a comparison of long-acting injectable medications for
advertisement

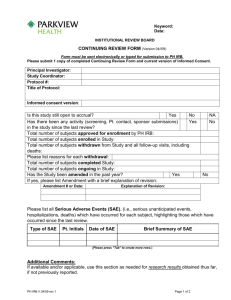
A COMPARISON OF LONG-ACTING INJECTABLE MEDICATIONS FOR SCHIZOPHRENIA (ACLAIMS) Coordinators Follow-Up and Final Visits Procedures Review Dial 1-919-962-2731 1 GO TO MEETING • We will pause between agenda items to take questions. • To ask a question enter it in the chat box on the right side of your screen • Select ‘organizer’ from the menu just below • Or you may ask on the phone line 2 Welcome & Introductions • Project Administrator—Columbia University -Alejandrina (Alex) Estevez • Data Coordinating Center—UNC Biostatistics -Project Management-Tania Wilkins -SAE/Endpoints Coordinator-Monica Miles -Clinical Monitor-Dianne Mattingly -Unblinded Statistician-Neepa Ray 3 SPECIFIC AIMS To compare the effectiveness, cost and tolerability of long-term treatment with haloperidol decanoate (HD) vs. paliperidone palmitate (PP) in patients with schizophrenia and schizoaffective disorder: 1. therapeutic effectiveness (as measured by time to efficacy failure) 2. cost-effectiveness over 24 months 3. incidence and severity of adverse events 4. enduring acceptability (as measured by time to all-cause treatment discontinuation) 4 TRIAL OVERVIEW • 311/360 randomized participants with schizophrenia or schizoaffective disorder • 22 sites in the US • Up to 24 months of treatment with LAI • Participants, treating clinicians, and raters are blinded to treatment assignment • 15-month recruitment period 5 ACLAIMS SITES 6 TODAY’S REVIEW • Primary Outcome Endpoint Monitoring and Reporting • Safety Monitoring and SAE Reporting • Final Study procedures: – Early RTDs Psychiatric Hospitalizations Lost to Follow-Up --Study Assignment Completion 7 TODAY’S REVIEW Cont. • DMS Reports – Follow-up Report – Expected and Keyed Forms Report – Safety Alerts – Queries • DMS • Statistical 8 Primary Outcome Endpoint • Efficacy Failure reflecting inadequate therapeutic benefit is the primary outcome measure • An Endpoints Adjudication Committee reviews outcomes of each study participant and makes the final determination • Site clinicians provide the narrative detail needed for these deliberations 9 PRIMARY OUTCOME: EFFICACY FAILURE Efficacy failure defined as any of the following: • Psychiatric hospitalization • Need for crisis stabilization • Clinician decision to discontinue assigned LAI due to inadequate therapeutic benefit • Need for adjunctive oral antipsychotic 10 OUTCOMES ADJUDICATION COMMITTEE • Panel of 3 research psychiatrists, independent of research team and blinded to treatment • Deliberations based largely on service use, concomitant medications, and reasons for study discontinuation • Event Narrative Form (ENF) is critical to endpoint classification process 11 DATA COLLECTION FORMS/TRIGGERS RELATED TO ENDPOINTS • Reason for Assigned Treatment Discontinuation Form (RTD) • Service Utilization and Resources Form for Monthly Items (SRF) • Adjunctive Medication Form (AMR) • Serious Adverse Events Form (SAE) • Adverse Events Form (AES) 12 ENF Event Triggers • All SAEs require an ENF • All psychiatric Emergency Room visits -unless the ER visit is directly associated with an SAE • All early RTDs -unless the RTD is directly associated with an SAE 13 ENF Triggers Cont. What other events do not trigger an ENF? • Non-Psychiatric Emergency Room Visits -Site PI may determine that an ENF is not necessary to document a potential endpoint if: -medical in nature (i.e. sprained ankle, flu, etc.) -at a time when there are no psychiatric symptoms exhibited -the medical condition did not in any way instigate psychiatric symptoms 14 ENF Triggers Cont. • Early Reason For Treatment Discontinuations (RTD) -after a psychiatric hospitalization -participant no longer willing to take study medication -participant lost to follow-up for > 90 days 15 EARLY RTDs • After a psychiatric hospitalization -every effort must be made to complete all assessments normally conducted at the last study visit -Record as the visit at which the study physician discontinued the study medication visit number will be the same as corresponding SAE -Date assigned study treatment stopped? this is the date the decision to discontinue treatment is made RTD form and QxQ 16 EARLY RTDs • Participant no longer willing to take study medication, but agrees to continue follow-up visits -every effort must be made