Applicator - Research - Vanderbilt University
advertisement

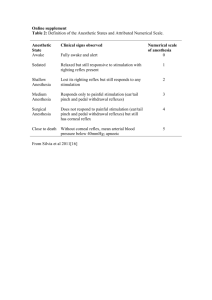
Non-Transcranial Electroanesthesia Device Group 2: Ryan Demeter 1, Matt Jackson1, Caroline Schulman1, Matt Whitfield1 Advisors: James Berry, M.D. 2, Paul King, Ph.D.1; 1 Department of Biomedical Engineering, Vanderbilt University, Nashville, TN 2 Vanderbilt University Medical Center Anesthesiology Multi-Specialties Division, Nashville, TN Transcranial Products Problem Statement The goal of this design project is to develop a device to control and administer non-transcranial electroanesthesia using the vagal nerve. The device will be portable, self sustaining, and rechargeable.. The exact parameters for stimulation will be variable allowing the device to be adaptable to altered stimulation parameters determined with any future research. The electrical pulses required for the electroanesthesia will be generated by the computer’s soundcard and then output from the sound jack to an external amplification circuit. This circuit will amplify the signal to the desired voltage and a set of electrodes will deliver the signal to the surface of the skin. This project assumes that non-transcranial electroanesthesia is possible. The device was designed based on the best understanding of both current electroanesthesia and vagal nerve stimulation. Further research into the actual application of vagal nerve stimulation to achieve electroanesthesia will be addressed in a later project. Site of Application Our Design 2 electrodes on the forehead, 2 electrodes on the back of the head 1 electrode over the right vagus, 1 electrode over the left vagus Applicator Multiple pad electrodes 2 pad or 2 needle electrodes Stimulus Production Electrical Soundcard Output Parameters 35 V, 4 mA, 100 Hz, rectangular pulse Power Rechargeable Battery 25 V, 50 uA, 20 Hz, rectangular pulse (250 us) Rechargeable Battery Pricing $1500-$3000 $1500 Budget Box and mountings ($214.15) • Case (Dimensions: 18" x 18" x 10") ($124.12) • Foam Padding (VU BME Donated) • Keyboard Hand Rest ($8.75) • Hardware Mounting ($81.37) Circuit and Supplies ($155.78) • 2 Fans ($18.00) • 3 Amplifiers ($45) • Supplies from Radio Shack ($92.78) Applicator ($0) • Pad Electrode (VU BME Donated) • Needle Electrode (VUMC borrowed) Computer ($0, VUMC Loaned) • 1.6 GHz • 1 GB Hard drive Miscellaneous ($130) Theory Behind Electroanesthesia Total Budget =$500 •Quicker recovery time and fewer biological effects than gas and intravenous anesthesia (Photiades, 218225). Patent Search •Patients heal better and are less affected by the process. •No patents involving non-transcranial electroanesthesia. •Less buildup of naturally produced gases in the body. •Little neural tissue change in mammalian studies. •A patent was found (4383522, 1983) that describes a transcranial method of delivering electroanesthesia using electrodes placed on the neck and the forehead. •Little change in potassium and sodium concentration levels in extracellular and intracellular fluids of the brain. These electrolytes are important to the function of many systems, homeostasis, and iron regulation in the body and play a role in nerve stimulation. •With this method, electric pulses are used in conjunction with muscle relaxants, nitrous oxide and oxygen to produce anesthesia. • Another patent (6,393,319, 2002) involves using prerecorded wave forms to generate electric pulses for therapeutic purposes. •Decreased gastric acid secretion leading to less of a chance for stomach ulcers seen with other anesthesia (Sances and Larson, 33-46). •Our device differs from the above by allowing for dynamic control of the output signal. Design Specifications Theory Behind Vagal Nerve Stimulation LabVIEW virtual instrument •Pain can be controlled by electrical stimulation of the vagal nerves (Kirchner et al., Ness et al.). •The ON/OFF button turns the signal generation on or off but does not close the program. •Vagal nerves lead into the brain and allow for the control of pain without passing current through the brain. •There are dials to control pulse duration, amplitude, and frequency of the output signal. Normal nerve reaction to a stimulus •Pain control is possible via clips on the earlobes (Cork et al 2004). Gain Stage “Relative refractory zone” showing inhibition of function •The computer output passes through a gain stage of 23 to amplify the signal for patient delivery to any desired voltage between 13.8 and 59.8V. •When inhibitory neurons are tonically excited, other inhibitory neurons are excited through mutual inhibitory connections (Jefferys et al. 202-208). •The circuit consists of a precision instrumentation amplifier, resistors, fans, and a battery power supply contained under the laptop. •When an excitatory nerve is repeatedly stimulated, it can cease responding to the stimulus effectively inhibiting the nerve and all of its downstream connections (See adjacent graphic). •The power supply to the amplifier is a 9V rechargeable Nickel Metal Hydride battery. •At this point, the use of the vagal nerve to administer electroanesthesia is theoretical, but through the development and further research into vagal nerve stimulation full anesthesia may be achieved. Market Analysis •20 million people undergo surgery using general anesthesia each year in the United States. •An electroanesthesia device would reduce the cost of anesthesia and the need for a highly trained anesthesiologist making it especially marketable in less developed countries. •Electroanesthesia devices in the European market utilize transcranial methods. Risks Reduction Technique Low current and voltage Insulated housing and wires Computer, circuit, and fans are grounded Unplugged during use Thorough testing of computer code Backup battery Electrical Shock Applicator •The white foam backing of the pad electrode allows for stretch-ability and memory over repeated use. The carbon/silver film gives uniform current distribution and lower impedance levels for more comfort. •A monopolar 1 in., 28 gauge conical tip needle electrode will be used to delivery the desired signal for any length of time. •Substitute for intravenous and gas anesthesia in any medical procedure requiring general anesthesia below the neck. Safety Considerations •A rechargeable battery maintains the portability of the device while also offering an easy way to recharge the system. •Pad or needle electrode. •Nothing on the market in the US similar to the proposed device. To date, the FDA has not approved any electroanesthesia devices and considers them to be Class III medical devices under 21CFR868.5400. Approval for such a device needs to go through a Premarket Approval (PMA) or Product Development Protocol (PDP). Extensive clinical testing, the disclosure of specifications, intended use, manufacturing methods, and proposed labeling would be required for the PMA process. In order to collect preliminary data and show proof of concept, animal testing would have to be conducted first. Before proceeding with animal testing, Institutional Review Board (IRB) approval would need to be obtained. After these studies, an investigational device exemption (IDE) would need to be cleared for human trials to begin. •During waveform generation, a plot showing the current waveform generation and a plot showing a ten second window of all of the pulses during the session are displayed. •Ammons et al. (1983) proposed that there are sites on the brain stem that can activate descending inhibitory pathways via the stimulation of the vagal nerves and the surrounding nerves. •Hammond et al. (1992) reported that “synchronous bursts of potentials could be dispersed to widespread areas of the brain” through afferent pathways. FDA Regulations Housing •The laptop and amplification circuit are be housed within an 18" x 18" x 10" compartment constructed from rigid high-density polyethylene. •Underneath the laptop is space for the circuit, a battery and charger to run the circuit and fans, a power strip to connect all of the devices, and extra space for the storage of the recommended vital signs equipment. Pad Electrode Needle Electrode Cessation of Function Detachment of Applicator Self-adhesive medical tape to be used Acknowledgements Special thanks to Dr. James Berry, Dr. Paul King,, Ray Erlandson, Ray Booker, Patrick Taylor, Dr. Jerry Collins References Ammons et al. "Vagal Afferent Inhibition of Primate Thoracic Spinothalamic Neurons." Journal if Neurophysiology 50.4 (October 1983): 926-940. Clarke, H.L. "Anaesthesia for Out-Patient Procedures." The West African Medical Journal 11 (1962): 155-160. Cork et al. "The Effect of Cranial Electrotherapy Stimulation (CES) on Pain Associated with Fibromyalgia." The Internet Journal of Anesthesiology (2004): 1-7. Hammond et al. "Electrophysiological studies of cervical vagus nerve stimulation in humans: I. EEG effects.." Epilepsia. 33 (1992): 1013-1020. Jefferys, John GR, Roger D. Traub, and Miles A. Whittington. "Neuronal networks for induced '40 Hz' rhythms." Trends in Neuroscience 19 (1996): 202-208. Kirchner et al. "Left vagus nerve stimulation suppresses experimentally induced pain." Neurology 55.8 (2000): 1167-1171. Ness, T.J., R.B. Fillingim, A. Randich, and E.M. Backensto. "Low intensity vagal nerve stimulation lowers human thermal." Pain 86 (2000): 81-85. Photiades et al.. "Electroaneasthesia in Major Surgery ." The West African Medical Journal (October 1963): 218-225. Sances Jr., Anthony, and Sanford J. Larson. Electroanesthesia Biomedical and Biophysical Studies. New York: Academic Press, Inc., 1975. Takakura, Kintomo. “Transcutaneous Electrical Nerve Stimulation for Relieving Pain: Physiological significance of the 1/f frequency fluctuation.” Accessed 11/4/05 <http://www.everbest.com.au/TENSforRelievingPain1ffrequencyfluctuation.html.>