Newborn Screening
advertisement

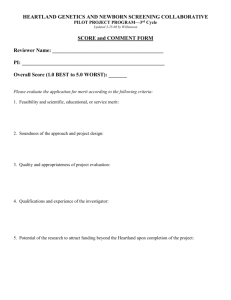
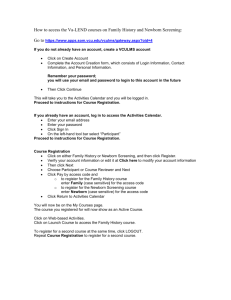
Expanded Newborn Screening: Public Health Policy and Clinical Impact Nutrition 526 October 26, 2011 Beth Ogata, MS, RD, CSP, bogata@uw.edu Cristine M Trahms, MS, RD, FADA Newborn Screening A state-mandated public health program that begins with a “heel poke” for every baby before hospital discharge First screen must be taken 24-48 hours of life regardless of feeding status or weight Blood Sample on Guthrie Filter Paper Card Who is screened? Washington State law requires that every newborn be tested prior to discharge from the hospital or within five days of age Second screen strongly recommended (between 7 and 14 days of age) Third screen recommended for sick and premature infants Why do newborn screening? Screen a presumably healthy newborn population Detect disease before symptoms present clinically Goal: Prevent or reduce morbidity and mortality Criteria for Newborn Screening Important condition Acceptable treatment available Facilities for diagnosis and treatment Difficult to recognize early Suitable screening test Natural history known Cost-effective to diagnose and treat Wilson & Jungner, 1968 Tandem Mass Spectrometry (MS/MS) High Impact and High Throughput One disease, one test is not cost-effective Many diseases, one test is cost-effective MS/MS allows for rapid, simultaneous analysis and detection of many disorders of amino acid, organic acid, and fatty acid metabolism Tandem Mass Spectrometer (MS/MS) MS/MS Methodology Blood spots punched (3/16th inch disc) Stable isotope internal standards added (deuterated) Butyl esters derivatives made Automatic injection into MS/MS via 96 well plates Sample set up determines which masses and therefore which compounds are detected 2 minute analysis time Automated data processing for results MS/MS Methodology – continued Compounds analyzed are amino acids and acylcarnitines Amino acids – to identify PKU, MSUD, homocystinuria Acylcarnitine – carnitine (vehicle) + fatty acid for identification of organic acidurias and fatty acid oxidation disorders MS/MS Plasma Acylcarnitines 100% C8 Intensity * C2 MCAD * * C6 * C10:1 * * C16 100% Control Intensity * C2 * * * * * * internal standards MS/MS Plasma Amino Acids What is the scope of newborn screening? Screen ~80,000 newborns Receive ~160,000 specimens Track ~3000 infants with abnormal results Prevent ~140 babies from death or disability For example: In WA State Which disorders should be identified? NBS mandates are under state control Some states screened for 3 diseases, others 40+ 2002 Maternal and Child Health Bureau commissioned ACMG Analyze literature Develop consensus on which disorders Recommend a core panel to create uniform NBS across all states Historical Harm (?) Early PKU screening led to cases of overrestriction and/or implementation of diet prior to confirmation of diagnosis Today, diagnosis is quite rapid 40 years ago, it took much longer so more potential for harm However, no published evidence of widespread physical/medical harm BUT the cases do underscore need for expertise and resources for management Amino Acid Disorders AA that are not used to make proteins are recycled by their specific metabolic pathways. Enzymatic deficiencies in these pathways lead to various clinical phenotypes. Diagnosed by plasma amino acids, urine amino acids, and/or urine organic acids (takes 2-5 days) PKU: severe, permanent ID MSUD: ID, hallucinations, ataxia HCY: connective tissue damage (joints, heart), ID, psychiatric disturbances CIT: risk of hyperammonemia ID, coma, death ASA: brittle hair, liver disease ID TYR I: acute or chronic liver disease, liver cancer, neurologic pain crises Organic Acid Disorders Organic acids are breakdown products of protein and fatty acid metabolism. Defects in their breakdown lead to (generally): Vomiting, metabolic acidosis, elevated ammonia in crises ID, motor delay, ataxia, cardiac/renal/pancreatic problems Diagnosed by urine organic acids and/or plasma acylcarnitines IVA: Isovaleric acidemia GA I: Glutaric acidemia type I HMG: 3-OH 3-CH3 glutaric aciduria MCD: Multiple carboxylase deficiency MUT: Methylmalonic acidemia (mutase deficiency) 3MCC: 3-Methylcrotonyl-CoA carboxylase deficiency Cbl A,B: Methylmalonic acidemia PROP: Propionic acidemia BKT: Beta-ketothiolase deficiency Fatty Acid Disorders Fatty acid disorders lead to impaired energy production Hypoglycemia, cardiomyopathy, muscle weakness can be seen Diagnosed by plasma acylcarnitines, and urine organic acids can be helpful MCAD: Medium-chain acyl-CoA dehydrogenase deficiency VLCAD: Very long-chain acyl-CoA dehydrogenase deficiency LCHAD: Long-chain L-3OH acyl-CoA dehydrogenase deficiency TFP: Trifunctional protein deficiency CUD: Carnitine uptake defect Who is identified? 