to complete all assessments normally conducted at the last study visit -Record as the visit at which the study physician discontinued the study medication -Date assigned study treatment stopped? this is the date the decision to discontinue treatment is made • If the participant later decides to withdraw from the follow-up visits, the FWF is the only final form needed. RTD form and QxQ 17 EARLY RTDs • Participant Lost to Follow-Up > 90 days – RTD and FWF forms required -Record the visit number as the visit following the last visit by the participant while still on study medication -Date study treatment stopped 90 days after the last injection if no other information is available – ENF is required • if possible, note signs and symptoms relating to lost to follow-up 18 QUESTIONS? 19 SAFETY MONITORING DSMB Safety Action Plan • Central oversight of all clinically significant laboratory values • Post-baseline lab values that are clinically significant will be flagged for review and discussion between the site PI and the project Safety Officer to determine an appropriate plan, which may include discontinuation of study treatment • Prolactin-related monitoring in place 20 LABORATORY TEST ASSESSMENTS • • • • • • • Hematology Serum chemistries Fasting lipids Fasting blood glucose and insulin levels Urine screen for drugs of abuse Prolactin Serum pregnancy test for women who can become pregnant • Additional WBC’s when indicated 21 SAFETY ALERTS • Additional safety situations that warrant consultation with the Safety Officer - Hospitalization for any reason -Worsening tardive dyskinesia -Weight gain of 15 pounds or more -An increase in LDL cholesterol of 20mg/dL -New onset diabetes mellitus (FBS > 200) -significant clinical worsening as indicated by CGI score DMS has a Safety Alert Report for monitoring these situations Protocol v7.6 Section 7.2.10 22 ACLAIMS SAFETY OFFICER • Tom Smith, MD, Columbia University • Will review all SAEs to make sure they have information required by DSMB • If needed, will communicate with site physician to make specific requests • To be consulted in adverse safety situations about appropriateness for continuation on study medication if there is a desire to continue the medicine 23 PROJECT MEDICAL OFFICERS • Drs. McEvoy and Byerly • Address clinical and medication management questions • Develop laboratory monitoring plan for participants who have a history of leukopenia/ develop leukopenia during trial • Address protocol questions and violations 24 SERIOUSADVERSE EVENTS A serious AE is defined as one that satisfies any of the following criteria: • Results in Death • Is immediately life-threatening, including potentially life threatening suicidal behavior that results in hospitalization Any fatal or life threatening AE’s must be reported immediately Protocol v7.6, Section 5.1.1-4 25 SERIOUS ADVERSE EVENTS—cont. • A serious AE is defined as one that satisfies any on the following criteria: • Requires inpatient hospitalization or prolongation of existing hospitalization • Results in persistent or significant disability or incapacity • Is a congenital abnormality or birth defect • Is an important medical event that may jeopardize the subject or may require medical intervention to prevent one of the outcomes listed above. Protocol v7.6, Section 5.1.1-4 26 SERIOUS ADVERSE EVENTS • Per NIH guidelines: The trial period is defined from the time that the informed consent document is signed until 30 days after study withdrawal. Participants continuing in follow-up visits after early discontinuation from study drug must be monitored for SAEs and all SAEs reported. 27 SAE Procedures • All SAEs must be initially reported to the DCC within 24 hours after a site becomes aware of an occurrence. • Please note that an SAE is not considered reported until entered into the DMS. • Sites must report SAEs that are unanticipated and related to FDA within 10 days. (We will assist.) • Some site IRBs may require reporting of other adverse events or experiences that do not fit the description above. This additional reporting is the site’s responsibility (as is all IRB reporting), and is not part of study data collection. 28 Required SAE Information • • • • • • • Timing of SAE Primary diagnosis/description of event Diagnostic procedures (if any) Relationship according to the investigator Action taken for the SAE, e.g., stopping the drug, etc. Outcome of SAE Other Adverse Events: Only AEs related to the SAE should be mentioned. • Laboratory findings and Vital signs: Only those that are related to the SAE should be provided. 