C4 & c5 spinal cord injuries - Stephanie Huff's ePortfolio
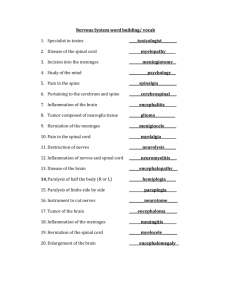
advertisement

DESCRIPTION AND DEFINITION “Spinal cord injury (SCI) is an insult to the spinal cord resulting in a change, either temporary or permanent, in the cord's normal motor, sensory, or autonomic function, damage to any part of the spinal cord or nerves at the end of the spinal canal — often causes permanent changes in strength, sensation and other body functions below the site of the injury (Mayo Clinic).” CHARACTERISTICS OF A C4 SCI Most severe of the spinal cord injury levels Paralysis in arms, hands, trunk and legs Patient may not be able to breathe on his or her own, cough, or control bowel or bladder movements. Ability to speak is sometimes impaired or reduced. When all four limbs are affected, this is called tetraplegia or quadriplegia. Requires complete assistance with activities of daily living, such as eating, dressing, bathing, and getting in or out of bed May be able to use powered wheelchairs with special controls to move around on their own Will not be able to drive a car on their own Requires 24-hour-a-day personal care(Shepherd Center) CHARACTERISTICS OF C5 SCI Person can raise his or her arms and bend elbows. Likely to have some or total paralysis of wrists, hands, trunk and legs Can speak and use diaphragm, but breathing will be weakened Will need assistance with most activities of daily living, but once in a power wheelchair, can move from one place to another independently(Shepherd Center) ETIOLOGY “Spinal cord injuries result from damage to the vertebrae, ligaments or disks of the spinal column or to the spinal cord itself. (Mayo Clinic).” Traumatic Spinal Cord Injuries •Motor vehicle accidents. Auto and motorcycle accidents are the leading cause of spinal cord injuries, accounting for more than 40 percent of new spinal cord injuries each year. •Falls. Spinal cord injury after age 65 is most often caused by a fall. Overall, falls cause more than one-quarter of spinal cord injuries. •Acts of violence. As many as 15 percent of spinal cord injuries result from violent encounters, often involving gunshot and knife wounds, according to the National Institute of Neurological Disorders and Stroke. •Sports and recreation injuries. Athletic activities, such as impact sports and diving in shallow water, cause about 8 percent of spinal cord injuries. •Alcohol. Alcohol use is a factor in about 1 out of every 4 spinal cord injuries (Mayo Clinic). INCIDENCE & PREVALENCE Incidence: It is estimated that the annual incidence of spinal cord injury (SCI), not including those who die at the scene of the accident, is approximately 40 cases per million population in the U. S. or approximately 12,000 new cases each year. Since there have not been any incidence studies of SCI in the U.S. since the 1990's it is not known if incidence has changed in recent years (NSCISC). Prevalence: The number of people in the United States who are alive in 2012 who have SCI has been estimated to be approximately 270,000 persons, with a range of 236,000 to 327,000 persons (NSCISC). SIGNS & SYMPTOMS Pain in the neck or back Weakness in the arms or leg Loss of bowel or bladder control Loss of sensation in the arms or legs Inability or reduced ability to regulate heart rate, blood pressure, sweating and hence body temperature. • Autonomic dysreflexia or abnormal increases in blood pressure, sweating, and other autonomic responses to pain or sensory disturbances (MedicineNet). SIGNS & SYMPTOMS CONTINUED •Pounding headache (caused by the elevation in blood pressure) •Goose Pimples •Sweating above the level of injury •Nasal Congestion •Slow Pulse •Blotching of the Skin •Restlessness •Hypertension (blood pressure greater than 200/100) •Flushed (reddened) face •Red blotches on the skin above level of spinal injury •Sweating above level of spinal injury •Nausea •Slow pulse (< 60 beats per minute) •Cold, clammy skin below level of spinal injury (NCSIA) COURSE AND PROGNOSIS “The prognosis for substantial recovery of neuromuscular function after SCI depends on whether the lesion is complete or incomplete. If there is no sensation or return of motor function below the level of lesion 24 to 48 hours after the injury in carefully assessed complete lesions, motor function is less likely to return. However, partial to full return of function to one spinal nerve root level below the fracture can be gained and may occur in the first 6 months after injury. In incomplete lesions, progressive