Document
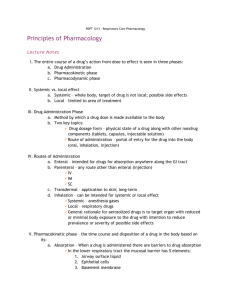
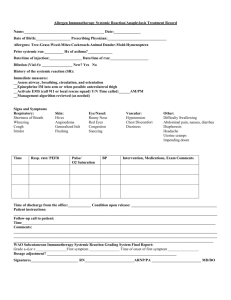
advertisement

Dermatotherapeutics - Systemic Digital Lecture Series : Chapter 31 Prof. Satyendra Kumar Singh Department of Dermatology and Venereology Institute of Medical Sciences, B.H.U., Varanasi CONTENTS Introduction Retinoids Sulfones Cytotoxic Agents Antihistamines Antimalarials Systemic Steroids Drugs Used During Pregnancy & Antibacterial Agents Lactation Antifungal Drugs MCQs Antiviral Drugs Photo Quiz Antiparasitic Agents Introduction The current-day dermatologist is well equipped with an array of therapeutic tools in his/her armamentarium for the successful management of various dermatoses. A better understanding of diseases has resulted in the evolution of drugs that act more specifically with minimal risk to the patient. Drug interactions, resistance and side effects, however, pose challenge to the treating physician. Commonly used systemic agents in dermatological disorders will be discussed. Sulfone : Dapsone Metabolized in liver and excreted by the kidneys Doses : 50 to 300 mg/day Drug interaction : with rifampicin, probenecid, omeprazole, and trimethoprim Dapsone resistance : reported in leprosy (changes in DNA sequences in fol P gene) Important indications : Leprosy, Dermatitis herpetiformis, erythema elevatum diutinum Other indications : Bullous eruption in SLE, linear IgA disease, actinomycetoma, bullous pemphigoid, subcorneal pustular dermatosis, chronic bullous disease of childhood, ITP, acne conglobata, pyoderma gangrenosum. Dapsone : Adverse effects Pharmacologic : hemolytic anemia and methemoglobinemia GI system : Gastric irritation, nausea, anorexia, hepatitis, cholestatic jaundice Headache, fatigue, psychosis Muco-cutaneous : morbilliform eruptions, erythema multiformae, exfoliative dermatitis, SJS/TEN Leukopenia, agranulocytosis Peripheral neuropathy (almost always motor) Antihistamines Histamine receptors are of four types:• H1 receptors : vasodilation of small vessels, smooth muscle contraction and itching. • H2 receptors : gastric acid production. • H3 receptors : located in brain, & responsible for histamine production & release. • H4 receptors : on immune active cells (eosinophils, neutrophils), in GIT and CNS Antihistamines classification:• Traditional/classic or First generation • Low-sedating or second and third generation • H2 type antihistamines H1 antihistamines (H1 AH) Both traditional & low sedating antihistamines are commonly used in dermatological disorders. Low sedating AH are preferred in chronic urticaria. First generation antihistamines cause sedation as they cross blood brain barrier. Most H1 AH are FDA category B or C Some AH (hydroxyzine, fexofenadine) cross the placenta while some others (chlorpheniramine, cetrizine, loratadine) do not cross. Desloratadine and mizolastine are safe in renal disease patients. Cetrizine, fexofenadine and desloratadine are safe in hepatic patients First generation antihistamines First generation antihistamines Doses Chlorpheniramine maleate 25-50mg, 6-8 hourly Diphenylhydramine HCl 25-50mg, 6-8 hourly Promethazine 12.5-25mg, 6-8 hourly Hydroxyzine HCl 10-25mg, 6-8 hourly Cyproheptadine HCl 4-5mg, 8-12 hourly Second and third generation antihistamines Second & third generation antihistamines have minimal sedative & anticholinergic effects. Examples – Cetirizine (10mg), Levocetirizine (5mg), loratidine (10mg), Desloratidine (5mg), Ebastine (10-20mg), Fexofenadine (30-180mg). Traditional antahistimines need to be used in multiple daily dosages while newer drugs are used in a once daily dose. Presence of H2 receptors in the cutaneous vasculature justifies their use in dermatology. Mechanism of action Act by competitive inhibition of the actions of histamine by receptor blockade thereby reducing histamine mediated pruritus. These drugs also prevent vasodilation, transdution and formation of typical wheals on the vascular endothelial surface. Indications Indicated as first line treatment for pruritus, urticaria & angioedema. Side Effects Sedation & impaired concentration are the main adverse reaction hence