29 Steps for SAE Reporting 1. 2. 3. 4. 5. 6. 7. 8. Complete the SAE form with as much information as possible, following the instructions in SRM Chapter 8. The PI or study physician should sign all completed SAE forms. Assign the appropriate visit# and seq#. For the initial report, use SEQ number 101. For any later updates to the form for this SAE, use SEQ 102, 103 and so on. If a different SAE occurs on a participant at the same visit number, that Seq # series then begins with 201… Key the form into the DMS. Call the DCC Help Line 1-866-659-3064 to notify them of an SAE. The DCC and/or Alex will review the data and send out queries if needed. The DCC will notify and report the SAE to the Safety Officer. The Safety Officer may request additional information on the Event Any follow-up information that updates this event must be recorded on a new SAE form that is documented as follow-up with the next Seq # 30 DO NOT include in SAE reports: • Any identifying information, e.g.: – Patient's name or initials – Anything indicating geographic location or research site (such as names of hospitals or facilities, names of clinicians or study coordinators or any other identifiers) – Do not include participant study ID in note-log narrative – Place a participant ID label on paper copy narrative 31 QUESTIONS? 32 NARRATIVES—SAE & ENF • What’s the difference? – SAE narratives are needed to help IRBs and the DSMB understand the safety of the study treatments and procedures—the relationship between the SAE and the study medication is critical – ENF narratives are necessary to help our Adjudication Committee determine if an efficacy failure has occurred and thus require more information about symptoms and behaviors 33 ENF NARRATIVE GUIDELINE The following information about any event signifying a possible efficacy failure should always be provided: – Timing of Event – Description of Event including symptoms and behaviors – Circumstances surrounding event – Action taken (e.g., used oral medication, stopped LAI, none needed) – Outcome of event or relevant subsequent events Avoid Personal Health Information (PHI)/any identifying information Make sure dates in narrative correspond with dates on other forms Use the Clinician’s Check List on the ENF form to guide the narrative 34 NARRATIVES—SAE & ENF • Create all narratives in a word document and copy and paste into the note-log item. -ENF form: Item 4 -SAE form: Item 14 • The paper form is considered a source document: a study ID label should be placed and the narrative filed with the paper CRF • Simple corrections to paper note-logs may be done with a single-line cross through, initials and date 35 NARRATIVES cont. • Copy and paste the contents of the document into the DMS note-log by: -Open the narrative document and select “select all” from the Edit menu on the Windows Tool Bar. Then select “copy” from same menu -Minimize the document and then open the note-log for copying -Use the key combination “SHIFT + INSERT” to paste the document in the note-log -Save the note-log by using the key commands “ALT + S” 36 NOTE-LOG PROBLEM • What’s the problem? – The problem is that a user sometimes can’t save a changed form – The problem stems from an apostrophe (‘) or quote (“) copied from WORD and saved in a note-log from a previous session. – The DMS converts to boxes ( □ ) Note: the apostrophe or quote will look normal at first. It will only have the box look after the form has been saved and re-opened • What’s the solution? - The user can leave apostrophes/quotes out. After copying into the DMS add the apostrophes/quotes - The user can correct boxes as required. Note: The initial form will save with no problem. The problem only occurs when trying to change a previously saved form 37 QUESTIONS? 38 DMS REPORTS AND QUERIES 39 Statistical Queries • Statistical Queries are queries that are generated by our statisticians based upon a data retrieval • Statistical Queries are not generated by the DMS and not resolved through DMS query resolution • To resolve—click on remote data entry from the main DMS menu and select the participant, visit and form. • Open the form, resolve the query and Select save the form from the CHANGES menu 40