1. Patients who need active management Symptomatic at diagnosis Strong evidence of pathology if untreated Examples: PKU, classic galactosemia, MSUD, PROP, etc. Who is identified? 2. Patients with disorders known to pose risk but reduced penetrance i.e., probably not everyone needs to be treated HPHE, MCAD Both are/have mild ends of the spectrum that have only been identified through NBS MCAD mutation c.199 C>T Never seen in patients picked up clinically Who is identified? 3. Patients who may not need any management Disorders considered extremely rare but seen in large numbers via NBS programs Reported cases have significant morbidity NBS pickups are mostly mild 3MCC, SCAD Biochemical phenotype Proceeding with Caution (Reasons to be Thoughtful) Proceeding with caution Not screening Core diseases vs. secondary targets / unintended targets What is reported vs. withheld? Will we pick up untreatable conditions? What is the impact of false positives on families? No long-term outcome data – consider research paradigm Consider infrastructure needed for follow-up What are we screening for? 9 OA 5 FAO 6 AA 3 Hb Pathies 6 Others CORE PANEL IVA GA I HMG MCD MUT 3MCC Cbl A,B PROP BKT MCAD VLCAD LCHAD TFP CUD PKU MSUD HCY CIT ASA TYR I Hb SS Hb S/ßTh Hb S/C CH BIOT CAH GALT HEAR CF How many infants does NBS identify? 2006 2007 Infants Diagnosed 2 1 Biotinidase deficiency 5 5 Congenital adrenal hypoplasia (CAH) 45 45 Congenital hypothyroidism (CH) 12 14 Cystic fibrosis 6 0 Galactosemia 1 0 Homocystinuria 0 0 Maple syrup urine disease 3 6 Medium chain acyl coA dehydrogenase (MCAD) def. 7 7 Phenylketonuria (PKU) 13 23 Sickle cell and other HG 95 112 TOTAL Emma 13 months old, healthy Normal pregnancy and delivery Normal eating pattern, no allergies or intolerances Feb 2008: Vomited 4-5 times throughout the weekend No fever Sleeping for extended periods – parents concerned, but previous fever had same pattern Parents gave Pedialyte Emma 4½ yo brother, parents sick on Sunday/Monday; same symptoms Monday night 9:30 checked on Emma Raspy breathing – thought respiratory problem but not worried Tuesday morning 11 am she was found motionless in her crib and pronounced dead at the scene Emma Autopsy revealed fatty changes to liver Coroner requested newborn screening blood spot be sent for acylcarnitine profile Diagnostic for very long chain acyl-co A dehydrogenase deficiency (VLCAD) VLCAD Disorder of long chain fatty acid breakdown C14, C14:1 C16, C18 Normal beta oxidation occurs in mitochondria Fatty Acid Oxidation http://www.genomeknowledge.org/figures/saturatedbetao.jpg VLCAD Presentations Hypertrophic cardiomyopathy, with hypoglycemia and skeletal myopathy, lethargy, failure to thrive Usually present birth to 5 months Hypoglycemia, hepatomegaly, muscle weakness without cardiac manifestations Late infancy – older childhood Muscle weakness/pain, rhabdomyolysis with exercise or illness. No hypoglycemia or cardiac Teens to adulthood VLCAD Treatment Diet low in long-chain fats (Portagen, Monogen = 87%, 90% of fats as MCT) Additional medium chain fats (MCT oil, walnut oil) Carnitine 100 mg/kg/day Avoidance of fasting Treating illness with IV glucose support VLCAD Diagnosis Newborn screening Plasma acylcarnitine profile Urine organic acids (should be normal) DNA sequencing Emma’s Family Family referred to genetics by coroner Parents requested testing for older brother (Zach) Acylcarnitine ordered DNA sequencing of ACADVL gene ordered Acylcarnitine – Zach (5 yo) C14:1 C14 C16 - nl C16:1- nl Zach Testing Reported: mild elevation of C14 and C14:1 with low free carnitine. VLCAD cannot be ruled out Recommend supplementing with carnitine and retest in 1 week DNA testing results back before AC repeat: Zach’s DNA testing reveals he is affected Family seen in clinic, started on treatment Zach – Clinical Picture 5 yo Healthy No symptoms of muscle weakness CPK = 315U/L (35-230) No hepatomegaly AST= 49 (5-41) ALT= 23 Bilirubin conj, unconj = normal (0.0, 0.4) No evidence of cardiac involvement Has had several viral illnesses in his lifetime without difficulty Once on carnitine, AC profile was classic for VLCAD Components of Newborn Screening Sampling hospital partnerships Screening State Lab Reporting to health care provider Referral to specialty care provider Short term follow-up diagnosis Long term follow-up ongoing treatment & monitoring Washington State Newborn Screening Birth Day 1 First Screen NL + ++ Primary Doctor Primary Care Doctor/ Biochem Clinic ASAP 2nd Sample DX NL TX + Primary Care Doctor Biochem Clinic Long term Follow up DX •Timely/urgent •Systematic process TX Long term Follow up Effective NBS requires a close working