return of motor function is possible, yet determining exactly how much and how quickly return will occur is difficult. The longer it takes for recovery to begin, often is less likely it is that it will occur (Early, 2013).” MEDICAL/SURGICAL MANAGEMENT “Medications may be used to manage some of the effects of spinal cord injury. These include medications to control pain and muscle spasticity, as well as medications that can improve bladder control, bowel control and sexual functioning. Immobilization should be done immediately following the traumatic event that caused injury; you may need traction to stabilize your spine, to bring the spine into proper alignment or both. Sometimes, traction is accomplished by securing metal braces, attached to weights or a body harness, to your skull to keep your head from moving (halo). In some cases, a rigid neck collar may work. A special bed also may help immobilize your body. Often, surgery is necessary to remove fragments of bones, foreign objects, herniated disks or fractured vertebrae that appear to be compressing the spine. Surgery may also be needed to stabilize the spine to prevent future pain or deformity (Mayo Clinic).” AUTONOMIC DYSREFLEXIA “Autonomic dysreflexia (AD), also known as hyperreflexia, refers to an over-active Autonomic Nervous System, which causes an abrupt onset of excessively high blood pressure. Persons at risk for this problem generally have injury levels above T-5. AD can develop suddenly and is potentially life threatening and is considered a medical emergency. If not treated promptly and correctly, it may lead to seizures, stroke, and even death (NSCIA).” AVOIDING AUTONOMIC DYSREFLEXIA •Apply frequent pressure relief in bed/chair •Avoid sun burn/scalds •Maintain a regular bowel program •A well balanced diet and adequate fluid intake •Compliance with medications •If you have an indwelling catheter, keep the tubing free of kinks, keep the drainage bags empty, check daily for grits (deposits) inside of the catheter •Perform routine skin assessments (NSCIA) OTHER PRECAUTIONS Due to lack of sensation thermal regulation is another function that can be disturbed after SCI. Poikilothermic, which is a complication occurring the first year after the injury where the body assumes the temperature of the external environment. This can lead to discomfort and the bodies’ ability to conserve body heat, which puts the body at risk for hypothermia. Extreme temperatures should be avoided and attention should be given to the extent and type of clothing worn by the client at all times (Atchison). The risk of Postural Hypotension and DVT should also be noted during OT therapy. Decreased blood pressure results in postural hypotension can be prevented by the use of antiembolism hosieries and abdominal binders, which externally assist circulation. Symptoms include lightheadedness, dizziness, pallor, sudden weakness, and unresponsiveness. Client should be semi reclined or reclined potion should be maintained until symptoms subside. Deep Vein Thrombosis causes embolisms and can be life threatening if not detected. Clients at most risk for this 2 weeks post injury, however it remains a concern in higher SCI’s due to extent of paralysis. Signs of DVT are swelling in the LE’s, localized redness, and a low-grade fever. AGE RANGE The risk of spinal cord injuries is at the highest between the ages of 16 and 30. Motor vehicle crashes are the leading cause of spinal cord injuries for people under 65, while falls cause most injuries in older adults (Mayo Clinic). DEPRESSION & SCI Depression can lead to feelings of hopelessness which can lead to thoughts of suicide; the risk for suicide in SCI clients is most in the first 5 years. “It involves major changes in mood, outlook, ambition, problem solving, activity level and bodily processes, such as sleep, energy and appetite”. Other risk factors associated with depression include drug and alcohol dependence, lack of a family support, access to weapons and a previous attempt at suicide. C4 & C5 spinal cord injuries can affect a person’s self-esteem and feelings of self worth because they have to depend on people around them for almost everything, this can also lead to anxiety and depression (Reeve Foundation). GENDER & GENETICS • “Spinal cord injuries affect a disproportionate amount of men. In fact, females account for only about 20 percent of traumatic spinal cord injuries in the United States (Mayo Clinic).” • “Genetic variation may partially underlie complex personality and