Hypertension Case Study: R.L., 45-Year-Old African American Man
advertisement
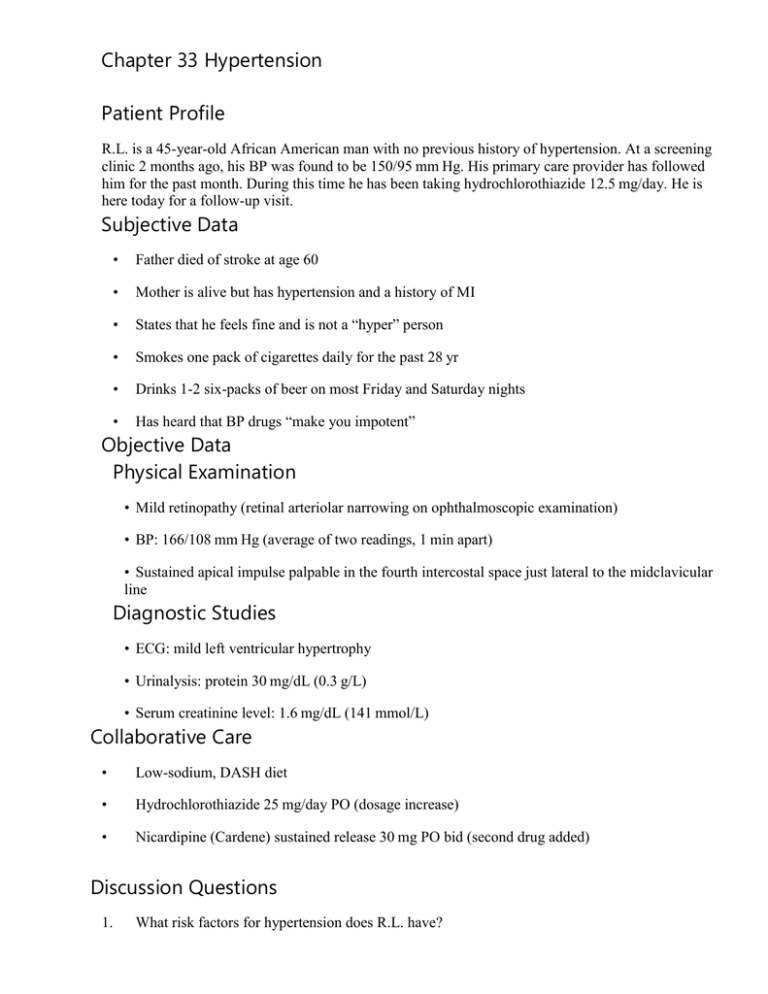
Chapter 33 Hypertension Patient Profile R.L. is a 45-year-old African American man with no previous history of hypertension. At a screening clinic 2 months ago, his BP was found to be 150/95 mm Hg. His primary care provider has followed him for the past month. During this time he has been taking hydrochlorothiazide 12.5 mg/day. He is here today for a follow-up visit. Subjective Data • Father died of stroke at age 60 • Mother is alive but has hypertension and a history of MI • States that he feels fine and is not a “hyper” person • Smokes one pack of cigarettes daily for the past 28 yr • Drinks 1-2 six-packs of beer on most Friday and Saturday nights • Has heard that BP drugs “make you impotent” Objective Data Physical Examination • Mild retinopathy (retinal arteriolar narrowing on ophthalmoscopic examination) • BP: 166/108 mm Hg (average of two readings, 1 min apart) • Sustained apical impulse palpable in the fourth intercostal space just lateral to the midclavicular line Diagnostic Studies • ECG: mild left ventricular hypertrophy • Urinalysis: protein 30 mg/dL (0.3 g/L) • Serum creatinine level: 1.6 mg/dL (141 mmol/L) Collaborative Care • Low-sodium, DASH diet • Hydrochlorothiazide 25 mg/day PO (dosage increase) • Nicardipine (Cardene) sustained release 30 mg PO bid (second drug added) Discussion Questions 1. What risk factors for hypertension does R.L. have? R.L.’s ethnicity and family history of hypertension are primary risk factors for hypertension. This is because African Americans develop hypertension at an earlier age, with increased severity and have a higher prevalence of stroke, heart disease, and chronic kidney disease compared with whites. His alcohol consumption, smoking, age, and gender are also risk factors for hypertension. 2. What evidence of target organ disease is present? Target organ disease is evident in the retina, as manifested by the early retinal changes (retinopathy); the heart, as manifested by mild left ventricular hypertrophy; and the kidneys, as manifested by proteinuria and a slightly elevated serum creatinine level. 3. What misconceptions about hypertension should be corrected? R.L. should be taught that hypertension is a “silent killer” because it usually does not cause symptoms. In addition, symptoms do not reliably indicate BP levels. Despite his absence of symptoms, organs throughout his body are being significantly damaged by the hypertension. He also needs to be informed that hypertension is not related to a “hyper” personality but, rather, is an elevation of BP. Not all antihypertensive medications cause sexual dysfunction, and it should be explained that if erectile dysfunction or decreased libido occurs, he should consult with his health care provider about changing drugs or dosages. 4. Priority Decision: Based on the assessment data, what are the priority nursing diagnoses and interventions? What are the collaborative problems? Nursing diagnoses: Ineffective self-health maintenance; ineffective renal perfusion; risk for decreased cardiac tissue perfusion; risk for ineffective cerebral tissue perfusion Nursing interventions: BP monitoring; evaluating effects of drug therapy, including presence of any side effects; patient teaching. R.L. needs detailed information on the following topics: Current BP measurement and his goal BP Instruction on home BP monitoring Dangers of uncontrolled hypertension and need for long-term control to limit further damage to heart, kidneys, and eyes and to reduce the risk for additional end-organ disease (e.g., stroke) Drug therapy: review action, dosage, and side effects of hydrochlorothiazide and nicardipine. Instruct R.L. to develop a regular and convenient schedule for taking the medication, not to discontinue the drug abruptly, not to double dose if a dose is missed, and not to change the dosage without consulting his health care provider. A second drug (a calcium channel blocker) has been added to R.L.’s regimen since his BP reflects stage 2 hypertension. Note: African Americans produce less renin and do not respond well to renin-inhibiting drugs. Lifestyle modifications necessary to control his BP, especially smoking cessation, limiting alcohol consumption to no more than 2 drinks per day, restricting sodium intake to 1500 mg per day, following a DASH diet, maintaining adequate potassium and calcium intake, engaging in at least 30 minutes of moderately intense aerobic activity on most days of the week, and maintaining or reducing weight, if appropriate. Resources for tobacco cessation coaching. Resources for DASH diet (diet history may be appropriate) Importance of regular follow-up with his primary care provider Collaborative problems: retinopathy, renal insufficiency, left ventricular failure 5. Evidence-Based Practice: R.L. wants to know the most effective nonpharmacologic strategies to lower his BP. What would you tell him? Explain to R.L. that the lifestyle modifications (discussed above) are the best nonpharmacologic strategies to help lower his BP and limit further target organ disease. Suggest behavioral interventions such as relaxation training, stress management courses, support groups, and exercise training if R. L. is not in acute psychologic distress