Diapositiva 1 - Semmelweis Egyetem
advertisement

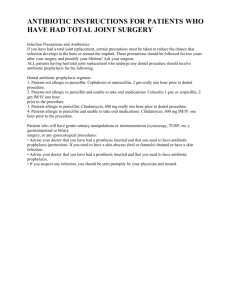
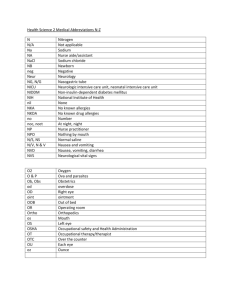
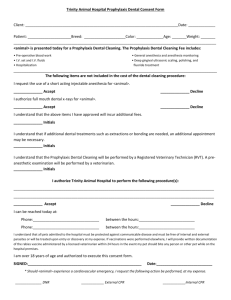
Oral Diagnostics Indication and contraindication of dental treatment relating to general health status Dr Bródy Andrea Semmelweis Egyetem Fogorvostudományi Kar Oralis Diagnosztikai Tanszék Factors for the assessment of general health status • The known health problems of the patient • Contraindications and risks caused by used medicines • Estimation of complications and risks, and planning the possibilities of prevention • Evaluation of the complaints and symptoms which refer to undiagnosed diseases – to improve chances for early diagnosis of a serious disease Is the information received always realistic? No! Because: • The patient had a bad experience earlier and doesn’t tell us the truth • Extenuate the earlier treatments or earlier used medicines • Is ashamed of the problem – e.g. alcohol abuse, or afraid of the consequences – e.g. drugs • Is unable to give us the right information • No explanation • Surprising motivation Risks relating to general health status The general health status could cause a risk for the • patient (e.g. Prosthetic valves, hemophilia), • environment and the health team (e.g. infective diseases) • for both (e.g. haemophiliac HIV positive patient). Medical problems influenced Treatment, used materials Oral health Dental treatment influenced Disease General health Contraindications relating with general health status Treatment is contraindicated in case of • Acute infective diseases • Patient in need of hospitalization • Mental disorders in need of sedatives • Severe allergic reaction to earlier dental treament with unknown origin Must find the solution! Patients with infectious diseases • Important to differentiate acute (influenza, herpes simplex, etc.) and chronic infections (HIV, HBV, HBC, TBC) • Acute infection – postpone the treatment if it is possible or choose conservative therapy Exception: pulpitis, periapical abscess • Take into consideration applied medicines for the basic disease. Patients with infectious diseases • The treatment may not be refused in the event of an infectious disease! • In most cases interaction with an HIV infected patient’s blood or excretion does not lead to infection. • Accepting attitude – more information • In case of an injury it is vital to find the serological status of the source of the infection. Types of exposure • Pierced or cut injuries with a contaminated instrument • Direct contact between mucosa or damaged skin with blood or excretions • Human bite • Laboratory infection Risks • The probability of HIV infection in the event of exposure is 0.3%. • In connection to HBV and a vulnerable patient it is 6-30%, to HCV 1.8% • Contact between a small amount of blood and intact skin does not carry risk. Treatment of a patient with an infectious disease • Should be called into the dentist’s surgery as the last patient • Mouth hygiene has increased significance, chlorhexidine mouth rinse • In the event of invasive treatment antibiotic prophylaxis may be necessary • Protective equipment should be worn – mask, glasses, gloves • Avoid the use of the turbine and ultrasonic depurator if possible • Disinfection must be performed as usual!!! Oral cavity symptoms of HIV viral infection Most common symptoms: • • • • • Oral candidosis (75% incidence) Hairy leukoplakia Herpes simplex, Herpes zoster Periodontal infections HIV gingivitis, necrotizans ulcerative gingivitis, necrotizans ulcerative periodontitis • Kaposi’s sarcoma Oral manifestations of human immunodeficiency virus • Photograph of the interior of the mouth of a person suffering from AIDS • Photograph of the interior of the mouth of a person suffering from AIDS Kaposi’s sarcoma Autoimmune diseases – Lupus Vulgaris • The buccal mucosa, hard palate, and vermilion border are the locations most frequently involved by lesions, which can be three types (discoid lesions, erythematosus lesions, and ulcers) Discoid erithematosus laesio Autoimmune diseases Sjögren syndrome •Dry mouth • Inflamed conjunctiva • Lymph node enlargement Cardiovascularis betegségek Cardiovascular diseases • High blood pressure, valve disorders, myocadial infarction, congestive heart disease, arithmia, angina • Warning symptoms: heavy breathing, high blood pressure, irregular pulse, periferic oedema, cyanosis, chest pain, gingiva hyperplasia, dry mouth • Alpha and Beta blockers, Ca channel blockers, diuretics Nifedipine induces gingiva hyperplasia 6 months after the end of the therapy Cardiovascular diseases – dental aspects Pacemaker Ultrasonic depurator, electrocauter and apex locator may not be used. Depuration with manual tools or possibly sonic depurator. Dental aspects • Stress reduction protocol, control of blood pressure • Patients with stable heart