PowerPoint Presentation - Medicine is an art
advertisement

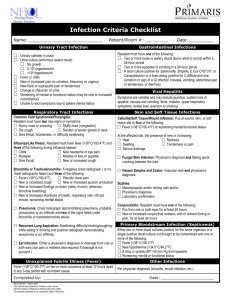
Presented By: Dr.Fatimah Al Dubisi Pediatric Infectious Diseases Head Infection control Follicular TonsillitisTonsillitis Pharyngitis Pharyngitis, Tonsillitis: Etiology Viral: Most Common, important agents : adenoviruses, coronaviruses, enteroviruses, rhinoviruses, respiratory syncytial virus [RSV], Epstein-Barr virus [EBV], herpes simplex virus [HSV], metapneumovirus) Bacterial : A β hemolytic Streptococcus Transmission: close contact, and occur most commonly in fall, winter, and spring. Clinical Manifestations: viral Onset: more gradual, symptoms often include rhinorrhea, cough, and diarrhea - A viral etiology may be also suggested by the presence of conjunctivitis, coryza, hoarseness, and cough. The The pharynx is red, and the tonsils will be enlarged if involved. Classically not covered with exudate. Clinical Manifestations Bacterial Streptococcal pharyngitis : uncommon before 2-3 years. Peak incidence : early school years, and declines in late adolescence and adulthood Onset often rapid, with prominent sore throat (odynophagia) and fever and chills in the absence of cough. referred otalgia, headache The pharynx is red, and the tonsils are enlarged and classically covered with a yellow, blood-tinged exudate, enlarged tender, cervical nodes - Can be followed by scarlet fever Epstein-Barr virus [EBV] Infectious mononucleosis syndrome Primary HSV infections Gingivostomatitis Primary HSV infections Primary HSV infections Enterovirus (Coxsackie virus) Herpangina Some specific viral Pharyngitis Patterns: Adenovirus (pharyngoconjunctival fever), concurrent conjunctivitis and fever Coxsackie virus(herpangina) small (1-2 mm) grayish vesicles and punched-out ulcers in the posterior pharynx EBV (infectious mononucleosis syndrome) prominent tonsillar enlargement with exudate, cervical lymphadenitis, hepatosplenomegaly, rash, and generalized fatigue Primary HSV (gingivostomatitis) in young children: high fever and oral ulcers F. necrophorum (Lemierre syndrome) serious complication, septic thrombophlebitis of the internal jugular veins with septic pulmonary emboli. Diagnosis: Clinical diagnosis. Strept pharyngitis: Culture ( Throat swab) Rabid test Treatment: Viral pharyngitis: supportive management Bacterial Pharyngitis: Treatment is mainly to prevent possible development acute rheumatic fever. 1- Medical,Antibiotics: 1st line: Penicillin ( V, Benzathine penicillin, amoxill) 2nd line: Macrolide ( erythromycin, Azithromycin ) Clindamycin 2- Tonsilectomy Complication of tonsillitis : Airway obstruction Peritonsillar Infection Retropharyngeal Space Infection Rhumatic fever Recurrent or Chronic Pharyngotonsillitis Otitis Media Peak incidence and prevalence of OM is during the 1st 2 years of life Most common reason for prescribing antimicrobial drugs Most common cause of hearing loss in children. propensity to become chronic and recur. It can be: - Suppurative ( acute otitis media, AOM ) or - Nnonsuppurative (secretory OM, or otitis media with effusion OME). Epidemiology: More below 2 years of age Incidence is greater in boys Tends to run in families More in Low Socioeconomic Status More with Formula Feeding Incidence increase with Exposure to Tobacco Smoking Increased incidence with congenital Anomalies ( cleft palate, craniofacial anomalies) Risk depends on Vaccination Status Etiology: Pathogens predominate: Streptococcus pneumoniae, nontypeable Haemophilus influenzae, and Moraxella catarrhalis Other less frequent pathogens Group A streptococcus, Staphylococcus aureus, and gram-negative organisms EXAMINATION OF THE EARDRUM: Normal Tympanic membrane Examination: Tympanic Membrane Findings: Findings can include: Erythema, loss of light reflex . Presence of liquid in the middle-ear cavity Opacity of the membrane Absence/impairment of memberane mobility. Perforations In sever cases: Retraction pockets and Cholesteatoma formation Treatment: Adequate analgesic medications (acetaminophen, ibuprofen) Pathogenic bacteria cause a large majority of cases, antibiotics is need in most of the cases Bronchiolitis Acute bronchiolitis It is a viral disease. RSV is responsible for >50% of cases Other agents: Parainfluenza ,influenza, and adenovirus. Older family members are a common source of infection Pathophysiology picture Pathophysiology: Bronchiolar inflammation, edema, mucus, and cellular debris This will lead to bronchial narrowing and obstruction Early distal air trapping and overinflation of the chest. Trapped distal air will be resorbed and the child will develop atelectasis Hypoxemia and hypercapnia can develop. Risk factors for bronchiolitis: Social history should include an environmental history, any smokers at home, number of siblings , daycare exposure, Prematurity Age <12 weeks. Underlying comorbidity : Cardiovascular, pulmonary, or immunologic diseases Clinical Manifestations: Usually preceded by exposure to an older contact with a minor respiratory syndrome within the previous week Infant 1st develops a mild upper respiratory tract Infection Diminished appetite and fever of 38.5-39°C Gradually, respiratory distress ensues Clinical Manifestations: Physical Examination: Signs of respiratory distress: Tachypnea, increased respiratory effort, nasal flaring, tracheal tugging, subcostal and intercostal retractions, and excessive use of accessory muscles. Wheezing Prolonged Expiratory time Auscultation :crackles or wheezes, with prolongation of the expiratory phase. - Diagnosis: - Mainly Clinical - Chest radiography can reveal hyperinflated lungs, Peri-Hailer ticking of the Bronchi and patchy atelectasis - Specific Viral study Treatment : - Mainstay of treatment