ppt - American Academy of Pediatrics
advertisement

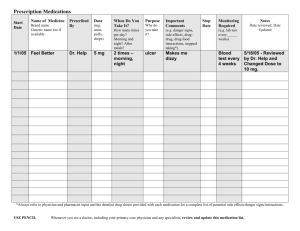
Simple Solutions to the Complicated Problem of Home Medication Use Thursday, December 18, 2008 12:00 – 1:00 p.m. EST © American Academy of Pediatrics 2008 Moderator: Karen Frush, MD, FAAP Chief Patient Safety Officer Duke University Health System Durham, North Carolina DISCLOSURES Financial Relationships Melissa A. Singleton, MEd, Project Manager-Consultant has disclosed a financial relationship with an entity producing, marketing, re-selling, or distributing health care goods or services consumed by, or used on, patients. Her husband is employed by Walgreen Co. as a Workforce Administration Manager (technology position) for the company’s call centers. The AAP determined that this financial relationship does not relate to the educational assignment. None of the other involved individuals (Speaker, Moderator, Project Advisory Committee members, or Staff) has disclosed a relevant financial relationship. Refer to full AAP Disclosure Policy & Grid available below for download. DISCLOSURES Off-Label/Investigational Uses Our Speaker, Kathleen E. Walsh, MD, MSc, does intend to discuss an unapproved/investigative use of a commercial product/device in her presentation. None of the other involved individuals (Moderator, Project Advisory Committee members, or Staff) has disclosed plans to discuss an unapproved/investigative use of a commercial product/device. Refer to full AAP Disclosure Policy & Grid available below for download. This activity was funded through an educational grant from the Physicians’ Foundation for Health Systems Excellence. Visit our website: http://www.aap.org/saferhealthcare Resources: Useful strategies, valuable information links, and expert advice on reducing or eliminating medical errors affecting children. Webinars: Register for an upcoming, live Webinar, and earn a maximum of 1.0 AMA PRA Category 1 Credit™. Or, access a full archive, including audio, from one of the past Webinar offerings. Or, download just the Podcast or slide set from an archive. Latest News: Links to recent articles relating to pediatric patient safety. Email List: An e-community dedicated to pediatric patient safety issues and information exchange with other clinicians. Parents’ Corner: Resources to help parents understand what they can do to help ensure their optimal safety in the health care that their child receives. CME CREDIT Live Webinar Only The American Academy of Pediatrics (AAP) is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. The AAP designates this educational activity for a maximum of 1.0 AMA PRA Category 1 Credit™. Physicians should only claim credit commensurate with the extent of their participation in the activity. This activity is acceptable for up to 1.0 AAP credits. These credits can be applied toward the AAP CME/CPD Award available to Fellows and Candidate Members of the American Academy of Pediatrics. OTHER CREDIT Live Webinar Only This program is approved for 1.0 NAPNAP contact hours of which 1.0 contain pharmacology (Rx) content per the National Association of Pediatric Nurse Practitioners Continuing Education Guidelines. The American Academy of Physician Assistants accepts AMA PRA Category 1 Credit(s)TM from organizations accredited by the ACCME. Important Note: You must have been pre-registered, and viewing the live webinar, in order to claim CME or other credit for your participation. LEARNING OBJECTIVES Upon completion of the webinar, participants will be able to: • Cite the epidemiology of home medication errors, and what questions remain unanswered. • Recognize clinical situations where patients may be at high risk for home medication errors. • Apply at least one strategy to reduce home medication errors in your patient population. Speaker: Kathleen E. Walsh, MD, MSc Assistant Professor of Pediatrics University of Massachusetts Medical School Worchester, Massachusetts Simple solutions to the complicated problem of home medication use Kathleen E Walsh, MD, MSc University of Massachusetts School of Medicine Case 1 10 mo old with anemia prescribed – Fer-gen-sol (15mg/0.6 ml) 1.2 ml orally once daily – Parents given instructions by nurse who spoke some Spanish – No one at pharmacy spoke Spanish, bottle labeled in English After med, child vomited, appeared ill. ED iron level 365 mcg/dl (normal 60-180) Parent reported administering medication with a home tablespoon (15 ml) Outline Background Home medication errors Unanswered questions and next steps Take home points Even home