relationship between hospitals, newborn screening program, and follow-up program Informed Consent Supporting understanding for families Nutrition Involvement in NBS Policy Diagnostic/coordination Clinical Community Example: infant with galactosemia Symptoms in newborn, if untreated Vomiting, diarrhea Hyperbilirubinemia, hepatic dysfunction, hepatomegaly Renal tubular dysfunction Cataracts Encephalopathy E. coli septicemia result Death within 6 weeks, if untreated Also Duarte variant galactokinase deficiency uridine diphosphategalactose-4-epimerase deficiency Galactose-1-phosphate uridyl transferase (GALT) deficiency Example: infant with galactosemia Treatment: eliminate all galactose from diet Primary source is milk (lactose= galactose + glucose) Secondary sources are legumes Minor? sources are fruits and vegetables Food labels milk, casein, milk solids, lactose, whey, hydrolyzed protein, lactalbumin, lactostearin, caseinate Medications (lactose is often an inactive ingredient) Dietary supplements Artificial sweeteners Monitoring: galactose-1-phosphate levels <3-4 mg/dl Example: Infant with galactosemia POLICY CLINICAL MANAGEMENT RD participated on State Advisory Board to select disorders, including galactosemia RD provides nutrition care as member of the Biochemical Genetics Team: •Initiation of formula •Guidelines for monitoring intake •Plans for follow-up DIAGNOSIS & COOORDINATION “Presumptive positive” RD in contact with family and local providers to discuss appropriate feeding practices and arrange clinic appointment RD as case manager COMMUNITY RD at local health department provides ongoing education to family, local care providers Nutrition and NBS: Policy Screening process (disorders, procedures) RD participated in Advisory Board meetings, providing input about nutrition-related treatment Services and reimbursement Nutrition consultant to state CSHCN Program RD provides input about relevant state Medicaid policies Training and education RD provides information about management of metabolic disorders to local WIC agencies Nutrition and NBS: Clinical Management – PKU Phenylketonuria Phenylalanine hydroxylase Dihydropteridine reductase Biopterin synthetase Establish diagnosis Presumptive positive NBS results > 3 mg/dL, >24 hrs of age Differential diagnosis serum phe, nl tyr r/o DHPR, biopterin defects Current Treatment Guidelines With effective NBS, children are identified by 7 days of age Initiate treatment immediately Maintain phe levels 1-6 mg/dl (60-360 umol/L) Lifelong treatment Outcome Expectations With NBS and blood phenylalanine levels consistently in the treatment range Normal IQ and physical growth are expected With delayed diagnosis or consistently elevated blood levels IQ is diminished and physical growth is compromised Clinical Management: PKU Goals of Nutrition Therapy Normal growth rate Normal physical development Normal cognitive development Normal nutritional status Clinical Management: PKU Correct substrate imbalance Restrict phenylalanine intake to normalize plasma concentration Supply product of reaction Supplement tyrosine to maintain normal plasma tyrosine levels Phenylalanine -------------------//----------------------- Tyrosine (substrate) phenylalanine hydroxylase (product) Phe Levels from NBS to Tx Diagnostic levels Blood levels every 2 days because of rapid growth Equilibrium achieved by 14 days of age Adjustments necessary to maintain “safe” blood phe levels Usual intake of phe Newborn on formula 20 oz x 22 mg phe/oz = 440 mg phe 1 yo child on “regular” diet 30 g protein = 1500 mg phe (DRI = 13.5 g) 7 yo child on “regular” diet 50 g protein = 2500 mg phe (DRI = 19 g) Phenylalanine requirement 250 mg/d Management Tools Specialized formula provides 80-90% energy intake 85-90% protein intake tyrosine supplements no phenylalanine Phenylalanine to meet requirement from infant formula or foods Food Choices for PKU Effect of a single amino acid deficiency on growth Effective Blood Level Management in Childhood Blood levels once per month, or more frequently if needed for good management Age of Child 0-6 months 6 months 6-7 months 8-9 months 10-15 months 2-3 years 4-5 years PKU Management Guidelines Selfmanagement Skills 5-6 years 7-10 years 10-12 years 13-14 years 15-17 years 18 years Tasks for Children and Parents Parents learn about and adjust to PKU Start low-protein solid foods Introduce cup Introduce finger foods Consider weaning from bottle (discuss transition with clinic staff) Learn the concept of “formula first” Learn to distinguish “yes” and “no” foods Begin to learn to count foods – “how many” Begin to use scale – “how much” Assist in formula preparation Teach children how to deal with other children’s curiosity about PKU Prepare formula with