genus Argas: most nocturnal bird-associated • A. persicus (Fowl tick) cosmopolitan (economic importance, painful bite) • A. arboreus east, S. Africa (arbovirus vector) 25 Genus Ornithodoros: Reservoirs and vectors of relapsing fever • O. moubata (African Relapsing Fever tick) S. Africa (species complex) numerous species Genus Otobius: Adults do not feed • O. megnini (Spinose ear tick) western hemisphere, Africa, India (nymphal infestations in ears) 26 Tick Sampling a. b. c. observation on hosts and premises Dragging/flagging CO2 - baited traps Tick Control a. b. Natural predators Repellents/toxicants for human use I. DEET (apply to skin) II. Pyrethroids (apply to clothing) 27 • Cultural/mechanical control I. II. III. remove harborage for hosts/ticks destroy hosts pasture rotation (one-host only) • Resistant livestock • Anti-tick vaccine • Chemical control on animal host, or acaricide in habitat 28 AVOIDING TICKS • Wear light-colored clothing to allow you to see ticks that are crawling on your clothing. • Tuck your pants legs into your socks so that ticks cannot crawl up the inside of your pants legs. • Apply repellants to discourage tick attachment. Repellents containing permethrin can be sprayed on boots and clothing, and will last for several days. Repellents containing DEET (n, n-diethyl-mtoluamide) can be applied to the skin, but will last only a few hours before reapplication is necessary. Use DEET with caution on children. Application of large amounts of DEET on children has been associated with adverse reactions. 29 AVOIDING TICKS - II • Conduct a body check upon return from potentially tick-infested areas by searching your entire body for ticks. Use a hand-held or full-length mirror to view all parts of your body. Remove any tick you find on your body. • Parents should check their children for ticks, especially in the hair, when returning from potentially tick-infested areas. Additionally, ticks may be carried into the household on clothing and pets. Both should be examined carefully. 30 Tick Removal: 1. Use fine-tipped tweezers or shield your fingers with a tissue, paper towel, or rubber gloves. When possible, persons should avoid removing ticks with bare hands. Removal of an embedded tick using fine-tipped tweezers. 2. Grasp the tick as close to the skin surface as possible and pull upward with steady, even pressure. Do not twist or jerk the tick; this may cause the mouthparts to break off and remain in the skin. 31 3. Do not squeeze, crush, or puncture the body of the tick because its fluids (saliva, body fluids, gut contents) may contain infectious organisms. 4. After removing the tick, thoroughly disinfect the bite site and wash your hands with soap and water. 5. Save the tick for identification in case you become ill. This may help your doctor make an accurate diagnosis. Place the tick in a plastic bag and put it in your freezer. Write the date of the bite on a piece of paper with a pencil and place it in the bag. 32 33 34 Haemaphysalis bremneri mouthparts, showing toothed, sawlike hypostome. Photograph copyright 2001 Steve Barker 35 Photograph copyright 2001 Steve Barker Otobius megnini 36 Medical Importance of Ticks 1. Dermatosis - inflammation, itching , swelling at site of bite 2. Exsanguination - anemia can result from heavy infestation 3. Otoacariasis - auditory canal infestation, poss. secondary infection 4. Predispose to myiasis and infection 5. Tick paralysis (envenomization) 6. Pathogen transmission (virus, rickettsia, bacteria, spirochaete, protozoa, filarial worms) 37 Factors Accounting for High Vector Potential of Ticks 1. Persistent hematophagous feeders 2. Relatively slow feeding time allows time for pathogen transfer 3. Typically have a wide host range 4. Longevity increases chances of acquiring and transmitting a pathogen 5. Transovarial transmission of some pathogens 6. Few natural enemies, highly sclerotized (resistant to environmental stress) 7. High reproductive potential - up to 18,000 eggs and parthenogenesis in some species 38 Non-viral Tick-Borne Pathogens • • • • • • • • • Lyme Disease (Borrelia burgdorferi) Babesia microti (malaria-like) Ehrlichia species Relapsing fever (Borrelia species) Tularemia (Francisella tularensis) RMSF (Rickettsia rickettsii) Tick typhus (Rickettsia sp.) Heartwater (Cowdria ruminantium) Anaplasmosis (Anaplasma sp.) 39 Some Tick-Borne Pathogens • Human monocytic ehrlichiosis (HME), caused by Ehrlichia chaffeensis a new monocytotropic ehrlichia, was discovered in 1986 and human granulocytic ehrlichiosis (HGE), caused by the HGE agent (newly named Anaplasma phagocytophilum), a new granulocytotropic ehrlichia, was discovered in 1994. • In 1999 another granulocytotropic ehrlichia, E. ewingii which was previously known as a canine pathogen has been recognized as human pathogen. E. sennetsu (renamed to Neorickettsia sennetsu) is another monocytotropic Ehrlichia sp. and the first human pathogen discovered in Japan in the 1950’s and recently found in Malaysia. 