Asperger's Syndrome - University of Nebraska Medical Center
advertisement
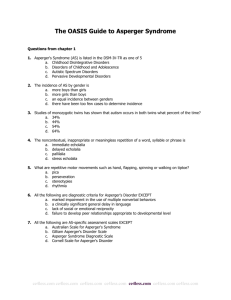
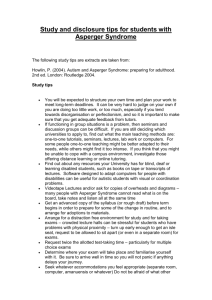
Asperger’s Syndrome: Assessment and Intervention in the Mental Health Setting By Ariadne V. Schemm, MA Pediatric Psychology Intern Munroe-Meyer Institute for Genetics and Rehabilitation University of Nebraska Medical Center April 5, 2006 History of Asperger’s Syndrome Hans Asperger and Leo Kanner first described similar forms of autism in the 1940’s Asperger’s description differed from Kanner’s in that speech was less delayed, motor deficits were more common, the onset was later, and it appeared to be most prevalent in boys Kanner’s work has defined recent views of autism, as a lack of responsiveness to other people and severe language impairments There was growing concern that the diagnosis of Autism could no longer be given to children who had developed fluent speech and an interest in socializing with others. The term “Asperger’s Syndrome” was first used by Dr. Lorna Wing in 1981. Current View Asperger’s Syndrome is now considered to be a less severe form of autism and a Pervasive Developmental Disorder The syndrome is also placed on the spectrum of autistic disorders and was recognized and provided with its own diagnostic criteria in 1994 in the DSM-IV (Attwood, 2000) Clinical Features Lack of empathy and perspective-taking Naïve, inappropriate, one-sided conversations Limited ability to form friendships Pedantic and repetitive speech Poor non-verbal communication Intense absorption in certain subjects (little professor) Clumsy movements and odd postures (Burgoine & Wing, 1983) Asperger’s Syndrome 299.80 Qualitative impairment in social interaction (at least 2): Marked impairment in the use of nonverbal behaviors Failure to develop peer relationships appropriate to developmental level Lack of shared interest with others Lack of social or emotional reciprocity Restricted repetitive and stereotyped patterns of behavior, interests, and activities (at least 2): Encompassing preoccupation with one or more patterns of interest Inflexible adherence to rituals, routines, and rules Repetitive motor movements Persistent occupation with object parts Disturbance causes clinically significant impairment in social, occupational, or other areas of functioning No clinically significant general delay in language, cognitive development, or adaptive behavior Criteria are not met for other PDD or Schizophrenia (APA, 2000) What it’s not: Children and adolescents with one of these characteristics do not meet the criteria for AS: Social akwardness or poor social skills Limited repertoire of interests Being described as a “weird kid” These children fall between the criteria“tweeners” Statistics Prevalence estimated at 20-25/10,000 More common in males Genetics seem to play a larger role in AS than in autism (Simon-Cohen, 2005) Neurologically Based Disorder Limited information on brain development differences in AS In autism, absolute increases in the total brain volume, total CNS tissue, and lateral ventricular volume Especially in temporal/parietal/occipital region Cerebrum Decrease in neuronal size Increased cell packing density in the limbic system Differentiating Asperger’s Syndrome from Related Disorders Autism Rett’s Disorder Asperger’s Syndrome Childhood Disintegrative Disorder Pervasive Developmental Disorder, NOS Disorder Similarities Differences Social Anxiety Fear/avoidance of social situations Child has capacity for age-appropriate relationships; anxiety is situation specific Mental Retardation Social & communication impairments; repetitive behaviors Impairments are quantitative rather than qualitative Speech Disordered Delayed/Absent language development Social intact; socially motivated; receptive language is higher ADHD Impaired social functioning; easily distracted Social quality better Distracted by anything Behavior Disordered Inappropriate behavior compared to peers; oppositional Socially motivated; socially aware Assessment Procedures Initial Interview Rating Scales Observations Direct Interactions Environmental Assessment Initial Interview Developmental History (age onset, milestones, delays) Medical History ( TBI, fragile X, ADHD, fetal alcohol) Previous Evaluations (medical, psych, genetic, GI) Presenting Concerns and Symptoms Severity of Symptoms (frequency, duration, intensity) Rating Scales Gilliam Asperger’s Disorder Scale Easily completed by parents Items are confounded across domains Provides a nice interpretation guide Word of caution-norm group, over-identification None are adequate to use independently in assessment All are best used as screening devices Consider having multiple raters across settings Direct Observation Interest is in observing behavior across the relevant domains Interest is in observations not just of target child behavior but also of environment Direct Observations Child-teacher interactions (child behavior and teacher behavior) Child-peer interactions (child behavior and peer behavior) Child-parent interactions (child behavior and parent behavior) Child-therapist interactions Child-Therapist Interactions Unstructured interview (school, home, friends, preferences) Assessing perceptions of social norms (Dewey) Perspective taking experiment (Frith) Direct Interactions Reinforcer Assessment Successful intervention requires motivation to learn the skill Generating motivation to learn requires functional reinforcers Identifying functional reinforcers can be difficult Function can change day-to-day and moment-tomoment Assess the Environment Do environments include demands that are within the capabilities of the child Is there direct teaching of social interactions? Is there limited social stimuli (noise, pace, crowd) Collaboration between home and school appropriate educational objectives Look also for environments that: Use primarily positive motivation strategies Prevent frequent errors and rely on prompting strategies Identify functional reinforcers Arrange consistency across settings and team members Treatment and Intervention Teach the acquisition of basic social interaction skills Teach the acquisition of adaptive skills Social Skill Training Social skills will need to be taught in an explicit, scripted, and rote fashion Skills taught may include: Appropriate nonverbal behavior Verbal decoding of other’s nonverbal behaviors Social awareness and perspective-taking skills (Klin & Volkmar, 1995) Behavioral therapy vs. Psychotherapy Individuals with AS have great difficulty with insight-oriented therapy Standard problem-solving techniques are not effective as the socially appropriate response is not socially meaningful to a child with AS More effective to script out appropriate reactions in problematic situations and practice. Prognosis Children with AS are more likely to become independently functioning adults than children with other forms of PDD Adults with AS often gravitate to professions that mirror their own areas of special interest They will continue to demonstrate difficulties in social interactions It is estimated that 30-50% of adults with AS are never correctly diagnosed (Bauer, 2006; Gillberg, Resources OASIS-Online Asperger Syndrome Information and Support www.aspergersyndrome.org/ Autism Society of Nebraska www.autismnebraska.org Asperger’s Syndrome- Parent Support Group: Cindy Roden, 334-9594 or Celeste Montoya, 891-6166 Munroe-Meyer Institute, Psychology Department: 559-6408 Questions and Comments? References Attwood, T. (2000). Asperger’s Syndrome. New York: Jessica Kingsley Publishers. American Psychiatric Association (2000). DSM-IV-TR. Arlington, Virgina: American Psychiatric Association. Baron-Cohen, S. (2000). Is Asperger’s Syndrome/ High-Functioning Autism necessarily a disability? Special Millenium Issue of Developmental and Psychopathology. Burgoine, E. & Wing, L. (1983). Identical triplets with Asperger’s Syndrome. Journal of Child Psychology and Psychiatry, 21, 303-313. Klin, A. & Volkmar, F. R. (1995). Asperger’s Syndrome: Guidelines for Assessment and Diagnosis. New Haven, Connecticut: Learning Disabilities Association of America.