physiological traits—such as impulsivity, risk taking and stress response—as well as a substantial proportion of vulnerability to addictive diseases (Kreek),” which can all be contributing factors to accidents that result in SCI. OCCUPATIONAL THERAPIST Educate client and their family on his or her condition, in this case SCI. During the initial stages of rehabilitation, OT practitioners will focus their treatment on regaining or maintaining the skills affected by the spinal cord injury, as well as maintaining and strengthening what muscle function the client has left. Educated and teaching their client’s on adaptive equipment that can make doing everyday tasks easier (Mayo Clinic). · Increasing independence in dressing, grooming, hygiene, feeding, and homemaking skills · Increasing the strength and function of your upper body and arms · Improving your thinking, visual, and perception skills · Evaluating and training in the safest method of bathroom transfers · Evaluating and training in computer skills (Rehab Team Site The rest of the treatment team include Physical Therapist, Psychologists, Recreational Therapist, Respiratory and Speech Therapist, Dietitian, Discharge Planner(Social Worker), Physician and Nurse. FRAMES OF REFERENCES • Biomechanical: Addresses the capacity for motion with specific relation to function; applying the mechanical principles of kinetics to movement of the human body and particular activities or functions ROM, Strength, Endurance -involved only if they believed the limitation in capacity affects the individual’s ability to do their occupations • Rehabilitative: To enable the client to participate fully in daily living, work, and leisure activities using compensatory methods, assistive devices, and environmental modifications • Injury prevention and control: To increase the probability of preventing SCI in the future, substantial evidence demonstrates the importance of understanding prevention • The Learning frame of reference: Used with an educative approach may be used to provide the teaching of new behaviors, information about and strategies of managing the symptoms of a disease or impairment • The Compensatory frame of Reference: allows for adjustments to be made to the way in which an activity is done, either through the method, materials or environment, to make certain that the occupation is completed by any possible means. When used with a rehabilitative approach, functioning is assessed and intervention modified as the condition progresses, and allows for the use of adaptive equipment to overcome the deficits the individual may have to increase wellbeing and independence MODEL OF PRACTICES Model of Human Occupation: Seeks to explain the complex interactions between person, activity or occupation and environment. Volition= motivation • Habituation= routines/customary • Personal Capacity=”ability for doing things” • Client-Centered: “We measure the effectiveness of person-centered services through the right blend of measures, indicators, and questions such as the Personal Outcome Measures (CQL).” Refers to understanding the client's desires and wishes for intervention and outcome • The Model of Rehabilitation : Patient centered, based on the best available evidence and aims to achieve consistency of practice, equity of access and sustainability of spinal cord injury services • The occupational adaptation practice: model emphasizes the creation of a therapeutic climate, the use of occupational activity, and the importance of relative mastery. Practice based on occupational adaptation differs from treatment that focuses on acquisition of functional skills because the practice model directs occupational therapy interventions toward the patient's internal processes and how such processes are facilitated to improve occupational functioning. The occupational adaptation practice model is holistic (Schultz).” • STANDARDIZED ASSESSMENTS Modified Ashworth Scale: Measures spasticity in patients with lesions of the Central Nervous System • Cost is FREE • http://www.rehabmeasures.org/PDF%20Library/Modified%20Ashworth%20Scale% 20Instructions.pdf • • Functional Independence Measure: “Provides a uniform system of measurement for disability based on the International Classification of Impairment, Disabilities and Handicaps; measures the level of a patient's disability and indicates how much assistance is required for the individual to carry out activities of daily living (Rehab Measures).” • Cost is not FREE • http://www.udsmr.org/WebModules/FIM/Fim_About.aspx • Spinal Cord Independence Measure :Assessment in overall ADL function • Cost is FREE • http://www.rehab.research.va.gov/jour/07/44/1/pdf/catzappend.pdf • Qualriplegia Index of Function: Assesses ADL's performed with the hands among non-ambulatory individuals with cervical SCI. • Cost is FREE • http://www.ncbi.nlm.nih.gov/pubmed/3960588 NONSTANDARIZED ASSESSMENTS Magnetic Resonance Imaging was judged to be the neuroimaging modality of choice for assessment of SCI because of its ability to define location of injury, degree of cord compression, as well as presence of hemorrhage, contusions or edema. • MRI-Diffusion Weighted Imaging is used to quantify the extent of axon loss after SCI. • Functional MRI shows the correlation between sensorimotor activities of persons with chronic SCI with imaging of metabolic activities of brain and spinal cord. • Magnetic Resonance Spectroscopy assess biochemical characteristics of the spinal cord after injury • COST RANGES • http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2722687/ • • MMT: Test of a person’s muscle strength, or ability of the muscle to move a part of the body against resistance. A doctor or therapist will assess muscle strength in individual muscles, and the results show which muscles are weak and the pattern of the weakness. • Cost is FREE • http://scottsevinsky.com/pt/mmt.html Mr. G, is a 30 yr. old Caucasian man who sustained a C5 complete SCI as a result of a MVA. As a result of his injury he is now tetraplegia with little functional movement. He is married with two young children and they live in the city in a one story brick house. He wife now assumes the role main homemaker and caregiver of their children. He assists where he can. He graduated from ITT with a master’s degree in computer software engineering. He was active before the accident with no prior health problems and a clean bill of health at his annual physical. Mr. G was referred to OT on the day of his injury and initially evaluated in ICU within 24 hours of injury. He was immobilized in cervical traction and his vital capacity stabilized after being on a ventilator for 24 hours, he also has compression garments on his legs to prevent DVT. He has no sensation in his LE, trunk, hands and wrist, as well as absence of elbow extension and pronation. He can assist in some ADL’s, communication and wheelchair mobility with supervision and setup but is total assist in all other aspects of life. Movements possible are shoulder flexion, abduction, and extension; elbow flexion and supination; scapular adduction and abduction. He has a weakened vital capacity due to paralysis of intercostals and may require assist to clear secretions. OT treatment objectives included (1) educating the client and family members of safety precautions and adaptive equipment that may be helpful (2) maintaining the movements in the UE’s that the client does have function of (3) achieving optimal independence in available musculature (4) achieving independent wheelchair mobility on all indoor and outdoor surfaces (5) receiving appropriate durable medical equipment (DME) to meet both short-and-long-term needs (e.g., manual and power wheelchair, cushion, and bathing and toileting equipment (6) returning to safe and accessible housing. Mr. G has had a difficult that accepting he has complete SCI. He could not imagine how his life was going to be okay now that he is a tetraplegic, his wife and children do give him some motivation and keep his life meaningful. He went to a psychologist once a week for a couple months to help him cope with his dysfunction and depression. On discharge, He is doing better although he still gets sad from time to time. He is happy that OT has helped him find ways to maintain working so he can still support his family and with the help of OT he can assist his wife in helping him in dressing, hygiene, grooming and self-feeding. He can also now get around using a wheelchair. ADL’S & IADL’S • C5: may require 24 hour caregiver assistance for activities of daily living, a person with an incomplete SCI or a generally strong person with a C5 may assist with some dressing, hygiene and grooming activities with the aid of assistive equipment. Feeding is generally possible with the use of adapted utensils and setup (Atchison). • C4 & C5: task such as household maintenance, meal preparation, shopping, cleaning, clothing care and safety procedures will require assistance with all of these activities…taking care of others is particularly