40 This phylogram is constructed based on 16S rRNA sequences of these species. Nomenclature has been changed from original names based on 16S rRNA sequences which divided them into four genera groups. Family Anaplasmataceae now contains four genera: Ehrlichia, Anaplasma, 41 Neorickettsia, and Wolbachia. Ehrlichiosis and Anaplasmosis • Small gram-negative bacteria that grow in membrane-bound vacuoles in leukocytes or platelets • Typically 1-3 um cocci • Different species of Ehrlichia infect different types of host cells • Not all species transmitted by arthropods • HME (human monocytic ehrlichiosis), E. chaffeensis • HGE (human granulocytic ehrlichiosis), (A. phagocytophila) • HGE overlap with Lyme disease - both transmitted by Ix. scapularis complex members in US 42 Ehrlichia chaffeensis is principally transmitted by the lone star tick (Amblyomma americanum). White-tailed deer are a major host of lone star ticks and appear to represent one natural reservoir for E. chaffeensis. Antibody to E. chaffeensis has been found throughout deer populations in the southeastern and midwestern United States, and the organism has been 43 cultured from deer blood. (CDC) Cases of HME are predominantly found in the South and south-central regions where the suspect vector, the Lone Star tick (Amblyomma americanum) is present. Amblyomma americanum Lonestar tick Associated with E. chaffeensis transmission (HME) 44 Average annual incidence of reported human monocytic ehrlichiosis (HME) by county, using 1995 45 population census data. The HGE agent has been associated with the blacklegged tick (Ixodes scapularis) in the northeastern and upper midwestern United States. The western blacklegged tick (Ixodes pacificus) is a vector in northern California. Ixodes ricinus has been shown to be a vector of A. phagocytophila in Europe. Deer, elk, 46 and wild rodents are likely reservoirs. Ixodes pacificus - western black-legged tick Cases of HGE have been reported primarily in the Northeast and Midwest regions and are associated with the bite of deer ticks (Ixodes scapularis). A few cases on the Pacific coast are associated with the related species, Ixodes pacificus. Ixodes scapularis - black-legged deer tick 47 Average annual incidence of reported human granulocytic ehrlichiosis (HGE) by county, using 1995 population census data. 48 Distribution of the Tick Vectors of Ehrlichia and Anaplasma in the United States 49 Ehrlichiosis - Epidemiology • During 1986 to 1997, health departments and other diagnostic laboratories reported over 1200 cases of human ehrlichiosis to CDC. • Approximately two-thirds were cases of HME. CDC compiles the number of cases reported by the state health departments. • Ehrlichiosis is a nationally notifiable disease; however, not all state health departments have reported cases of ehrlichiosis to CDC. 50 Reported Cases of Ehrlichiosis in the United States51 Approximate Seasonal Distribution of HGE in the United States 52 States where Ehrlichiosis is a notifiable disease (green) 53 Lyme Disease • Lyme disease was named in 1977 when arthritis was observed in a cluster of children in and around Lyme, Connecticut. • Other clinical symptoms and environmental conditions suggested that this was an infectious disease probably transmitted by an arthropod. • Further investigation revealed that Lyme disease is caused by the spirochete bacterium, Borrelia burgdorferi. • These bacteria are transmitted to humans by the bite of infected deer ticks and cause more than 16,000 infections in the United States each year. 54 Lyme Disease - Vectors • Black-legged ticks (Ixodes scapularis) are responsible for transmitting Lyme disease bacteria to humans in the northeastern and north-central United States. • On the Pacific Coast, the bacteria are transmitted to humans by the western black-legged tick (Ixodes pacificus). • Ixodes ticks are much smaller than common dog and cattle ticks. In their larval and nymphal stages, they are no bigger than a pinhead. • Ticks feed by inserting their mouths into the skin of a host and slowly take in blood. • Ixodes ticks are most likely to transmit infection after feeding for two or more days. 55 56 Ixodes scapularis female, male, nymph, larva White-tailed deer important vertebrate host of adult ticks 57 58 Borrelia sp. Transmission Greatest risk 59 Lyme Disease - Risk • In the United States, Lyme disease is mostly localized to states in the northeastern, mid-Atlantic, and upper north-central regions, and to several counties in northwestern California. • In 1999, 16,273 cases of Lyme disease were reported to the Centers for Disease Control and Prevention (CDC). • Ninety-two percent of these were from the states of Connecticut, Rhode Island, New York, Pennsylvania, Delaware, New Jersey, Maryland, Massachusetts, and Wisconsin. • Outdoor exposure - recreational, professional. 