Witness and narrator: Addressing problems
of secondary traumatic stress and
compassion fatigue in spoken language
interpreting
Dr. Emily Becher and Chris Mehus, MA, doctoral candidate
Who we are
• Couple and Family Therapists
• Work a lot with trauma
• We have each worked with interpreters
through our research
How we got here
• We observed a lot of variety within the
interpreters we have worked with
• We highly value and are grateful for
interpreters and the work you do
• We are still outsiders and still learning
Overview
• Defining secondary traumatic stress
• Research in this area
• What to do about it
– Prevention
– Intervention
Terminology
• Secondary traumatic stress
• Burnout
• Compassion satisfaction
Secondary traumatic stress
• Sometimes called compassion fatigue
• A little different than vicarious trauma
• Refers to the presence of symptoms
similar to PTSD resulting from indirect
exposure to traumatic material
Burnout
• Exhaustion
• Less satisfaction
• Can be unrelated to secondary
traumatic stress
Compassion Satisfaction
• Positive feelings related to work
• Feeling good about the difference you
make through your work
• Can protect against burnout
Secondary Traumatic Stress
•
•
•
•
•
Hypervigilance
Avoidance/ coping
Intrusive thoughts
Anger or irritability
Loss of empathy
•
•
•
•
Fearful or jumpy
Exhaustion
Social withdrawal
Emotionally down
or feeling numb
Secondary Traumatic Stress
• Symptoms might impact personal life
and/or professional life
Secondary Traumatic Stress
•
•
•
•
•
Hypervigilance
Avoidance/ coping
Intrusive thoughts
Anger or irritability
Loss of empathy
•
•
•
•
Fearful or jumpy
Exhaustion
Social withdrawal
Emotionally down
or feeling numb
Our brains protect us!
• This is all a result of our brains doing
what they are supposed to do
• Our brain learns to look out for things
that hurt us and then try to avoid them
Really abbreviated brain info
• Primitive brain: emotion and immediate
reaction (fight, flight, or freeze)
• Cognitive brain: logic and reasoning
Memories
•
•
•
•
Sensory information
Thoughts
Physiological changes
Emotions
Example
Think of a positive memory
Sensory
Thoughts
Sweet Smell
Sound of
Mixing
Emotions
Warmth from
Oven
Slow
Breath
Happy
I love
Sweets
Content
Singing
Physical
I’m
safe
Calm
Slow
HR
Muscles
Relax
Sensory
Thoughts
Sight of ___
Crying
Emotions
Smell of ___
Heart
racing
Scared
I’m
going to
die
Helpless
Loud noise
Physical
Police
aren’t
safe
Rage
Sweaty
palms
Muscles
Tense
Old and new memories
• Past experiences (or memory webs)
can get brought up
• New associations (or memory webs) are
created
Our brains protect us
• Making this connections is protective
• Symptoms of secondary traumatic
sense make more sense now
Secondary Traumatic Stress
•
•
•
•
•
Hypervigilance
Avoidance/ coping
Intrusive thoughts
Anger or irritability
Loss of empathy
•
•
•
•
Fearful or jumpy
Exhaustion
Social withdrawal
Emotionally down
or feeling numb
A metaphor
• Books in a cabinet
Research
Research: Background
• Increasing attention since 1995
• Recognition that professionals may face
direct and indirect exposure, as well as
having a personal trauma history
Research: Prevalence
• Some researchers have found similar
rates of secondary traumatic stress
across disciplines
• Although some may be at higher risk
(e.g., as many as 50% of child welfare
workers vs. 5-25% of trauma therapists)
Research: Risk Factors
• Personal history of psychological
trauma
• High levels of empathy
• Sharing a similar background with the
client
Research: Risk Factors
• Work environment and stress
– High demand and low control
– Workload
– Lack of support
• Working primarily with trauma-related
cases
Research: Risk Factors
• Possibly gender
• Interpreters convey traumatic content in
first person
• Interpreters are more likely to be from
the same community as the client
Protective Factors
• Supportive work environments
• Good self-care
• Debriefing or consultation
This will be covered more later today
Our Research
• Online survey with a measure of
secondary traumatic stress, compassion
satisfaction, and burnout
• Also asked open ended questions
• Interpreters across Minnesota
Our Research
• Before we share our results, what do
you expect?
– Levels of STS, CS, and burnout?
– What do you think people said in terms of
stress related to interpreting?
– Do you think your experience is similar to
the experiences of other interpreters?