difficult, of especially if the injured person was the primary caregiver for a child, spouse, or parent. A concurrent goal of OT may be activities, such as diapering a baby or bathing a child that can allow them to resume some premorbid roles. Often, many these previous responsibilities must be delegated to others, when this happens it is important that the person with the SCI retain the responsibility for the verbal directions of care. WORK & LEISURE • C4 & C5: With these levels of SCI, returning to work is usually not possible. However with proper high-tech devices, they could work from home if the resources are available. Volunteering for an organization may also add some extra meaning to the lives of a person with a SCI. Due to the fact that the age at risk of SCI’s is so young; returning to work may be an important client factor. Teaching your client ways of how they can still feel like they are providing for their families and increasing their self-esteem and self-image is important, this is where the high-tech devices come into play, and working from home can be made possible. • C5: at this level sensation of the UE is typically present, however diminished. Therefore a person may be able to participate in more of the leisure activities they had before the injury, just in adapted ways and exploring new leisure activities that are more geared toward their injury is an important key. EDUCATION & SOCIAL INTERACTION • C4 & C5: depending on the level of injury, secondary diagnosis, complications, availability of specialty hospital resources, people with SCI can generally resume educational activities, even while still inpatients in rehab facilities. Adaptive writing devices, page turners, recording devices, and computers play an intricate part in being able to resume educational pursuits after the injury (Atchison). Cognition will typically still be present; therefore being able to continue their educational pursuits can increase their outlook on life, especially if he or she is young. • C4 & C5: Social interaction and participation will be impacted in those with SCI, especially because as a result of the injury they may feel embarrassed and have deceased self-esteem in social situations. Family support and support groups, where they can identify with others is important. Community Mobility: with a strong C5 SCI, driving with assistive devices can be possible. For C4 or low C5 total assist with transportation is required, such as attendant-operated van or accessible public transportation. MOTOR SKILLS • C5: a person with this level of injury will have a few more movements than that of a C4 injury; however function is still greatly impaired. Due to the lower extremities being paralyzed and the upper extremities being weak, balance will still be impaired. Unlike with the C4 level injury, a person with this level can operate a manual wheelchair independently to some assist indoors, on noncarpeted, level surface and some to total assist outdoors. A power wheelchair can be operated independently. During d bed mobility some assist is require with a full electric hospital bed with Trendelenburg feature with patient controls is indicated. Postural support devices needed. Working on building strength in the UE is important, so that person can assist in some Areas of Occupations. Endurance and energy are going to be impacted much of the same way as in the C4 level SCI. PROCESS & COMMUNICATION SKILLS • C4 & C5: organizing space and objects to best benefit the person with the injury is important. Adapted equipment can be helpful in this as well as DE cluttering the main areas that the person will be using. In the case of C4, once they wake up from being on a vent, their temporal organization may be impacted as well as their energy level. Initially, ask them basic questions until they are more stable. Cognition is usually intact in SCI patients. • C4 & C5: Total Assist to independent depending on work station setup and equipment available (ex. Use of mouth stick, high-tech computer access, environmental control unit) Able to instruct in all aspects of care, even if they cannot physically do the task themselves. This can be important for maintaining some selfidentity and control. ROUTINES & ROLES • C4 & C5: due to the extent of the c4 and c5 SCI, routines previously followed will be impacted. Bathroom routines as well as self-feeding are impacted. When once the person could handle the routines of ADL’s, the paralysis caused by SCI will now require that they have total