KARDİYOVASKÜLER RİSK DEVAMLILIĞI
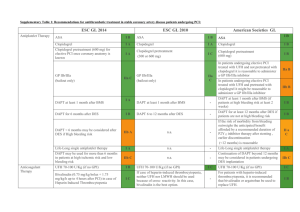
advertisement

Antiplatelet Therapy in General Overview Prof. Lale Tokgözoğlu MD, FACC, FESC Hacettepe University Faculty of Medicine Department of Cardiology Cause of Death by Gender in Europe: WHO 2008 Platelets are important in atherothrombosis After release from bone marrow, circulate for 7-10 days without interaction with vessel wall If exposed to subendothelium, platelets activated Plaque Fissure or Rupture Unstable plaques activate platelets Platelet Adhesion Platelet Activation Platelet Aggregation Thrombotic Occlusion Adhesion mediated by vWF, agonists like ADP, secreted granules and TXA2 cause aggregation, exposed GPIIbIIIa receptors crosslink with fibrinogen to form platelet aggregates 1 Adhesion 3 Aggregation 2 Activation Reproduced with permission from Cannon CP. Atherothrombosis slide compendium. Available at: www.theheart.org. THROMBUS FIBRIN THROMBOCYTE AGGREGATION THROMBOCYTE ADHESION ENDOTHELIUM MACROPHAGE SMOOTH MUSCLE CELL MONOCYTE Platelet surface membrane receptors play important role Platelets also important in stent thrombosis: Mechanism of AMI after stent implantation Relative frequency 12% Atherothrombosis at new location (after 27 months) 48% Restenosis (after 19 months) Stent thrombosis (after 9 months) 40% Alexopoulos D. Am Heart J 2010; 159: 439-445 Different mechanisms of antiplatelet drugs: 1. COX-1 inhibitors ASA, Omega 3 2. Phosphodiesterase inhibitors Dipyrdamole, Cilostazol 3. ADP-P2Y12 interaction blokers Ticlopidine, Clopidogrel, Prasugrel, Cangrelor, Ticagelor 4. GP IIb/IIIa blokers 5. Thrombin receptor antagonists Blocking different pathways for additional clinical benefit: Clopidogrel Prasugrel Cangrelor Heparin, hirudin Epinephrine Collagen ADP AA Aspirin TxA2 PLATELET GPIIb/IIIa Aggregation GP IIb/IIIa antagonists ASA Inactivates COX irreversibly blocking TXA2 formation (potent mediator of aggregation and vasoconstriction) Effective 15-30 minutes after oral administration Large dose over 10 gr eicosapentaenoic acid also blocks TXA2 Phosphodiesterase Inhibitors Dipyridamole stimulates PGI2 synthesis, blocks uptake of adenosine Clinical trials failed to show efficacy alone, enhances warfarin and ASA MR form useful for stroke prevention Cilostazol may be useful in claudicatio and has vasodilatory and antiplatelet effects Thienopyridines Bind to P2Y12 receptor inhibiting interaction with ADP that would result in activation and aggregation Prodrugs requiring transformation to active metabolites Ticlopidine dramatically changed interventional cardiology by making stent implantation safe 14 12 10 8 6 4 2 0 Prim. Cardiac EP Abrupt vessel closure Ticlo + ASA Schomig, NEJM 1996 Prim. Noncardiac EP UFH + Warfarin + ASA Bleeding Ticlopidine replaced by clopidogrel: more effective, safer 5 4 Ticlopidine Clopidogrel 3 2 1 0 MACE Bhatt, JACC 2002 Mortality Antiplatelet Resistance: Genetic polymorphism in platelet proteins (CYP2C19 reduced function alleles have 30 % decrease in active clopidogrel) Drug interaction (NSAID , drugs metabolized with Cytochrome P450 ) Environmental factors (Smoking, DM, HTN, HLP, ACS) VARIABILITY IN RESPONSE NOT ALWAYS RESISTANCE: Insufficent dosing, differences in assays and cutoffs, no gold standart Is Aspirin Resistance Clinically Significant? 