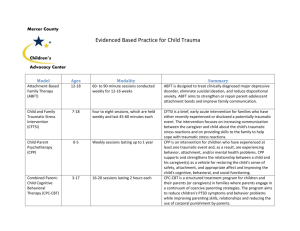
Our Study: Participants
•
•
•
•
N = 119
81 women, 36 men
24 reported refugee or asylee status
Age:
Our Study: Participants
• 30 languages represented in total,
most common:
– Spanish (25%)
– French (6%)
– Somali (6%)
– Hmong (5%)
Our Study: Participants
• Most commonly-reported highest level
of training was 40-hour training for
medical interpreters (41%), followed by
18% completing certificate or degree
Our Study: Participants
• Country of origin:
• Fields interpreted in:
United States
41
Mental Health
94
Mexico
13
Medical
109
Laos
8
Legal/Court
43
Somalia
7
Human Services
85
29 other countries
50
Other Gov.
47
Our Study: Findings
* CS: t = 9.94, d = .77
* ST: t = 4.48, d = 1.25
p < .017
Our Study: Findings
Our Study: Findings
• “Average” interpreter: high compassion
satisfaction and high secondary
traumatic stress with similar rates of
burnout to other helping professionals
• Some comments from participants who
reported high CS and high STS:
Our Study: Summary
• Compared to other helping professions, our
sample reported high STS, high CS, and
normal levels of burnout
• Some reported feeling supported and valued,
while other reported feeling disrespected,
exhausted, and in need of support
So what to do about it?
What to do - Prevention
• Psycho-education
– Signs and symptoms
• Professional Development & skills training
– Feeling competent and understanding your role
• Supervision and support
– Debriefing
Psycho-education
• Understand what STS is, the symptoms,
and what you are most likely to see
change in yourself
• Know you are not crazy
Secondary Traumatic Stress
•
•
•
•
•
Hypervigilance
Avoidance/ coping
Intrusive thoughts
Anger or irritability
Loss of empathy
•
•
•
•
Fearful or jumpy
Exhaustion
Social withdrawal
Emotionally down
or feeling numb
Psycho-education
• Really, you are not crazy
• Our brains try to protect us
• Teach your family about the possible
impact of your work and about STS
Professional Development
• Competence is protective
– Decreases stress
– Increases likelihood of compassion
satisfaction
• Know the bounds of your role
Professional Development
• Remember that you are integral to
patient care and a valuable member of
the human services community
• Create and validate this narrative
Supervision and Support
• Important to have people who can listen
and support you
• Who are those people for you?
• Confidentiality and debriefing
Example
You recently worked with a family and a
caseworker about reported child abuse. You
know of this family because they are part of
your community but you don’t personally know
them. Something about the child reminded you
of something from your past. You get through
the meeting but after it is over you feel
exhausted, numb, and detached from the world.
Example
• Talk with a few people about what
would be appropriate to share or not
share with a supervisor. How about with
a family member?
Example
You recently worked with a family and a
caseworker about reported child abuse. You
know of this family because they are part of
your community but you don’t personally know
them. Something about the child reminded you
of something from your past. You get through
the meeting but after it is over you feel
exhausted, numb, and detached from the world.
Practicing prevention
• Role-play debriefing with a peer while
maintaining confidentiality
Supervision and Support
• Helpful to have people who understand
your situation
– Validation that you aren’t crazy
– Prevents isolation
– Reminds you that your work is valuable
Workplace best practices
Nurses: Offer on-site counseling, support
groups for staff, de-briefing sessions, art
therapy, massage sessions, bereavement
interventions, and attention to spiritual
needs (Boyle, 2011)
Workplace best practices
Social workers:
• Organizational culture and values
• What does it mean to be a supportive organization?
Vacations, diverse case-load, opportunities for prof.
development, emphasis on self-care
• Environment is safe, comfortable and private
Workplace best practices
Social workers continued:
• Trauma specific-education
• Group support, social support within the organization,
spectrum of less formal to more formal structured debriefing, peer support groups
• Supervision and resources (Bell, Kulkarmi, & Dalton,
2013).
Workplace best practices
• Students:
• Same as previously discussed
• Addition of Empowerment
• Feeling in control, working towards
political/social change, feeling like you are
apart of proactive problem solving (Zurbriggen,
2011)
What does interpreter
empowerment look like?
Quick poll: How many people in the audience
have been in professional interpreting
situations and have observed unethical
professional behavior or behaviors that you
just felt were “not right”? Please raise your
hand.
What does interpreter
empowerment look like?
• Quick poll: Now, in those experiences, how
many of you felt that you knew who to report
that unethical or uncomfortable behavior to?
Or felt that reporting that behavior would
actually lead to a positive outcome? Please
raise your hand.
The empowered professional
• In the field of MFT
http://mn.gov/health-licensing-boards/marriage-and-family/public/complaints.jsp
Lawyers
Police officers: Must file a formal
complaint to the local agency that
employs the officer
For example:
http://www.ci.minneapolis.mn.us/police/
opcr-complaint
Personal best practices
• Self-care
• Stress-management
Small group discussion
Question 1: Are there strategies that your
organization could implement, or that
you could implement within your
organization that would decrease the
likelihood of secondary traumatic stress
and burnout for interpreters?