assistance in most of these areas. This is in part due to the loss of sensation, strength, balance, being bed ridden. These patients will have tubes for emptying the bowel and bladder. • C4 & C5: due to the extent of injury the client’s roles such as father, employee, and spouse are impacted. Learning to accept this can be difficult and often leads to depression. Being able to get back to functioning in the roles they once had is an important goal in OT intervention, although with these levels of SCI that can be a challenge. CLIENT FACTORS • Values, Beliefs, and Spirituality are impacted, when a SCI occurs a person’s whole world and view on their selves can change. It is important that they see the meaning and purpose of things beyond themselves. Important to keep motivation since all aspects of their lives are impacted. Body Structures will be weakened such as, sensory (due to paralysis), Neuromusculoskeletal (due to high level of injury), Cardiovascular(spinal shock), Voice and Speech(due to low endurance and energy and diaphragm strength), Skin(increased risk of ulcers) which is turn can impact the healing process and what function they have left. Body Structures are impacted such as, the spinal cord (where the injury is located), voice and speech, the heart and lungs, immune system, digestive, reproductive, bones and joint become weak from misuse, skin and sensory issues can occur due from lack of movement. GLOBAL & SPECIFIC MENTAL • Mental capacity is still intact, however depression and lack of motivation can arise in people with this level of SCI. Psychological state should be addressed. • In these levels of SCI, lack of sensation can lead to secondary disabling conditions and pain in places where some sensation is left, so safety should always be considered. Memory, mental capacity, cognition usually intact. Can remember how to function in task but due to injury physically being able to complete them is hard without assistance. ASSESTS AND WEAKNESSES • C4: neck flexion, extension, rotation; scapular elevation; inspiration • C5: shoulder flexion, abduction and extension; elbow flexion and supination; scapular adduction and abduction • C4: paralysis of trunk, UE, LE; inability to cough, endurance, and respiratory reserve low secondary to paralysis of intercostals. FIM: 28/assist=12 • C5: absence of elbow extension, pronation, all wrist and hand movement; total paralysis of trunk and LE. FIM: 41/assist=35 FUNCTIONAL PROBLEM Inability to self-feed (C5 Level) LONG TERM GOAL Client will improve in ability to self-feed using assistive devices by discharge date SHORT TERM GOAL 1 Client will use adaptive eating utensils with max trunk support twice a week for 2 weeks with mod fatigue, to increase level of independence during self-feeding. SHORT TERM GOAL 2 INTERVENTIONS Client simulate the act of bringing food to mouth using a adapted eating utensil with an extended handle and a universal cuff to aid in holding the utensil, once they have achieved needed ROM for doing this task, add food to utensils or try graded up the activity. Client will use adaptive eating utensils Client will use arm with max trunk support twice a day weights while doing for 1 month with min fatigue, to elbow flexion activities to increase level of independence during increase strength and self-feeding until discharge date. endurance while selffeeding (bringing hand to mouth). FUNCTIONAL PROBLEM LONG TERM GOAL Unable to participate in grooming activities Client will be able to participate in grooming activities with min assist (setup and supervision) in 4 weeks. SHORT TERM GOAL 1 Client will be able to brush teeth independently with mod assist using an extended handle and universal cuff with setup and supervision with max trunk support twice a day after 2 weeks. SHORT TERM GOAL 2 INTERVENTIONS Place 2 pound wrist weights on client and instruct them to bring arms to chest for 5 repetitions. Grade the activity as client’s strength improves, this is a purposeful activity that simulates the motion needed for brushing their teeth. Client will be able to comb hair independently with min Have client simulate doing jumping assist using an extended handle and universal cuff with jacks with max truck support and setup and supervision with max truck support once a day supervision to increase ROM in after 2 weeks. shoulders and elbows. DISCHARGE ●Patient activity level and functional status improve enough for safely being discharged from OT services or OT services are no longer helpful. ●The nature of