326 stable CAD 5.2 % Aspirin resistance In HOPE study, @ 5 year follow up MI, stroke, death rate 1.8 % increased in the group with 11- deoxythromboxane B2 level ! Circulation 2002, 105: 1650 JACC 2003:41; 961 ASA resistance vs. clopidogrel resistance vs. dual resistance The prevalence of drug resistance: ASA 16%, CLOPI 15%, dual 9% The risk is 7x higher with dual resistence and 4.5x higher with multivessel PCI 40 37% 35 Percentage 30 26% No resistance 25 ASA resistance 20 CLOPI resistance 15 Dual resistance 10 5 0 Periprocedur.MI Eshtehardi P, Am Heart J 2010; 159: 891-898 Ischaemic events within 30 days Definition of Resistance Varies with Method Used: ASA Resistance Measured by PFA-100 and Aggregometry Stable AP n= 325 patients Partial response 23.8 % Routine assessment of platelet RESISTANT 5.5 %not 9.5 % aggregation recommended (II-B) 70.7 % Aspirin Sensitive Aggregometry Response to ADP and AA Gum P. Am J Cardiol 2001;88:230-235 90.5 % Aspirin Resistant PFA-100 600 mg clopidogrel loading is faster and more effective ! Aggregation inhibition (%) 0 *P=0.01 ** P=0.02 ‡ P=0.0008 20 40 ** * 60 ‡ Clopidogrel, 300 mg Clopidogrel, 600 mg 80 0 2 * ** 4 6 Hours Zidar F, et al. J Am Coll Cardiol. 2004;43(5, suppl A);Abstract 1100-1159. ARMYDA-II Circulation 2005;111:2099 Doubling loading and maintenance dose of clopidogrel in ACS patients undergoing PCI CV death, MI or stroke Clopidogrel standard 15% RRR Cumulative hazard 0.04 Clopidogrel double 0.03 0.02 HR 0.85 95% CI: 0.74-0.99 p=0.036 0.01 0.00 0 3 6 9 12 15 18 Days 21 24 27 30 Clopidogrel to Prasugrel Crossover Study: Less variability with prasugrel since it produces higher concentrations of active metabolite Healthy volunteers Crossover study IPA (20 µM ADP) 24 hours Platelet aggregation inhbition (%) 100 N=66 80 60 40 20 Clopidogrel effective 0 Clopidogrel resistant -20 Clopidogrel reply Prasugrel reply Brandt et al. J Am Coll Cardiol 2005;45(3 Suppl 1):87A – abstract 868-5 TRITON-TIMI 38: 13608 patients with ACS Prasugrel 60 mg LD/ 10 mg MD ASA UA/NSTEMI (TIMI Risk Score ≥ 3) & Planned PCI 12.0 month planned median R Double-blind treatment 6 - 15 months planned follow-up STEMI (Primary PCI ≤ 12 hours of symptoms or post-STEMI within 14 days) ASA 14.5 month actual median Clopidogrel 300 mg LD/ 75 mg MD = Primary efficacy end point: a composite of the rate of death from cardiovascular causes, nonfatal MI, or nonfatal stroke = Key secondary end points at 30 and 90 days included primary efficacy end point and a composite of the rate of death from cardiovascular causes, nonfatal MI, or UTVR Key safety end point: non-CABG related TIMI Major Bleeding Wiviott SD et al. New Engl J Med 2007;357:2001-2015; Wiviott SD et al. Am Heart J 2006;152:627-635 TRITON TIMI-38: Balance of efficacy and safety in patients < 75 Yrs, ≥ 60 kg, and without prior TIA/Stroke (N=10,804) 16 CV death, NF MI, or NF stroke 14 Endpoint (%) 12 Clopidogrel 11.0% HR 0.74 (95% CI: 0.66-0.84) p<0.001, NNT 37 10 8 Prasugrel 8.3% 6 4 HR 1.24 (95% CI: 0.91-1.69) p=0.17, NNH 222 2 TIMI major bleeding Prasugrel 1.9% Clopidogrel 1.5% 0 0 30 90 Wiviott SD et al. Circulation 2010;122:394-403 180 Days 270 360 450 Prevention of bleeding just as important as prevention of ischemia: Efficacy Safety In Clopidogrel group ,30 % of subjects had reduced function allele for CYP, these had 3X more stent thrombosis Genetic and Platelet Fx Tests are Complementary Genome Genetics Transcriptome Environment Proteome Phenotype Platelet function testing Variable Response to Clopidogrel Test: Genetic, platelet function Increase dose + Personalise + Easy - Complex - Efficacy, safety ? Alternative treatment: + Efficacy - Cost ? Bleeding ? Patients undergoing PCI with high platelet activity randomised to 75 mg C or 600 loading plus 150 mg C: GRAVITAS Study Primary end point End point High-dose clopidogrel (%) Standard-dose clopidogrel (%) HR (95% CI) p Cardiovascular death/MI/stent thrombosis 2.3 2.3 1.01 (0.58-1.76) 0.98 Outcome High-dose clopidogrel (%) Standard-dose clopidogrel (%) p GUSTO severe/moderate bleeding 1.4 2.3 0.10 Any GUSTO bleeding 12.0 10.2 0.18 Bleeding results Percentage of patients with persistently high platelet reactivity at 30 days Platelet reactivity units High-dose clopidogrel (%) Standard-dose clopidogrel (%) p >230 62 40 <0.001 AHA 2010 Cangrelor Potent inhibitor of ADP induced aggregation ATP analogue that inhibits P2Y12 by 100 % No renal/hepatic metabolism to be activated İv,rapid action, platelets back to normal in 60 minutes Has additive effects to clopidogrel Two short term trials discontinued for less than expected efficacy Ticagrelor Stable, high affinity inhibitor of ADP induced aggregation Oral agent acting directly on P2Y12 receptor without transformation Rapid and greater action Reversibility 180 mg loading ,90 mg bid Higher doses cause dyspnea and ventricular pause PLATO Study . Lancet. 2002;359:189-198 NEJM 2009; 361:1045 Glycoprotein IIb/IIIa Inhibitors Block the Common Final Pathway to Platelet Aggregation regardless of the stimulus for activation Glycoprotein IIb/IIIa Inhibitors Monoclonal Ab against IIb/IIIa: Abciximab Peptide antagonist: Eptifibatid Nonpeptide antagonist: Tirofiban GP IIb/IIIa Inhibitors in ACS: 30 day death / MI (N=31,402) Study PRISM Placebo Gp IIb/IIIa Odds Ratio 95% CI 7.1% 5.8%* 0.80 0.60-1.06 PRISM-PLUS 12.0% (*) 8.7% († ) 13.6%* 0.70 1.17 0.50-0.98 0.80-1.70 PARAGON-A 11.7% (l) (h) 10.3% 12.3% 0.87 1.06 0.58-1.29 0.72-1.55 PURSUIT 15.7% (l) (h) 13.4% 14.2% 0.83 0.89 0.70-0.99 0.79-1.00 PARAGON-B 11.4% 10.6% 0.92 0.77-1.09 GUSTO-IV 8.0% (24h) 8.2% (48h) 9.1% 1.02 1.15 0.83-1.24 0.94-1.39 Overall 11.8% -High risk 10.8%t - Diabetic 0 1.0 Gp IIb/IIIa iyi Boersma E, et al. Lancet. 2002;359:189-198. 0.91 0.85-0.98 2.0 Placebo iyi P=.015 - ASA use on admission PRISM-PLUS: Thrombus size 50 Probable 40 Odds Ratio: 0.77 P=0.022 Probable 30 Small Cumulative (%) 20 Small Medium Medium 10 Big 0 Occlusion Tirofiban + Heparin (n=608) Circulation. 1999;100:1609-1615. 24.1% 17.1% Big Occlusion Heparin (n=622) ACUITY, timing GP IIb/IIIa at the time of PCI vs. upstream in everyone Routine Upstream GP IIb/IIIa (N=4,605) Deferred PCI GP IIb/IIIa (N=4,602) 98.3% 55.7% Rand. to angio/interv (h) 6.2 6.2 Rand. to GP IIb/IIIa (h) 0.6 4.6 Net clinical benefit 11.7 11.7 Ischaemic EP 7.1 7.9 Bleeding EP 6.1 4.9 Overall exposure Stone GW et al. JAMA 2007;297:591-602 TARGET: Benefit of triple antiplatelet therapy 6 months death/MI Clopidogrel and tirofiban Clopidogrel and abciximab No clopidogrel only tirofiban No clopidogrel only abciximab 18 16 15.5% 14 12 10.9% Patients 10 (%) 8.4% 7.2% 8 6 4 2 0 0 30 60 90 Days Chan A, et al. J Am Coll Cardiol. 2003;42:1188-1195. 