medication errors are a systems problem There are several simple solutions to help prevent errors in the homes of your patients now Outpatient quality improvement just getting started Background 44,000 to 98,000 patients die a year from medical errors 21st Century Healthcare System –Safety –Effectiveness –Patient-centeredness –Timeliness –Efficiency –Equity Definitions Medication error: error in drug ordering, dispensing, administering, or monitoring Adverse drug event: injury that results from medication use Adverse drug events and medication errors Medication errors Error without adverse event Adverse drug events Adverse Error event with adverse without error event Swiss cheese model Reduce human error 1. Person-centered 2. Systems-centered Reason, J. BMJ 2000; 320(7237): 768-70. Swiss cheese model Pharmacy MD Parent No No interpreter interpreter, Label in Did not give Patient receives Wrong measurement English syringe overdose instrument Outpatient medication pathway Ordering Dispensing Patient Monitoring Administering What’s different about the home? Vast majority of US medications taken at home Liquid medications – Much more complex to calculate – Reconstituted from powder – Measurement devices Cutting or crushing pills Vomiting or spitting medicines Day care or school administration of medications Risks of over-the-counter medicines Many children live in poverty The solution “Every system is perfectly designed to achieve exactly the results it achieves” -Don Berwick Outline Background Home medication errors Unanswered questions and next steps Methods in existing literature Medical record review Parent interview Bring meds to clinic to review Demonstration of the dose in clinic Home visit Outpatient pediatric adverse drug events Prospective cohort study of 1,788 patients who had medications prescribed at 6 Boston practices Medical record review and parent survey 3% had a preventable ADE (injury due to an error) – E.g.: 9 yo with strep prescribed amoxicillin. Parent did not fill the prescription and child returned with persistent symptoms 13% had a nonpreventable ADE – E.g.: 2 yo given cold medicine developed anaphylaxis Kaushal R, Goldman D, Keohane C, et al. Adverse Drug Events in Pediatric Outpatients. Ambulatory Pediatrics. 2007;7:383-9. Kaushal R, Goldman D, Keohane C, et al. Adverse Drug Events in Pediatric Outpatients. Ambulatory Pediatrics. 2007;7:383-9. Outpatient oncology errors Retrospective review of medical records 4 oncology clinics in Georgia, New Mexico, California, and New England 117 pediatric visits with 913 medications – 18% had a medication error 1,259 adult patient visits with 10,995 medications – 7% had a medication error Walsh KE, Dodd KS, Seetharaman K, et al., Medication Errors among Adults and Children with Cancer in the Outpatient Setting. Journal of Clinical Oncology. (in press). Outpatient oncology errors Monitoring Other Order 36% 56% Administration Dispense Outpatient oncology errors 77% of pediatric errors were in medications used at home – E.g.: child with ALL and abscess is given incorrect frequency of antibiotic at home, abscess does not improve and requires surgical drainage 7% of adult errors were in medications used at home Chemotherapy administration errors Prospective observational study in an outpatient oncology clinic Parents asked to bring in the child’s chemotherapy and demonstrate how they would measure and administer the dose – 30% did not bring in some of the chemotherapy 17 errors in 69 patients with 172 medications – 12 administration and 5 prescribing Taylor JA., Winter L, Geyer LJ, et al., Oral outpatient chemotherapy medication errors in children with acute lymphoblastic leukemia. Cancer, 2006. 107(6): p. 1400-6. Antipyretic dosing by parent report Li S, Lathcer B, Crain E. Acetaminophen and ibuprofen dosing by parents. Pediatric Emergency Care 2000;16:394-7. Chronic acetaminophen overdose 47 cases of hepatotoxicity after multiple overdoses of acetaminophen1 – 20 survived, including 4 liver transplants – 3 causes: Parent ran out of pediatric meds and used adult meds, misread label, fever was high so gave more medicine Henretig FM, Selbst SM, Forrest C, et al. Repeated acetaminophen overdosing. Clin Pediatr. 