The Nursing Diagnostic Process
advertisement

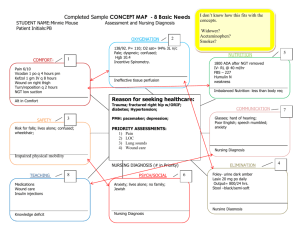
The Approach to the Medical Diagnosis for Nurse Practitioners: A Review of the Nursing Diagnostic Process and the Medical Diagnostic Process and how they differ Objectives This module has been designed to help the Student NP to understand the thinking processes behind the development of a nursing diagnosis and the development of a medical diagnosis. Upon completion the Student NP will be able to describe the key differences between the two processes and understand the appropriate application of each within NP practice. Outline This module will: • Review the steps of the Nursing Process and its link to the cognitive processes of developing a nursing diagnosis • Review the cognitive processes of developing a medical diagnosis • Compare the two processes • Give examples of each process • Show why the nursing diagnostic process should not be used to make a medical diagnosis • Provide a detailed “walk-through” of the medical diagnostic process • Make statements regarding the appropriate use of each process in NP Practice The Nursing Process has five stages Assessment Diagnosis Planning Implementation Evaluation The Nursing Diagnostic Process The Nursing Diagnostic Process follows the Nursing Process. It begins with an assessment and works towards a diagnosis. ▫ The nurse collects all data from the holistic assessment (subjective and objective), detects patterns and regularities, confirms the pattern with additional data and comes to a conclusion (diagnosis) about the patient. Pattern recognition is used to distinguish normal from abnormal patterns It looks like this: • • • • An observation is made Obtain subjective and objective data a pattern is recognized and a hypothesis is made More information is gathered to confirm the hypothesis • The pattern is confirmed = Diagnosis Metaphor: I search for as many puzzle pieces as possible. I begin to see a pattern emerge. I gather more pieces to allow me to confirm the pattern is true. The pattern is the Diagnosis. The Medical Diagnostic Process • The medical diagnosis begins with identifying the chief complaint or symptom. • The practitioner takes into account some key points about the patient and the context: usually age and gender. This gives the practitioner a context for the chief complaint. (Nurses do this, too.) • The practitioner comes up with about 3-5 ideas about the etiology of the chief complaint in consideration of the context of the patient. • These 3-5 ideas make up the differential diagnoses. • In a sense, the diagnosis comes first. However, it is just a hypothesis at this point and not a conclusion. • Note that Data Collection is only very preliminary at this point. Medical Diagnosis cont. Working from a differential list • After compiling a differential diagnosis list, the practitioner begins to gather subjective and objective data and, as he/she does so, the practitioner works to gather data to support or refute the 3-5 differentials. The practitioner is testing the hypothesis that one of these diagnoses may be correct. • The practitioner is able to do this by having a good understanding of the typical signs and symptoms of each possible diagnosis, and knowing what is common and uncommon for this patient’s demographics and risk factors. (Pattern recognition) It looks like this: •The green icon is the chief complaint. •The four hearts represent the DDx •The squares below the hearts are the data points that support that particular DDx. •The diagnosis favours the yellow heart hypothesis, and the orange heart hypothesis must also be kept in mind. Metaphor: It is a matching game where I match data pieces to pre-determined patterns . The biggest collection of matching pieces “wins.” An Example of the Medical Diagnostic Process • A chief complaint of unilateral ear pain in an otherwise healthy adult could be: Eustachian tube dysfunction (inner ear congestion), Acute Otitis Media, URTI Cerumen impaction. These are the differential diagnoses for a complaint of unilateral ear pain in the healthy adult. Subjective data: With the differential in mind, the practitioner will ask about: • Diving, air travel, trauma, recent URTI, fever, dizziness, nausea, hearing loss, drainage from ear, ringing in the ear, headache. Has he ever had this before? Does he have any allergies. [ Notice how each of these is a characteristic of one of the differential diagnoses and not “every possible” item of data. It is a focused data collection based on the Differential.] Findings: This patient denies all of these except for some hearing loss in that ear that has gradually worsened. He has had this before; ear was “plugged with ear wax.” He has a history of hay fever and environmental sensitivities that cause rhinitis and sneezing. He works as an accountant. The Evolution of the Differential Diagnosis (DDx) At this point, the DDx looks like this: Eustachian tube dysfunction –Possible (2˚to allergy) Acute Otitis Media –unlikely without URTI URTI -ruled out* Cerumen impaction -Possible Gradual onset hearing loss - Acoustic Neuroma?