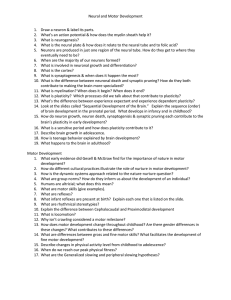
Project Checklist - the BRIGHT Foundation
advertisement

Scientific Advisory Board April Planning Meeting American Academy Of Neurology San Francisco, CA April 25th, 2003 BRIGHT - Brain Injury Group, Hope through Treatment 262-641-5639 www.brightonline.org info@brightonline.org Page 1 - Agenda Hour 1 Hour 1 - What can be done to help the children? • Introduction of BRIGHT members and Advisory Board Members • Brief summary of BRIGHT's Vision, Goals & Objectives from a parent's perspective • Brief summary of current state of knowledge, mechanisms of loss of function, mechanisms of recovery, (Matt to summarize, and send in advance, team to elaborate on during call) • Discussion of disparity between parents wants/needs and 5-10 year achievable goals (technical disparity as well as economic disparity). What specifically is not currently being addressed? • Summary - Three most promising areas to achieve parent's goals in 5-10 years 262-641-5639 www.brightonline.org info@brightonline.org Page 2 - Agenda Hour 2 Hour 2 - How does the team organize itself to best help the children? • Is there existing organizational capacity/interest to implement these solutions or does new capacity need to be created? • What organizational structures would best allow the goals to be met? (i.e. parent advocacy group to generate interest and funding, a scientific workgroup to refine the science, and partner company to implement the rehab solution?) • Can this current team provide all the skills to achieve the goal or do new members need to be recruited? • Discuss detailed plan to organize - what will excite and motivate the group to work for our kids? (Form a Coalition? Form a new workgroup? Operate under the umbrella of BRIGHT? Governing structure?) • Survey funding sources. (NIH, private foundations, corporate sponsors, direct fundraising) • Action plan to secure funding. Who/What/When • Summary - Define organizational strategy and who/what/when to secure funding. • Next steps - Develop operating mechanism to monitor who/what/when. Set next teleconference date. 262-641-5639 www.brightonline.org info@brightonline.org Page 3 - Vision, Goals & Objectives Vision Goals and Objectives - From a parents perspective... Mission and Population Served: Our mission is to facilitate the organization and prioritization of resources around the goal of development and implementation of effective treatments for acquired brain injuries suffered in the fetal, neo-natal and the early childhood period. (I.e. primarily the Cerebral Palsy population) Vision: Our vision is that our children will move and communicate successfully, allowing them their entitlement of a rich and full life. Objectives: Our objectives are focused on the implementation of effective treatment strategies with-in the next 5-10 years such that our children will benefit. • Full recovery of lost function for mild to moderate CP (GMFM Level 1-3) • Attainment of enough function for improved quality of life for severe CP (GMFM Level 4&5) • Improvement of cognition for types of CP where cognition is impacted Our focus is organization and prioritization of available resources for accelerated results Page 4 - What Is BRIGHT? BRIGHT’s Accomplishments to date... • Received official 501(c)(3) status • Developed a leadership core team with varied skill sets • We have developed sources for operating funding including a letter writing campaign, on-line shopping, used car donation program, etc. • Our website received over 300,000 hits in March alone… provides information and resources for parents of brain injured children • Our discussion groups provide support and guidance to both parents and practicing professionals, with over 4,000 messages exchanged. 2003 focused on building BRIGHT’s core organization capacity Page 5 - Scope of the BRIGHT’s Interest BRIGHT believes an organizational capacity needs to be developed that has expertise in all physical processes affecting BI children... • Neurological issues associated with the initial brain lesion • Physical issues likely linked to the initial brain lesion, (I.e., sensory issues, muscle tone issues, Cortical Vision Impairment, GI issues, dysphagia, diaphragm weakness, etc.) • Cognitive issues caused by the initial brain lesion • Developmental issues caused by the secondary effects of the Brian Injury… I.e. • Development Disregard ala Ed Taub • Maladaptive Plasticity ala Terry Sanger’s work with late onset dystonia • Diminished myelinization because of reduced activity ala John McDonald • W-sitting causing physical hip and knee issues, etc. Does our current group have the expertise to address all these areas… We will revisit in Part II of the call Page 6 - Current State of Knowledge What is our current state of science and clinical capability for these kids... 1.) Plasticity is seen as the key mechanism of recovery for children with early brain injury • Advances in neuro-imaging have shown that the brain is capable of plastically changing, using healthy areas to compensate for damage… this is an major scientific paradigm shift (Nudo, 2000; Xerri et al., 1998; Jenkins et al., 1990; Kaas et al., 1990) • This concept can be “Branded” with the term “Plasticity” • The concept of recovery of function through Plasticity has been demonstrated in both clinical interventions as well as in neuroscience research. • Plasticity can be broadened to include the concept of both re-organization of the brain (I.e. training) as well as re-regeneration (I.e. Cell repair) of the brain through the re-wiring of new neural cells • Re-generation (I.e. Cell repair) itself, will likely not result in improved function, ala Doug Kondziolka • Re-organization (I.e. Training) itself, may not be enough in for recovery in some lesion types (I.e. Basal Ganglia) where the damaged cells are specialized and neighboring cells can not adapt? Is a combination of Re-generation and Re-organization needed for these kids? Translating basic knowledge about brain plasticity into solutions for children with early brain injury Page 7 - Current State of Knowledge What is our current state of science and clinical capability for these kids... 2.) The brain’s development is influenced through physical interaction with the environment • Humans develop motor skill through a dynamical system approach. Motor development can be modeled as an open self organizing thermodynamic system. Changes in initial state (such as a brain injury, will have an effect on the resultant state of the system.) To some extend these changes should be predictable, and we in fact see them manifest themselves clinically (w-sitting, hip issues with Down Syndrome kids, etc.) • Maladaptive plasticity can result in secondary issues beyond the effects of the initial brain injury • Although the brain is capable of recovery, often little recovery occurs spontaneously… this pattern is entirely predictable based on established principles of behavioral conditioning and has been given the term “learned nonuse” (Taub, 1994; Taub and Wolf, 1997; Le Vere, 1980) • Maladaptive Plasticity ala Terry Sanger’s work with late onset dystonia • Diminished myelinization because of reduced activity ala John McDonald • W-sitting causing physical hip and knee issues, etc. Page 8 - Current State of Knowledge Vicious Cycle ... Abnormal inputs reinforce original brain injury 2001 - 5yr Weakness & illness retard Cognitive & Motor Learning Brain Injury Causes abnormal neurological condition Sensory Issues & Spasticity Occurs Childhood BI’s Vicious Cycle Reflux & Aspiration lead to chronic infections 1996 - 1yr Smooth Muscle Weakness Effect Digestion & Respiration 1999 - 3yr Childhood Plasticity Can Be Advantageous and Disadvantageous to Recovery… Can We Break The Vicious Cycle By Identifying and Treating the Impairments? Page 9 - Current State of Knowledge What is our current state of science and clinical capability for these kids... 3.) Learning (plasticity) is facilitated during “Critical Periods”, • There are critical periods that learning is most efficient I.e Patching the good eye • Can critical periods be expressed as periods of increased focal plasticity? Can critical periods be “reproduced” through techniques such as TMS or drugs? 4.) Effective measurements will be critical for problem solving… what tools are available • Motor Growth Curves - can they provide statically significant data for small case studies • fMRI - It as increased BOLD signal an effective surrogate marker for re-organization? Can we learn from fMRI? • Movement Analysis - what can it tell us about motor learning? Page 10 - Current State of Knowledge Motor Growth Curves • Motor Growth Curves were on a large population of mixed CP kids in Canada over four years using the GMFM test. • The curves appear to be predictive. • The curves may serve as a control group against case studies can be measured. • If a child is performing statistically better then the GMFMCS Group, can we conclude that the results are significant? Prognosis for Gross Motor Function in Cerebral Palsy Peter L. Rosenbaum, MD,FRCPC; Stephen D. Walter, PhD; Steven E. Hanna, PhD; Robert J. Palisano, ScD; Dianne J. Russell, MSc; Parminder Raina, PhD; Ellen Wood, MD,FRCPC,MSc; Doreen J. Bartlett, PhD; Barbara E. Galuppi, BA JAMA. 2002;288:1357-1363. Page 11 - Current State of Knowledge What is our current state of science and clinical capability for these kids... 5.) Possible process for problem solving • Can problem solving be done on a child by child basis and not in large multi-center clinical trails? 