disease receiving atraumatic treatment under local anaesthesia can receive treatment in the dental surgery. • After myocadial infarction in the first year treat the patient with high attention • Cardiac events are most likely to occur in the early morning – patients with cardia disease should be treated in the late moring or afternoon • If it is necessary - anitimicrobial prophylaxis • Limiting the dosage of the tonogen Antibiotikus profilaxis Antibiotic prophylaxis • A bleeding related intervention often causes transien bacteraemia. • In the event of certain diseases as well as patients with neutropenia (neutrophil < 500/mm3) the patient should be treated with antibiotic prophylaxis. • Before the treatment chlorhexidine mouth rinse must be administered to avoid bacterial complications. • • • • • • • • Antibiotic prophylaxis recommended in the event of Congestive cardiac failure, stenosis Prosthetic valves Intra-, extracardiatic shunt, Diseases of the valves (stenosis, insufficiency) Endocarditis Dialysis, renal diseases, Prosthetic joints, Immundeficiencies Amoxicillin, Clindamycin, Erythromycin (UK National Institute completely removing the need for antibiotic prophylaxis in relation of dentistry) Inflammation • Epicenter: Chronic inflammation at a certain place in the body. Often comes without symptoms as a persistent state. • The epicentral inflammation can cause disseminated infections. • Periodontal pocket myocardial infarction, stroke, premature birth Immune compromised patient need high attention! ? • Extreme amount of plaque in an adult male patient Investigation of background disease is necessary! Candidiasis Haematological diseases – neutrophil system • Leukemia – the first symptoms show in the mouth (Oral manifestations are more common in acute leukaemias.) Not healing, plaque-covered ulcers, necrotisans ulcerative gingivitis, candida infection – early diagnosis may be life saving! Ulcer on the lingual mucosa Haematological diseases – haemorrhagic patient • Vasculopathies • Complications regarding the platelet system • Coagulopathies (inherited, obtained) Inherited: • Haemostasis disorders (intramuscular haematomes, GI bleeding) Obtained: • Heparins, Kumarins, Aspyrin Haematological diseases – haemorrhagic patient • Hemophilia-This is a genetic bleeding disorder that frequently has oral manifestations. • Spontaneous gingival bleeding may occur. Spontaneous bleeding may occur Haematological diseases – haemorrhagic patient • The physician has to aim to avoid invasive treatment of haemorrhagic patients • Anaesthesia, subgingival depuration, oral surgery treatment – factor substitution is necessary • Team work is important in the case of a haemorrhagic patient: dentist – haematologist, laboratory expert Tooth extraction may be performed without hospitalizing the patient! Malignant diseases • Radiotherapy • Chemotherapy • Steroids Immune compromised status Bisphosphonate treatment Bisphosphonates • Bisphosphonates are analogues of inorganic pyrophosphates,which are commonly used in the treatment of osteoporosis, metastatic osteolytic bone disease and primary resorptive malignancies of bone like multiple myeloma. (act on osteoclasts) Bisphosphonates • Patients with bone metastasis suffer jaw necrosis in 2.8% of the occassions (Aredia, Zometa, intravenal use) • One of the main risk factors of the development of necrosis is existing tooth or periodontal disease, not properly fitting removable denture, dental treatment • It was caused in most cases by tooth extraction and periodontitis Bisphosphonates • Suspension of the bisphosphonate treatment does not stop the progress • Due to the long half life time, even after the completion of the treatment the risk of BON (bisphosphonate induced osteonecrosis of jaw) is still present • Prevention: Prior to starting the treatment all dental problems must be eliminated, if possible permanent tooth substitutions should be inserted • Warning signs: erithema, ulcer, movable teeth Steroids • Long-term application will harm the operation of the immune system • They cause osteoporosis Transplant patients, autoimmune patients, patients with malignant tumor Eating disorders - bulimia • Acid erosion on the teeth, the angulus oris, enlarged salivary glands Additional risks • Diabetes mellitus – severe periodontitis and candidosis may draw attention - timing of meals must be paid attention • Pregnancy – increased care must be taken when prescribing medicine, x-ray examination may only be performed if absolutely necessary • Alcohol abuse, drugs Patient assignment and consultation with other professionals • Always consult the GP or the doctor treating the patient in the event of severe basic disease e.g. recent myocardial infarction, coagulopathies, immune deficient state • All documents must be filed and properly taken care of. Thank you for your attention! brody.andrea@gmail.com