120 150 180 Major bleeding % Excess dose % Relation between age, dosing and bleeding Eur Heart J Suppl 2007, 9 (Suppl A) A23-A31. Age Antithrombotic treatment options in myocardial revascularisation: STEMI Classa Levelb ASA I B Clopidogrelc (with 600 mg loading dose as soon as possible) I C Prasugreld I B Ticagrelord I B Abciximab IIa A Eptifibatide IIa B Tirofiban IIb B Upstream GPIIb–IIIa antagonists III B Bivalirudin (monotherapy) I B UFH I C Antiplatelet therapy + GPIIb–IIIa antagonists (in patients with evidence of high intracoronary thrombus burden) Anticoagulation Fondaparinux III B a: Class of recommendation; b: Level of evidence; c: Primarily if more efficient antiplatelet agents are contraindicated; d: Depending on approval and availability. Direct comparison between prasugrel and ticagrelor is not available. Long term follow-up is awaited for both drugs Eur Heart J 2010. On line Antithrombotic treatment options in myocardial revascularisation: NSTE-ACS Classa Levelb ASA I C Clopidogrelc (with 600 mg loading dose as soon as possible) I C Clopidogrelc (for 9–12 months after PCI) I B Prasugreld IIa B Ticagrelord I B Abciximab (with DAPT) II B Tirofiban, Eptifibatide IIa B Upstream GPIIb–IIIa antagonists III B Antiplatelet therapy + GPIIb–IIIa antagonists (in patients with evidence of high intracoronary thrombus burden) a: Class of recommendation; b: Level of evidence; c: Primarily if more efficient antiplatelet agents are contraindicated; d: Depending on approval and availability. Direct comparison between prasugrel and ticagrelor is not available. Long term follow-up is awaited for both drugs Eur Heart J 2010. On line Antiplatelets for ischemic stroke or preventing systemic embolism Warfarin vs placebo Warfarin vs low dose Warfarin Warfarin vs ASA Warfarin vs ASA + clopidogrel 0 0.3 0.6 Warfarin better Camm, ESC 2009 0.9 1.2 1.5 1.8 2.0 Other better What is the ideal antiplatelet drug? Effective platelet inhibition without bleeding Uniformly effective in all patients (no resistance) Simple dosage No side effects No drug interactions Reasonable price FOR NOW: Beware of drug interactions and bleeding Keep ASA dose low in combination Calculate GPI dose meticulously New Horizons in Antiplatelet Therapy: - TRA thrombin receptor antagonists - Antagonists to A1 domain on vWF: ARC1779 - Collagen induced platelet aggregation blockers : CTRP-1 TRITON-TIMI 38: Therapeutic considerations for subgroups Age ≥75 years or weight <60 kg: Prasugrel 10 mg equivalent to clopidogrel (Prasugrel 5 mg under investigation) Majority of patients: Significant benefit with prasugrel 10 mg (MD) 16% 4% 80% Prior stroke/TIA: Prasugrel is contraindicated PRAGUE-8 (with 600 mg load): Patients undergoing elective PCI Percentage patients 20 Pre-treatment Clop 600 mg (n=155) No Pre-treatment Clop 600 mg (n=143) p=NS 15 11.9 p=0.006 10 8.4 7.1 p=NS 5 2.8 1.3 0.7 0 D/MI/CVA/UTVR Widimsky P et al. Eur Heart J 2008;29:1495-1503 Troponin >3XULN Major + Minor Bleeding Activated platelets express CD 40L triggering inflammation and thrombosis ISAR-CHOICE Circulation 2005;112:2946 30th DAY DEATH / MI WITH GPI 18 Placebo 16.7 GP IIb-IIIa Inhibitor 14.1 14 11.6 10.9 9 10 % Parients 10.2 10.1 5.9 4.8 6 3.6 3.9 1.8 2 0 EPIC CAPTURE EPILOG EPISTENT PRISM-PLUS PURSUIT JUMBO - TIMI 26 (Phase II) PCI + Stent (n= 904) ASA 325 + % 70 GP2b/3a Clopidogrel Klopidogrel Prasugrel 300/75 40/7.5 60/10 60/15 2 9,4 10 1,7 % % 7,2 1,2 1 5 0 0 Major, minor bleeding Circulation 2005;111:3366 MACE Variable Clopidogrel Response At 5 Days UA Patients* (n = 32) Nonresponders 22% Responders 47% Low responders 32% *Received an oral loading dose of 300 mg of clopidogrel followed by 75 mg daily. Gurbel PA, et al. Circulation. 2003;107(23):2908-2913; Lau WC, et al. Circulation. 2004;109(2):166-171.