Small group discussion
• Question 2: What self-care or stress
management practices do you engage
in that help you cope with a difficult
interpreting session?
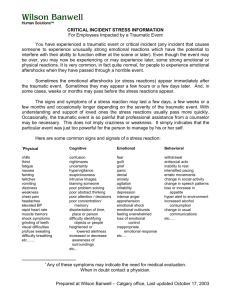
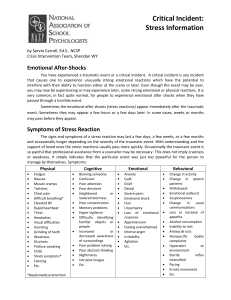
How do I know if there’s a
problem?
STS symptom list:
•
•
•
•
•
•
•
•
•
Feeling emotionally numb
Heart pounding when thinking about work with patients
Feeling like you’re reliving the trauma of your patients/clients
Trouble sleeping
Feeling discouraged about the future
Reminders of work upset you
Little interest in being around others
Feeling jumpy
Being less active than usual
How do I know if there’s a
problem?
•
•
•
•
•
•
•
•
Thinking about work with patients/clients when you didn’t intend to
Trouble concentrating
Avoiding people, places or things that remind you of work with patients
Disturbing dreams about work with patients
Wanting to avoid working with some patients
Easily annoyed
Expecting something bad to happen
Noticing gaps in memory about patient sessions (Bride et al., 2004)
Who should I go to?
•
•
•
•
•
•
Trusted mentor and peers
Medical doctor
Mental health professional
Spiritual advisor
Trusted supervisor
Family
What options are available to
get help?
• Depends on your level and duration of symptoms
• Low levels may be helped by decreasing/diversifying
work-load, sharing experiences with trusted person,
increasing stress management/ self-care
• Prolonged moderate to high levels may need
professional help
– Working 1 on 1 with a therapist
– Joining a psycho-education, support group
Can I still work if I’m
experiencing symptoms?
•
•
•
•
Typically a spectrum
Low level: Distress
Moderate level: Impairment
High level: Improper behavior
Definitions
• Distress “unresolved intense stress”,
“distracting”, “difficult to manage”.
• Impairment: “functionality of the
professional is compromised”.
• Improper behavior: dual relationships,
etc. (APA Advisory Committee on Colleague Assistance,2015)
Improper behavior and STS
Question: When you think of colleagues you
have known, can you identify a time when
you observed someone who perhaps was
experiencing Secondary Traumatic Stress
who also started seeming professionally
impaired and engaging in improper behavior?
Listen to your warning signs
• If you are distressed, experiencing
some symptoms, you most likely can
still work, but it is CRITICAL that you
address your symptoms head on and
implement a plan for action TODAY
When you could be
dangerous…
• If you fail to address the problem when you
are distressed, this most likely will lead to
impairment and eventually improper behavior
• If you are impaired or exhibit improper
behavior, you ethically should not be
practicing your profession
Practicing prevention
•
•
•
•
•
•
A body-scan exercise
Close your eyes, get comfortable
Breath deeply and slowly from your belly
Start with your head, notice how your head feels, is there any tightness,
pain, tension, stress? Pay attention to those feelings and breath.
Move slowly through the rest of your body. Paying attention to what you
are feeling and where and breathing, relaxing.
The goal is to notice where you are carrying stress from your day and
begin to address it.
Future plans
• Focus groups
• Maybe a psycho-education support
group?
• Other ideas?
Final thoughts?
Thank you!
Please contact us:
Emily Becher, 612-624-3335,
bech0079@umn.edu
Chris Mehus, 651-785-3660,
cjmehus@umn.edu
References
Advisory Committee on Colleague Assistance. (2015). The stress-distressimpairement continuum for psychologists. APA.
http://www.apapracticecentral.org/ce/self-care/colleague-assist.aspx
Bell, H., Kulkarmi, S., & Dalton, L. (2013). Organizational prevention of
vicarious prevention. Families in Society: The Journal of Contemporary
Social Services, 84(4), 463-470.
Boyle, D.A. (January 31st, 2011). Countering compassion fatigue: A
requisite nursing agenda. The Online Journal of Issues in Nursing,
16(1).
•
•
Killian, K.D. (2008). Helping till it hurts? A multimethod study of
compassion fatigue, burnout, and self-care in clinicians working with
trauma survivors. Traumatology: An International Journal, 14(2), 32-44.
Zurbrigen, E. L. (2011). Preventing secondary traumatization in the
undergraduate classroom: Lessons from theory and clinical practice.
Psychological Trauma: Theory, Research, Practice, and Policy, 3(3),
223-228.
©2014 Regents of the University of Minnesota. All rights reserved.
The University of Minnesota is an equal opportunity educator and employer.