60 61 62 Year 63 Month of Lyme disease onset for reported cases, United States - 1992-1998. 64 Lyme Disease - Symptoms • Lyme disease most often presents with a characteristic "bull's-eye" rash, erythema migrans, accompanied by nonspecific symptoms such as fever, malaise, fatigue, headache, muscle aches (myalgia), and joint aches (arthralgia). • The incubation period from infection to onset of erythema migrans is typically 7 to 14 days but may be as short as 3 days and as long as 30 days. • Some infected individuals have no recognized illness (asymptomatic infection determined by serological testing), or manifest only non-specific symptoms such as fever, headache, fatigue, and myalgia. 65 Lyme spirochete Borrelia burgdorferi 400x ECM erethyma chronicum migrans (bull’s eye rash) 66 Lyme Disease - Treatment/Control • Antibiotic treatment for 3-4 weeks with doxycycline or amoxicillin is generally effective in early disease. • Cefuroxime axetil or erythromycin can be used for persons allergic to penicillin or who cannot take tetracyclines. • Later disease, particularly with objective neurologic manifestations, may require treatment with intravenous ceftriaxone or penicillin for 4 weeks or more, depending on disease severity. • In later disease, treatment failures may occur and retreatment may be necessary. 67 Babesiosis • Babesiosis is caused by hemoprotozoan parasites of the genus Babesia. • While more than 100 species have been reported, only a few have been identified as causing human infections. • Babesia microti and Babesia divergens have been identified in most human cases, but variants (considered different species) have been recently identified. • Little is known about the occurrence of Babesia species in malaria-endemic areas where Babesia can easily be misdiagnosed as Plasmodium. 68 Babesiosis - Life Cycle • Babesiosis is transmitted by ixodid (hard-bodied) ticks. Ticks become infected by feeding on an infected vertebrate animal (rodents, cattle, wild animals) or transovarially (ticks thus can be vectors as well as reservoirs), depending on the Babesia species. • In the ticks, the parasites develop and multiply. Transmission to the next vertebrate host occurs during a subsequent blood meal of the tick. • Inside the vertebrate host, the parasites directly invade the erythrocytes (without the exo-erythrocytic liver stage required by human malaria parasites), where they undergo successive cycles of multiplication and reinvasion. • The cycle is closed when the infected blood is ingested by a tick feeding on the mammalian host. Babesia can also be acquired by transfusion of blood or blood products. 69 Babesiosis - Geographic Distribution • Worldwide, but little is known about the prevalence of Babesia in malaria-endemic countries, where misdiagnosis as Plasmodium probably occurs. • In Europe, most reported cases are due to B. divergens and occur in splenectomized patients. • In the United States, B. microti is the agent most frequently identified (Northeast and Midwest), and can occur in nonsplenectomized individuals. • Two variants, arguably different species, have been reported in the U.S. states of Washington and California (WA1- type and related parasites) and Missouri (MO1). 70 Tick-Borne Pathogens • • • • • • • • • Lyme Disease (Borrelia burgdorferi) Babesia microti (malaria-like) Ehrlichia species Relapsing fever* (Borrelia species) Tularemia (Francisella tularensis) RMSF (Rickettsia rickettsii) Tick typhus (Rickettsia sp.) Heartwater (Cowdria ruminantium) Anaplasmosis (Anaplasma sp.) 71 *soft tick Rocky Mountain Spotted fever a. pathogen Rickettsia rickettsii b. Nearctic and Neotropical, first described in US c. human disease, now most common in eastern US, human encroachment d. headache, lumbar ache, malaise, 2-5 day incubation, antibiotic treatment e. transmission by bite, trans-stadial and TOT f. D. variabilis eastern, D. andersoni western, Amblyomma cajennense neotropical 72 Characteristic spotted rash of latestage Rocky Mountain spotted fever on legs of a patient, ca. 1946 73 Dermacentor variabilis American dog tick Dermacentor andersoni Rocky Mountain wood tick 74 Figure 9. Reported cases of Rocky Mountain spotted fever in the United States, 1942-1996. 75 Figure 10. Seasonal distribution of reported cases of Rocky Mountain spotted fever, 1993-1996. 