1.) Define goals 2.) Establish reliable measurement system (both for Y's and x's) Y's re outcomes as measured on the GMFM test. X's are parameters like individual muscle strength, motivation, speed of transmission of signal from the nerve to the brain, temperament, number of motor neurons recruited, mood, output of the basal ganglia to the frontal lobe, etc. 3.) Collect data (ideally in numerical form) 4.) Analyze data (ideally sharing the data with a large number of people) 5.) Identify the vital few x's in the data (use techniques like statistical analysis and Design Of Experiments to achieve this) 6.) Develop experimental techniques to address the vital few x's 7.) Measure again 8.) Analyze the data again 9.) Make corrections 10.) Ensure that the goals have been met. Page 12 - Current State of Knowledge What is our current state of science and clinical capability for these kids... 6.) Possible treatment tools for improved function • CIMT, Shaping, and massed practice - Functional gain through reorganization • Robotic Assisted Therapy - Same mechanism as CIMT • Artane - Impairment reduction pharmacologically for certain lesions (improves upper extremity movement ) •TMS - Can it selectively induce increased plasticity? • Intense Activity - Can it induce neural generation? Reduce Spasticity? • Strength Training - Can it reduce Spasticity? • TheraTogs - Can this system provide stability and alignment and allow long term motor learning? • Botox, Baclofen - Can it prevent contractures and result in improved long term motor learning? Which treatment approach will result in Improvements faster than the Motor Growth Curves? Page 13 - Short Term Focus What is our current state of science and clinical capability for these kids... • Discussion of disparity between parents wants/needs and 5-10 year achievable goals (technical disparity as well as economic disparity). What specifically is not currently being addressed? • Summary - Three most promising areas to achieve parent's goals in 5-10 years What Three Specific Treatment Approaches Should BRIGHT Focus Page 14 - Organizational Capacity Do organizations exist that are trying to solve this problem? • No Specific NIH Focus • United CP Research Foundation - Focus on causation & prevention • Movement Disorders Study Group • Carter Foundation • Children’s Neurological Solution - Focus on stem cells? • ABC - AAN’s coalition • ?? Does a GAP exist? Is a new organization needed? Page 15 - Organizational Structure What structure would allow BRIGHT to meet the goal of dramatically helping our children in 5-10 years? • Parent advocacy group to generate interest and funding • A scientific workgroup to refine the science • Partner company to implement the rehab solution What is needed? Page 16 - Current Team Advisory Team Focus Adult Or Neuro- Robotic Neuro Cell Movment Learning Child? Neurology Rehab Science Thearpy Imaging Thearpy Science Theory Diane Damiano, PhD Child Suz Campbell, PhD Child Neville Hogan, PhD Adult Mike V. Johnston, MD Child Billi Cusick, PT Child Dennis Matthews, MD Child Mike Merzenich, PhD Adult Joh Mink, MD Adult Terry Sanger, MD, PhD Child Marsha Seltzer, PhD Child Clive Svendsen, PhD Adult Ed Taub, PhD Adult Esther Thelen, PhD Child Bev Ulirch, PhD Child Nathan Urban, PhD Adult a a a a a a a a a a a a a a a a a a a a a What Skills Need To Be Added To The Team? a a Page 17 - Motivations What will excite and motivate you to work towards BRIGHT goals? How do we structure ourselves? What are our Governing Rules? How do we disburse funds? Will you get involved? How do we structure ourselves? Page 18 - Funding What are the existing funding sources? How likely is it that we will be funded? To what amounts? How long is the funding cycle? NIH? Private Foundations? Corporate Sponsors? Direct Fundraising? What is our funding strategy? Page 19 - Action Plan For Funding Who? What? When? Action Plan Page 20 - Next Steps • How will we measure success? • How will we share information? • How often will we meet? • What is our next step? • When will we have our next call? Operational Mechanism