* *During the process data collection, some DDx may be removed entirely, some may be added due to new findings, and some will be weakly positive and others strongly positive Continuing the Data Collection, Working From The Differential List Objective Data: • On examination, the patient is found to have cerumen impaction in the affected ear canal. His neurological exam, in regards to the acoustic neuroma, is negative. He has no signs or symptoms of a URTI and no cervical adenopathy. • The differential now looks like this: Eustachian tube dysfunction – unlikely Acute Otitis Media -ruled out Cerumen impaction -positive Acoustic neuroma – unlikely but important to rule out. Arriving at a Diagnosis The diagnosis can now be stated: Dx: Cerumen impaction – unilateral, Rt. DDX: acoustic neuroma with unilateral hearing loss, eustation tube dysfunction. • The practitioner can commence with a treatment plan based on the working diagnosis (keeping the DDX in mind) Action: The impacted cerumen is removed with irrigation and curretage. The patient states he can hear normally now and the pain is almost gone. The TM is normal. (Reassessment) • The diagnosis is confirmed: Cerumen impaction. Comparing the Two Processes: A Review The Nursing Diagnostic Process -is like gathering as many pieces of a puzzle as possible and then arranging them into a pattern. The pattern identified is the diagnosis The strength of this model is that it works well for nursing diagnoses especially those that concern the whole person rather than the disease itself. The weakness of this model is that it may stop before the underlying etiology is found, and it may not take in to account other possibilities. It uses high-level critical thinking, reason and cognitive skills but not the scientific method of hypothesis-testing. The Medical Diagnostic Process Starts by having only one piece of a puzzle, and recognizing that that piece could be part of several possible etiologies or pictures. More puzzle pieces are gathered and matched according to the pictures under consideration. In the end, the pattern with the most matching pieces is the diagnosis. The weight of evidence will usually favour one hypothesis which then becomes the diagnosis The strength of this process is that all findings must be accounted for and remaining differentials are kept in mind even when the final diagnosis is made. It has this feature as a safeguard in case the first diagnosis is, in fact, wrong. This also allows for symptoms of red flag conditions to be ruled out or in to avoid catastrophe. The main weakness is that it is disease-oriented and is not the best method to approach personal and lifestyle issues. Key differences • While pattern recognition, high level reasoning, critical thinking and hypothesizing are utilized in both processes; The medical diagnostic process uses data to compare the best fit of sign or symptoms to hypothesized predetermined patterns. The pattern most heavily weighted by the evidence is the diagnosis. This is a deductive process; The nursing diagnostic process sums up data pieces into a pattern that can be confirmed by additional data. The pattern is confirmed and becomes the diagnosis. This is an inductive process. Another example Nursing diagnosis of a medical issue*: Assessment: Urine output is dropping. The nurse will gather more information by conducting a through head to toe assessment including vital signs, patient subjective experiences, colour and warmth of skin, sources of fluid loss, and history of intake, IV patency, knowledge about the patients current illness/condition. The nurse discovers that the patient is not eating or drinking well. The nurse investigates why the patient is not eating/drinking and finds that the patient is nauseated. Nursing Dx: Decreased urine output secondary to nausea as evidenced by decreased oral intake. *to illustrate that nursing models and medical models have unique uses and should not replace each other. Medical Diagnosis, same issue: Chief complaint: The urine output has dropped. Context: situation, age, comorbidities, history Differential diagnosis: dehydration, renal failure, decreased intake, increased output elsewhere. r/o hemorrhage and shock.* Data collected: Subjective: nausea; Objective: vital signs, peripheral perfusion, examination for sources of fluid loss/third spacing, Diagnostic tests: urine specific gravity, labs including CBC, lytes, BUN and Cr, stool for OB. *Note again how the data collection is connected to the differential diagnoses. It is not a random or general collection of data. Another example A patient comes in complaining of fatigue. The physical exam is negative. Lab reports (CBC and low ferritin) come back showing anemia. Nursing diagnosis: Fatigue secondary to anemia as evidenced by hgb of 80. Likely due to insufficient iron intake as evidenced by low ferritin. Medical diagnosis: fatigue and anemia DDX: hypothyroidism, chronic blood loss, pregnancy, iron-deficiency anemia. The nursing diagnosis may not adequately consider the many underlying causes of the anemia or lead one to