1989 Nov;28(11):525-8. Acetaminophen dosing intervention: Color syringes Color chart, material to help identify their child’s color, syringe with colored lines Compared with conventional methods, less errors with color syringes Average deviation from correct dose 26% for conventional vs. 1.7% for color syringes Frush KS, Luo X, Hutchinson P, Higgins JN. Evaluation of a method to reduce over-the-counter medication dosing error. Arch Pediatr Adolesc Med. 2004 Jul;158(7):620-4. Dispensing cup: simple solution or complex problem 34 calls to poison control centers with dispensing cup errors 3 types: 1. Confusing teaspoon and tablespoon on the cup 2. Assumption that the dispensing cup was the unit of measure 3. Assumption that the full dispensing cup was the actual dose Litovitz T. Implication of dispensing cups in dosing errors and pediatric poisonings: a report from the American Association of Poison Control Centers. The Annals of pharmacotherapy 1992; Jul-Aug;26(7-8):917-8. Simple solution: syringe with line marked Prescription and verbal instructions 2. Prescription with syringe and demonstration 3. Prescription, syringe with a line marked, and demonstration 1. 1. 37% correct – 2. 83% correct – 3. 32%-147% dose 20%-152% dose 100% correct McMahon SR, Rimsza ME, Bay RC. Pediatrics 1997; 100(3 Pt 1): 330-3. McMahon SR, Rimsza ME, Bay RC. Pediatrics 1997; 100(3 Pt 1): 330-3. 1970 Home visit study 104 visits to parents recruited from a private pediatric practice using home medications Observation of medication administration, measurement of the home teaspoon, interview Only 1/3 of teaspoons measure 4.5-5.5 ml 4 parents misunderstood dosing instructions 15 parents were non compliant with instructions Arnhold, RG, Adebonojo FO, Callas ER, et al., Patients and prescriptions comprehension and compliance with medical instructions in a suburban pediatric practice. Clinical Pediatrics, 1970. 9(11): p. 648-651. Cold medicine Cold medicine toxicity 10 infant overdose deaths; 8 accidental. Several cold meds involved Gunn: 1) overdose in 3 yo with VP shunt; 2) healthy 3 yo with poor LV function; 3) repeated overdoses in a healthy 9 mo old with an at home arrest 1965-1990: >100 cases of phenylpropanolamine toxicity, including several intracranial hemorrhage Cold medicine effectiveness 1. RCT: 0.5 to 5 year olds: brompheniramine + PPA + phenylephrine vs. placebo vs. nothing 2. RCT: 1.5 to 12 years: codeine vs. placebo vs. dextromethorphan 3. No change in symptom scores Review of trials 1950-1991 4. No change in symptom scores 2 studies with preschoolers showed no effect. 2 with 6 and older showed some symptom improvement RCT: 6 mo to 5 years; brompheniramine + PPA vs. placebo No change in symptoms, significantly more sleep Cold medicine solution Summary of the literature Rates and types of errors vary by study method and target population Only one study in home where all medicines, including over-the-counter medicines, and administration tools can be reviewed Parent errors appear to be common Parents may be unaware of many errors they make Outline Background Home medication errors Unanswered questions and next steps Description of the problem Methods needed to describe the range and types of home medication errors to target interventions Define high risk populations, if any – Many medications – Particular disease groups – SES, other demographic variables – Low health literacy One solution may be home visit studies Patient-centered communication 1/3 of parents can not accurately repeat back medication use instructions Patients who skip doses, stop taking medications, and experience side effects do not tell the doctor Primary care residency programs reassessing physician training, pilot testing new methods One solution: Need to refocus our outpatient time and infrastructure to ensure effective communication about home care Patient activation AAP parents guide to children’s medications “Ask your doctor to wash his/her hands” One solution is email One practice that used email had 1.2 emails per MD per day. 6% were urgent, and it was 57% faster for MD than phone Rosen P, Kwoh CK “Patient-Physician email: An opportunity to transform pediatric health care delivery. Pediatrics 2007; 120 (4): 701-706. Systems to support home care Pill boxes Calendars Web based systems Telephone based systems Support for organization and compliance Real time problem solving Take home points Even home medication errors are a systems problem There are several simple solutions to help prevent errors in the homes of your patients now Outpatient quality improvement just getting started Thanks!! Jerry Gurwitz Linda Sagor Bob Klugman Chris Stille Kathy Mazor Doug Roblin Naheed Usmani, Peter Newburger, Chris Kaucher,Hellen Mullen Katie Dodd and Kevin Chysna Terry Field Marianne Felice QUESTION & ANSWER SESSION Click on the Q&A button to submit your questions.