decreasing supervision Choose after school snack Learn to pack school lunch Begin to list foods on food record Begin weighing food regularly on scale Begin to prepare and consume formula independently each day (with parental monitoring) Prepare simple entrees independently Know what blood levels are ideal Increasing self-monitoring (with continued parent support) in formula preparation and consumption Independently manage total phenylalanine intake for the day Learn menu planning Responsible for food records Responsible for all aspects of self-management Able to do ‘finger poke’ for blood test Able to explain basics of PKU – “What is it?” Responsible for remembering recent blood levels Continued parent support Transition to adult-based clinic care Ready to live independently, including: -formula preparation and consumption -food preparation and records -monthly serum phenylalanine levels Goal of Lifetime Management of PKU To maintain metabolic balance while providing adequate nutrients and energy for normal physical and intellectual growth Maternal PKU Concerns/Outcomes Women with PKU are at high risk for delivering a damaged infant Placenta concentrates phe 2-4x Microcephaly Cardiac problems Infant IQ directly related to maternal blood phe level Outcome improved with maternal blood phe <2 mg/dl prior to conception and during pregnancy Nutrition and NBS: Community PHN and interpreter make monthly visits to family of young child with MSUD. Through pre-arranged phone calls, we can discuss formula composition and preparation, and solid foods. This helps provide information between regular clinic visits. Nutrition and NBS: Community A woman with PKU is enrolled in the First Steps program (WA State MSS). The RD with PKU Clinic provides consultation to the First Steps RD, about management of amino acid levels. Metabolic Team Child Age-appropriate self-management skills Parents Monitoring health status, teaching, advocacy Nutritionist Nutrition therapy, feeding skills Geneticist Medical monitoring Social Worker Family support, counseling Lab Laboratory monitoring Medical Home Well child care, family support Psychologist Developmental monitoring, counseling PHN, others Family support in community School Educational programs, treatment monitoring Community Support of family and friends Therapists (OT, PT, SLP, etc.) Developmental monitoring, intervention NBS and the Community: Challenges Understand the implications of the results of newborn screening tests Develop a communication system between the community providers and the metabolic team for support of treatment Interact with PCPs and families as needed, to support appropriate MNT NBS and the Community: What you need to know Which disorders are identified by NBS in your state? Where do you find this information? What is the difference between screening and diagnostic results? What is the system for follow-up of presumptive positive NBS results? How do you make referrals to regional genetics clinics and specialty care clinics? Scenes from the Annals of Reporting and Acting on NBS Results A primary care physician telephones are reports there is a new baby with PKU and asks that you please start the infant on formula ASAP. What additional information do you need? What would you do? Scenes from the Annals of Reporting and Acting on NBS Results You are on-call for the weekend for your local hospital and you receive an order from the newborn nursery on an infant with presumptive galactosemia and a request for the initiation of treatment. What additional information do you need? What would you do? Summary NBS is the first part of a process of care that requires strong partnerships for optimal outcomes NBS outcomes are only as good as the follow-up provided Families should have access to the best treatment and care for their child Summary Specific diagnosis must be confirmed in coordination with the state Newborn Screening Program Careful monitoring of medical and nutritional status must be on-going by the metabolic team Nutritional intervention must be specific to the disorder specific to the child Additional Information Washington State Newborn Screening http://www.doh.wa.gov/ehsph/phl/newborn/default.htm National Newborn Screening and Genetics Resource Center http://genes-r-us.uthscsa.edu Star G-Screening, Technology, and Research in Genetics http://newbornscreening.info Building Block for Life (PNPG) Expanded NBS – 27(1) Genetics and Expanded NBS – 30(3) Nutrition Focus Overview nutr assessment of children with metabolic disorders – 24(5) Genetics – 22(6) Journal of Developmental and Behavioral Pediatrics Levy PA. An overview of newborn screening. 2010;31(7):622. Why do we do newborn screening? So Super Girl can be whoever she wants to be….