consider serious diseases like cancer. The nursing diagnosis is still useful because it will lead to diet teaching regarding iron-rich foods which is still an appropriate nursing interventions. Let’s walk through another example of the Medical Diagnostic Process. The chief complaint is a cough. You know that the patient is a 18 months old boy. His immunizations are up to date, and the child has no allergies or chronic conditions. It is winter. His older brother has a cold. What do you do next? Construct a differential list. What are the top 5 differentials* in this case? 1) URTI 2) RSV Bronchioloitis 3) Asthma 4) GERD 5) Foreign body aspiration * Your list may be slightly different. That’s okay. Now what? 1) Collect subjective and objective data to rule in or rule out your potential diagnoses. 2) Assess the HEENT and chest and cardiac systems in this process. 3)But what are you looking for? Think about your differential list. ▫ ▫ ▫ ▫ ▫ 1) URTI 2) RSV Bronchiolitis 3) Asthma 4) GERD 5) Foreign body aspiration What are the disease patterns and symptoms and signs of each differential you are considering? • You know the symptoms of an URTI. • You know the pattern of RSV: runny nose, mild fever, cough, low O2 saturations, fine crackles bilaterally to chest. The cough is loose. • You know the pattern of Asthma: cough occurs when the airways are 50% constricted. It is often preceded by a URTI. The expiratory phase may be longer than normal. The cough may be dry or congested and can be paroxysmal. The cough is worse at night. • You know that GERD often presents with cough when supine and after meals. They may have had a lot of post-feeding regurgitation as a smaller infant. • You know that a sudden onset of cough and sometimes an inspiratory wheeze (stridor) are hallmarks of a foreign body aspiration. Your data collection finds the following subjective findings: The history: • Has had a runny nose ++ for three or four days. • Had a flu immunization one month ago. • Has not been eating very well and drinking poorly • Coughing day and night for 2 days; came on gradually and getting worse. • Had a mild fever on day 1. • Doesn’t want to lay down. • Sometimes a little blue around the lips. • No regurg history as a smaller baby. Refine your differential as you go along: What is your differential now? • RSV bronchiolitis – possible: Rhinitis, mild fever, cough, mild cyanosis reported • Asthma – possible, started with URTI symptoms, paroxysmal cough, mild cyanosis reported • GERD – unlikely, pattern not typical of GERD. • URTI – possible, has cold symptoms and cough and mild fever • Foreign body – ruled out for now: slow onset cough and URTI symptoms. Your physical exam finds: • • • • T 37.5, HR 148, RR 48 and moderately laboured O2 saturation 87%, slight peri-oral cyanosis. Hands and feet cool with cap refill 4 seconds. Chest has fine crackles bilaterally to entire posterior chest and RML. No wheezes or stridor heard. Expiratory phase normal. • Clear profuse rhinitis. • Prefers to sit on mother’s lap. • Decreased energy. What is your medical diagnosis? 1) RSV – Positive, all symptoms fit, time of year matches 2) Asthma – Unlikely: negative Hx of RAD 3) URTI – unlikely: viral URTI symptoms but breath sounds and hypoxia do not fit 4) GERD – rule out, child ill 5) Foreign body aspiration –ruled out 6) Bacterial pneumonia – positive findings: hypoxia, resp distress, unwell. Negative findings: pathologic breath sounds are bilateral and classic for RSV. Diagnosis: RSV bronchioloitis, hypoxia, dehydration DDX: bacterial pneumonia (supra-infection of viral RTI) Conclusion • Nursing and medical diagnostic processes differ. • Both processes are valuable. • Nursing diagnostic processes are excellent for patient-oriented, holistic care issues, and for guiding nursing care in all settings. • Medical diagnostic processes are efficient and effective for making medical diagnoses. • There is some overlap but one is not a substitute for the other; each has their unique purpose. Bibliography Baerheim A. (2001). The diagnostic process in general practice: has it a twophase structure? Family Practice, 18(3), 243–245. Retrieved from http://fampra.oxfordjournals.org/content/18/3/243.full Dunphy, L., Winland-Brown, J., Porter, B. & Thomas, D. (2007). Primary care: The art and science of advanced practice nursing (2nd ed.). Philadelphia: F.A. Davis Company. Godron, M. (1976). Nursing diagnoses and the diagnostic process. American Journal of Nursing, 76(8), 1298-1300. Retrieved from http://www.jstor.org/stable/3424002 Richardson, W., Wilson, M. & Guyatt, G. (2002). The process of diagnosis. Users’ Guides to the Medical Literature. Retrieved from http://medicine.ucsf.edu/education/resed/articles/jama6_the_process.pdf Robinson, D. (2002). Clinical decision making: A case study approach (2nd ed.). Philadelphia: Lippincott. Trochim, W. (2002). Research methods knowledge base: Deduction & induction. Retrieved from http://www.socialresearchmethods.net/kb/dedind.php Athabasca University Centre for Nursing and Health Studies MN:NP Program Author Donna Clare MN NP Jan 2012