76 Figure 11. Number of reported cases of Rocky Mountain spotted fever by state and region, 1994-1998. 77 Tick-borne Viruses 1. More than 100 arboviruses associated with ticks; 116 tick species, 32 argasid, 84 ixodid. 2. Many based only on isolation of virus, disease potential unknown 3. Most important all exist as zoonoses, and TOT occurs in some 78 Colorado tick fever (Reoviridae, genus Orbivirus) a. focal zoonosis in Rocky Mountain states and South Dakota of US, and western Canada, overwinters in nymph b. main vector to humans is Dermacentor andersoni, no TOT, other zoonotic vectors c. reservoir hosts - rodents, squirrels, porcupines d. disease is dengue-like, 3-6 day incubation in humans, severe in children 79 Tick-borne encephalitides (Flaviviridae, genus Flavivirus), two forms a. Russian Spring Summer encephalitis (far eastern form) I. taiga forest in E. Russia and NE China II. vector is Ixodes persulcatus b. Tick-Borne encephalitis (western form) I. coniferous and temperate deciduous forests II. vector is I. ricinus c. Overlap of tick species in western Russia, both forms of virus present, other ticks involved in focal transmission, TOT in ticks, "holiday" disease, tick bite or drinking milk of infected goat 80 Kyasanur Forest disease (genus Flavivirus) a. Southern India, disease discovered following monkey deaths, and human illness/death b. vector is Haemaphysalis spinigera (H. turturis - zoonotic cycle) c. human contact in forest, intrusion in foci of infection d. fever, headache, severe muscle pain - diphasic - cough, GI disturbance, prolonged recovery, 5% mortality 81 Crimean-Congo hemorrhagic fever (Bunyaviridae, genus Nairovirus) a. Russian states, Asia, Africa, Europe - first seen in Russian soldiers b. 27 tick taxa associated with zoonotic maintenance, TOT in some species c. human epidemics associated with Hyalomma marginatum and other sp. of Hyalomma d. infection via bite, or crushing tick on skin e. acute febrile illness with hemorrhagic symptoms 82 Others: Louping Ill virus I. ricinus sheep, UK Omsk Hemorrhagic Fever virus Dermacentor sp. and Ixodes sp. Siberia Powassan Encephalitis virus Dermacentor sp. and Ixodes sp. US 83 MITES Usually less than 1 mm long, life cycle: egg-larvanymph-adult, 1-3 nymphal stages 1. oviposition - usually egg, but some ovoviviparous 2. egg -- adult, 8 days to several weeks, average 4 weeks Abdomen joined to cephalothorax, no segmentation 1. Typical 3 legs - larva, 4 legs - adult, but reduction in some species 2. Chelicerae for tearing or piercing in parasitic species 84 MITES Free-living, predaceous and parasitic - endo/ecto Skin damage to livestock, as much as $5 million /year in economic damage Effects on humans and animals: 1. 2. 3. 4. dermatitis or other tissue damage loss of blood or other tissue fluids transfer of pathogenic agents cause of strong allergic reactions 85 ACARIASIS - infestation with mites Possible sites of infestation: • external, inner and middle ear • respiratory passages and lungs • nasal passages • lymphatic tissue 86 MITES Order Mesostigmata A. Relatively large mites, 0.2 - 2.0 mm length B. Pair of stigmata located behind and lateral to third coxa, associated with peritremes C. Many are predatory, biocontrol uses D. Not host specific, human host unusual but will cause skin disorders (Laelaps sp., Ornithonyssus sp.) 87 Mesostigmatid Mite 88 MITES Order Prostigmata A. Heterogenous group, weakly sclerotized, 0.1 10.0 mm in length B. Stigmata present, usually at base of chelicerae, difficult to see C. More than 50 families in suborder, some medically important (Demodex sp., Trombiculid mites) 89 90 MITES Order Astigmata A. Stigmata and tracheae absent, integumental respiration B. Small (0.2-1.2mm), thin-skinned mites without obvious shields C. Coxae sunk into ventral body wall (epimeres) D. Palps are 2-segmented and chelicerae pincer-like (Sarcoptes sp., Dermatophagoides sp., Tyroglyphus sp.) 91 Sarcoptes scabei 92 MITES - Control Sampling 1. Removal from outside host, with wash 2. Skin scraping for intradermal forms 3. Drag similar to tick flagging 93 MITES - Control Direct host treatment a. for human scabies, repeated treatments with ointments containing sulfur, benzyl benzoate, thiabendazole, or an approved insecticide (permethrin) - lindane resistance b. injection of products such as Ivermectin c. insecticidal dipping for domestic animals 94 MITES - Control • Premise spray a. • Repellent/Toxicant a. b. • spray roosts for chicken/fowl mites permethrin apply to socks, bottom of pant legs Quarantine 95 Mite-Borne Pathogens • Rickettsialpox (Rickettsia akari) • Scrub typhus (Orientia tsutsugamushi) 96 Rickettsialpox Rickettsia