is supportive: Oxygen, hydration, and suctioning of nasal and oral secretion CommunityAcquired Pneumonia Pneumonia: Inflammation of the parenchyma of the lungs Etiology: Streptococcus pneumoniae (pneumococcus) is the most common bacterial pathogen in children 3 wk to 4 yr of age, whereas Mycoplasma pneumoniae and Chlamydophila pneumoniae are the most frequent pathogens in children 5 yr and older. Clinical manifestations: Viral usually preceded by symptoms of an upper respiratory tract infection. Temperatures are generally lower in viral than in bacterial pneumonia. Tachypnea is the most consistent clinical manifestation. Increased work of breathing. Severe infection may be accompanied by cyanosis and respiratory fatigue. Auscultation of the chest: crackles, possible Bronchial breathing and wheezing, Clinical manifestations: Bacterial pneumonia in adults and older children typically begins suddenly with chill, high fever, cough, and chest pain. Physical findings: - Early : diminished breath sounds, scattered crackles over the affected lung field. - With the development of consolidation or complications such as effusion, empyema, dullness on percussion, lag in respiratory excursion, bronchial breathing are often occur. This classical presentation is rarely observed in infants and young children (Prodrome of URT symptoms followed by Sudden fever, prominent respiratory distress in addition to generalized non-specific signs and symptoms ) Diagnosis; Viral pneumonia; WBC count can be normal or elevated but is usuall not higher than 20,000/mm3, with a lymphocyte predominance Chest X Ray: hyperinflation with bilateral interstitial infiltrates and peribronchial cuffing Viral Pneumonia Xray : Bacterial Pneumonia: Eelevated WBC count, 15,000-40,000/mm3, and a predominance of granulocytes Chest X Ray: lobar consolidation, pleural effusion, empyema. Bacterial Pneumonia X Ray : Consolidation : Consolidation with pleural effusion : Patchy infiltrate Treatment: Well Patient : Out patient management; Antipyratic and Abx if required ( Amoxill or cephalosporin, Macrolide if Atypical Pneumonia is suspected ) Ill Patient: - Admission - Supportive mangament ( Oxygen, Hydarion) - Iv Abx ( Cephalosporin or Macrolide if Atypical Pneumonia is suspected ) Tuberculosis Picture of mycobacterium Etiology: Causative organism: Mycobacterium Tuberculosis Aerobes, non–spore-forming, nonmotile, pleomorphic, weakly gram-positive curved rods Slowly growing organism , takes 3-6 wk Definitions: Tuberculosis Disease: There are signs and symptoms or radiographic changes . Latent tuberculosis infection (LTBI) A reactive tuberculin skin test (TST) and the absence of clinical and radiographic manifestations. Definitions… Cont. Reactivation tuberculosis Rare in children, common among adolescents and young adults. There is infiltrate or cavity in the apex of the upper lobes. Pathophysiology of TB : Transmission; Airborne. Children with tuberculosis rarely infect other children or adults. Because: no. of Tubercle bacilli in their secretions is few only and cough is often absent or week that it lacks the force required to suspend infectious. Also absence of cavitary lesions ( adult Type TB, Opened TB) Children and adolescents with adult-type cavitary or endobronchial pulmonary tuberculosis can transmit the organism. The lung is the portal of entry in >98% of cases. The hilar lymph nodes usually are involved (The primary complex) (The primary complex) combination of a parenchymal pulmonary lesion and a corresponding lymph node site The parenchymal portion of the primary complex often heals completely by fibrosis or calcification after undergoing caseous necrosis and encapsulation Clinical manifestations of the 1st organism exposure ( primary infection): Majority of children with tuberculosis infection develop no signs or symptoms at any time Occasionally: low-grade fever and mild cough rarely marked by high fever, cough, malaise, and flulike symptoms that resolve within 1 wk. What happens after first exposure to the organism ? 1-Patient will have a Latent infection : infection under control, Normal CXRay: 2- Patient will have the Diseases Pulmonary TB - Silent with only Ghon’s complex( incidental finding chest xray) - Development of Local pathology: collapse-consolidation orsegmental lesion,Formation of fistula Local hyperinflation or emphysema Cont.. Primary Progressive TB; Bad progressive lung injury with sever manfistation clinically ( more in infant and immunecompromzed ) 2- Extrapulmonay (Lymphohematogenous spread): Disseminated Tuberculosis metastatic foci in many organs.( CNS,Cutaneous Disease,Bone and Joint Disease,Gastrointestinal Disease, Genitourinary Disease) 3- Reactivation of old Primary infection: When body immunity suppressed for any reason. Diagnosis: History: Possible exposure to an adult with or at high risk for infectious pulmonary tuberculosis is the most crucial risk factor for children. Tuberculin Skin Testing (Mantoux TST, PPD); - Delayed-type hypersensitivity (DTH) - The amount of induration in response to the test measured by a trained person 48-72 hr after administration. Treatment; General principle: Combination of drugs are used to effect a relatively rapid cure and prevent the emergence of secondary drug resistance during therapy The standard therapy of intrathoracic tuberculosis (pulmonary disease and/or hilar lymphadenopathy) 6 mo regimen of isoniazid and rifampin supplemented in the 1st 2 mo of treatment by pyrazinamide and ethambutol Prolonged treatment courses are need in CNS, bone, and joint infection. Prevention: Bacille Calmette-Guérin Vaccination (BCG) Strain of M. bovis Intradermal injection Life attenuated ( contra-indicated in immune compromised)