the patient's current home and suitability for the patient's conditions (eg, presence of stairways, cleanliness) ●Availability of family or companion support ●Ability to obtain medications and services ●Availability of transportation from hospital to home and for follow-up visits with OT or other healthcare professionals ●Availability of services in the community to assist the patient with ongoing care ●Obtain and self-administer medications ●Perform self-care activities(with assistance) ●Eat an appropriate diet or otherwise manage nutritional needs ●Follow-up with designated providers and being discharged to another type of rehabilitation setting DICHARGE TO • Home • Skilled Nursing Facility(SNF) • Rehabilitation Clinic • Outpatient Therapy • Inpatient Rehabilitation REFERENCES Alper, E. (2014, May 15). Hospital discharge. Retrieved July 10, 2014, from http://www.uptodate.com/contents/hospital-discharge Brougham, R. (2011, March). Speech-language pathology treatment time during inpatient spinal cord injury rehabilitation: the SCIRehab project. Retrieved June 21, 2014, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3066498/ Atchison, B. J., & Dirette, D. K. (2012). Spinal Cord Injury. In Conditions in Occupational Therapy (4th ed., pp. 257281). Baltimore, MD: Lippincott Williams & Wilkens. CQL-The Council on Quality and Leadership. (2010). Principles and Practices in Person-Centered Services. Retrieved July 5, 2014, from http://www.thecouncil.org/assets/0/183/560769ec-ea26-48be-802e0c98f6c2d798.pdf Early, M. B. (2006). Spinal Cord Injury. In Physical dysfunction practice skills for the occupational therapy assistant (3rd ed., pp. 534-556). St. Louis, Mo: Mosby Elsevier. Johns Hopkins Medicine Health Library. (2014). Acute Spinal Cord Injury. Retrieved June 22, 2014, from http://www.hopkinsmedicine.org/healthlibrary/conditions/nervous_system_disorders/acute_spinal_cord_in jury_85,P00770/ Kreek, M. J. (2005, October 26). Genetic influences on impulsivity, risk taking, stress responsivity and vulnerability to drug abuse and addiction. Retrieved July 5, 2014, from www.nature.com/neuro/journal/v8/n11/full/nn1583.html Mayo Clinic Staff. (2014). Spinal cord injury Definition - Diseases and Conditions - Mayo Clinic. Retrieved July 5, 2014, from http://www.mayoclinic.org/diseases-conditions/spinal-cord-injury/basics/definition/con20023837 MedicineNet. (2014). Spinal Cord Injury: Treatments and Rehabilitation Symptoms, Causes, Treatment. Retrieved June 21, 2014, from http://www.medicinenet.com/spinal_cord_injury_treatments_and_rehabilitation/page3.htm#how_is_a_spin al_cord_injury_diagnosed National Spinal Cord Injury Statistical Center,. (2012, February). Spinal Cord Injury Facts and Figures at a Glance. Retrieved June 28, 2014, from https://www.nscisc.uab.edu/PublicDocuments/fact_figures_docs/Facts%202012%20Feb%20Final.pdf NSCIA. (2011). What is autonomic dysreflexia. Retrieved June 21, 2014, from http://www.spinalcord.org/resourcecenter/askus/index.php?pg=kb.page&id=1394 PMC. (2010, August). Outcome Measures in Spinal Cord Injury. Retrieved July 5, 2014, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2722687/#R10 Reeve Foundation. (2014). Depression-Spinal Cord Injury - Paralysis Resource Center. Retrieved July 5, 2014, from http://www.christopherreeve.org/site/c.mtKZKgMWKwG/b.5016279/k.1FD9/Depression.htm Rehab Team Site. (2009). Spinal cord injury rehab team. Retrieved July 5, 2014, from http://calder.med.miami.edu/pointis/sci-team.html Rehabilitation Institute of Chicago. (2010). Rehabilitation Measures database. Retrieved July 5, 2014, from http://www.rehabmeasures.org/default.aspx Rehabilitation Measure Database. (2014, May 28). Rehab Measures - Functional Independence Measure. Retrieved June 28, 2014, from http://www.rehabmeasures.org/Lists/RehabMeasures/DispForm.aspx?ID=889 Shepherd Center. (2014). Levels of Injury - Understanding Spinal Cord Injury. Retrieved July 5, 2014, from http://www.spinalinjury101.org/details/levels-of-injury Statewide Rehabilitation Clinical Network. (2012, February). Model of Rehabilitation for Spinal Cord Injury. Retrieved July 5, 2014, from http://www.sahealth.sa.gov.au/wps/wcm/connect/3d3af3804b32f7e386e0afe79043faf0/ Spinal+Cord+Injury+Rehabilitation+Model+of+Care.pdf?MOD=AJPERES&CACHEID=3d3af38 04b32f7e386e0afe79043faf0 Wong, S. L., Shem, K., & Crew, J. (2012). Specialized Respiratory Management for Acute Cervical Spinal Cord Injury. Retrieved July 5, 2014, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3584785/