akari Liponyssoides mite vector House mice, rats - vertebrate hosts in urban areas 97 Chiggers • Chiggers, also known as "redbugs, jiggers or harvest mites", are the immature stages of a tiny red mite. • They inhabit areas of tall grass, associated with low, wet spots, ponds and stream banks, wild berry patches and forest underbrush. • The larvae attach themselves to the clothing of people or to the fur of passing animals. Before settling down to feed, chiggers move to a constriction such as sock tops, waist bands or armpits. • Feeding chiggers inject a salivary fluid which dissolves the host's cells, then suck up the liquefied tissue. Within a few hours, small, reddish, intensely itching welts appear. • These bites may continue to itch for several days up to two weeks after the chigger is dislodged. 98 99 US distribution of chiggers - other areas also have focally high populations The Culprit Larval chigger mite 100 Scrub typhus (Orientia tsutsugamushi) Vector - larval Leptotrombidium mites\ Reservoir - mites via TOT, transitory rodent infections Distribution - SE Asia and islands of Indian Ocean and SW Pacific, coastal North Queensland, Australia Exposure - outdoor recreation or occupational exposure - disturbed habitat 101 102 Chigger Protection • Stay out of areas where chiggers are likely to be present including woodlots, pastures, roadside ditches or other areas with tall grasses and weeds. Chiggers are especially common in moist low-lying areas. • Wear loose-fitting clothing and avoid sitting or reclining on the ground when camping, picnicking or working outdoors. • Apply a repellent containing DEET (N,N-diethyl-metatoluamide) to shoes, socks and trousers before entering chigger-infested areas. Caution: some individuals may be sensitive to DEET. Always read and follow label directions. 103 Chigger Protection - II • Immediately after possible exposure to chiggers take a bath, thoroughly scrubbing the body with hot soapy water. This will kill or dislodge many of the chiggers. • When bites begin to itch, apply rubbing alcohol, followed by one of the non-prescription local anesthetics. A baking soda paste, calamine lotion or product such as "After-Bite" also will help reduce discomfort. • Avoid scratching bites since this only increases irritation and may lead to secondary infection of the bite. • Where chiggers are a problem in landscapes, keep lawns and shrubbery well manicured especially in areas adjacent to dwellings. Eliminate tall grasses and weeds. Chiggers also can be reduced by spraying infested foliage with carbaryl (Sevin), chlorpyrifos (Dursban) or diazinon. 104 105 Sarcoptes scabei 106 Scabies • Scabies is an infestation of the skin with the microscopic mite Sarcoptes scabei. Infestation is common, found worldwide, and affects people of all races and social classes. • Scabies spreads rapidly under crowded conditions where there is frequent skinto-skin contact between people, such as in hospitals, institutions, child-care facilities, and nursing homes. 107 Scabies - Symptoms • Pimple-like irritations, burrows or rash of the skin, especially the webbing between the fingers; the skin folds on the wrist, elbow, or knee; the penis, the breast, or shoulder blades. • Intense itching, especially at night and over most of the body. • Sores on the body caused by scratching. These sores can sometimes become infected with bacteria. 108 Scabies - Infestation • By direct, prolonged, skin-to-skin contact with a person already infested with scabies. Contact must be prolonged (a quick handshake or hug will usually not spread infestation). Infestation is easily spread to sexual partners and household members. Infestation may also occur by sharing clothing, towels, and bedding. • People with weakened immune systems and the elderly are at risk for a more severe form of scabies, called Norwegian or crusted scabies. 109 110 DEMODEX 111 Demodex - the follicle mites 112 113 Dermatophagoides 114 House Dust Mites - Dermatophagoides • The term 'house dust mites' is used originally to refer to those mites belonging to Pyroglyphidae. At present, the term 'dust mites' is widely used instead and this is in reference to all pyroglyphid and nonpyroglyphidites that are implicated in dust borne respiratory allergy. • House dust mites cause 25% of all allergies and 50% of all asthmatic diseases are traceable to house dust mites 115 Areas at highest risk for dust mite problems. 116 Ticks, Mites and Associated Pathogens Summary: • Characteristics of the order Acari (ticks and mites) • Metastigmatid mites = ticks • MANY tick-borne pathogens… • Mesostigmatid mites, prostigmatid mites and astigmatid mites • Infestation, allergy, scrub typhus, rickettsialpox 117