evening dosing is preferred. Anti-cholinergic effects include mucosal dryness, urinary retention & precipitation of Glaucoma. Cutaneous side effects include photosensitivity & eczematous dermatitis. Precautions One should always observe caution while using antihistamines in hepatic diseases, epilepsy, BPH, Glaucoma, porphyria, & concomitantly with CNS depressants. Loratidine is currently approved as a safe drug to use in pregnancy & lactation. Chlorpheniramine and diphenhydramine are also considered safe in pregnancy. Systemic Steroids Systemic steroids are used for their anti-inflammatory & immunosuppressive effects in various dermatoses. Mostly low doses are used over the shortest possible time period. High doses of steroids are used in emergencies & in periods of stress and trauma. Mechanism of Action At the Cellular Level Steroids passively diffuse through the cell membrane. Bind to intra-cytoplasmic soluble protein receptors to form a complex. This complex enters the nucleus. Regulates the transcription of a limited number of genes. Decreased synthesis of pro-inflammatory molecules (ILs, cytokines, & proteases). Synthesis of lipocortin increases Reduces phospholipase A2 activity Reduces the concentration of PGs, & LTs. Steroids reduce the no. of monocytes, lymphocytes & eosinophils and increase the no. of neutrophils. They modify cellular activation, proliferation & differentiation Indications Long Term Systemic Steroids – Pemphigus, bullous pemphigoid, SLE, dermatomyositis, eosinophilic fasciitis, vasculitis, neutrophilic dermatoses & lepra reaction. Short Term Schedule – Atopic dermatitis, acute/disseminated eczema of varying etiology. Also used in Toxic epidermal Necrolysis, Erythema Nodosum , erythema multiforme, exfoliative dermatitis, Lichen planus and Discoid lupus erythematosus. FDA-approved indications of systemic steroids Pemphigus vulgaris, pemphigus foliaceus Bullous pemphigoid Stevens Johnson Syndrome and TEN Systemic lupus erythematosus Dermatomyositis Erythema multiformae minor Severe urticaria Pemphigus Vulgaris SLE Equivalent Doses of Corticosteroids Prednisolone/Prednisone 5 mg Methylprednisolone 4 mg Triamcinolone 4 mg Deflazacort 6 mg Betamethasone/Dexamethasone 0.75 mg Hydrocortisone 20 mg Side Effects Adverse effects vary & depend on the type of steroid used, the dosage & duration and patient factors. Low dose administration over a longer duration is more likely to precipitate side effects than a high dose over a short period. Immunosuppression, precipitation of infection & suppression of the HPA axis. Following lists the side effects in head to toe order :raised ICT, psychosis, glaucoma, premature cataract, cushingoid features, activation of pulmonary TB, hypertension, gastritis, perforation, pancreatitis, worsening of diabetes, osteoporosis, premature closure of epiphysis, avascular necrosis of the femur. Calcium and Vit. D supplementation is essential in postmenopausal women & elderly patient. Drug Interactions Steroids increase the metabolism of barbiturates, phenytoin, rifampicin, salicylates, antihypertensive, anti diabetic and increase in their dosage during concomitant therapy is therefore essential. Antibacterial Agents PENICILLINS Still the drug of choice for infections caused by gram-positive cocci. Antistaphylococcal penicillins include oxacillin, dicloxacillin, flucloxacillin and naficillin orally for mild infections or systematically. Acute side effects-life-threatening angioedema and hypersensitivity reactions such as urticaria, morbifilliform rashes, exfoliatve dermatitis, drug fever, serum sickness or Stevens Johnson syndrome. Injectable form are always preferred over oral forms for their proven efficacy. Other Penicillins Aminopenicillins (ampicillin, amoxicillin) Carboxypenicillins (Carbenicillin, Ticarcillin) Ureidopenicillin (Mezlocillin, Azlocillin, Piperacillin) ß-lactam group of Monobactams (Aztreonam) & Carbapenems (Imipenem, Meropenem). ß-lactamase inhibitors – Clavulanic acid, Sulbactam, Tazobactam NOTE : In combination formulations these restore the antibiotic activity of Amoxicillin, Ticarcillin (Clavulanic acid), ampicillin (Sulbactam), Piperacillin & Cefoperazone (Tazobactam), against a spectrum of both gram positive & negative organisms. Antibiotic allergic reactions and diarrhea are the main threat with combinations. Cephalosporines These broad spectrum antibiotics are best used as second line drugs in bacterial infections. Based on ß- lactamase stability & in vitro test these are classified as:- Generation First generation (Gram Positive) Second generation (Gram Positive) Third generation (Nosocomial Gram Negative including Enterobactericeae & Ps. Aeruginosa) Fourth Generation (Nosocomial Gram Negative including Enterobactericeae & Ps. Aeruginosa) Drug details with adult dosing Cefadroxil (0.5-1gm BD orally), Cephalexin (0.5-1gm QID orally) Cefuroxime (1.5gm 6-8 hourly, I.V. ) Cefoxitin (2gm 4-6 hourly, I.V. ) Cefaclor (0.5-1gm TDS, orally) Ceftriaxone (2gm, 12hourly, I.V. ) Cefotaxime (1gm, 12hourly, I.V. ) Cefpodoxime (200mg, BD orally ) Cefixime (0.4gm BD orally) Cefipime ( 1-2gm, 8-12hourly, I.V.) Aminoglycoside The action spectrum of aminoglycosides is mainly against gramnegative bacteria, and they act synergistically with penicillins against staphylococci. They should not be used alone in skin infections to avoid drug resistance among gram-negative bacteria and Ps. aeruginosa. Systemic : Tobramycin, Netilmicin, Amikacin, and Isepamicin. Topical : Neomycin, Both Topical & Systemic : Gentamicin Side effects include Ototoxicity & Nephrotoxicity. Tetracyclines Based on their half-lives these are classified as follows:• Short acting (oxytetracycline and tetracycline) • Intermediate acting (demeclocycline and methacycline) • Long acting- Doxycycline, Minocycline Dosage Schedule Tetracycline – 250-500mg QID daily Doxycycline - 200mg loading dose, f/b 100mg /day Minocycline -200mg loading dose, f/b 100mg BD Side effects - photosensitivity & gastrointestinal disturbances. Minocycline - Vertigo ( in females around day 2-4 of starting the drug). Precautions Avoid in pregnancy, lactation, & <8 yr. of age, as it causes teeth anomalies & skeletal growth depression in foetus. Tetracyclines should not be administered with food, antacids, milk or iron containing compound. Macrolides & Lincosamides Macrolides - Erythromycin, Roxithromycin, Azithromycin, Clarithromycin. Lincosamides - Lincomycin, Clindamycin. Cross-resistance amongst macrolides and lincosamides is the rule. Their main Spectrum of action is against Gram-positive cocci. Clarithromycin is effective against MRSA. Telithromycin is a newer semisynthetic macrolide that acts against Gram-positive bacteria. Dosage Schedule Erythromycin - 250-500mg, orally, 6 hourly Clarithromycin - 250-500mg, orally, 12 hourly Azithromycin - 500 mg, orally before food, 24 hourly Lincomycin - 500 mg, IV/orally, 8 hourly Clindamycin - 300-600mg, IV/orally, 8-12 hourly SIDE EFFECTS Erythromycin may cause gastritis. Lincosamides may cause diarrhoea. 10% of patients may suffer from pseudomembranous colitis. Quinolones Quinolones (norfloxacin, ciprofloxacin, ofloxacin, moxifloxacin, pefloxacin, enoxacin) have a wide range of action & good tolerability. Their use in dermatology is limited to P. aeruginosa infections, UTI & leprosy. SIDE EFFECTS GI disturbances are more frequent than CNS & phototoxic adversities. Antifungal Drugs Systemic antifungal drugs play an important role in the management of both superficial and systemic infections. Indications for systemic antifungals Extensive superficial fungal infections Failure of topical therapy Recurrent attacks presence Involvement of hair & nails Poor compliance regarding topical application Presence of associated immunocompromised states Deep mycoses/systemic fungal infection Systemic Antifungal : Azoles Imidazoles – Ketoconazole, Miconazole Triazoles- Itraconazole, Fluconazole, Voriconazole, Posaconazole. Mechanism of action: by inhibiting 14 α demethylation affecting ergosterol synthesis in the cell membrane Drug interactions are more with these groups because of the involvement of cytochrome P450 system Antifungals Common Indications Comments Ketoconazole Candidiasis (200-400 mg/day) Pityriasis versicolar (400 mg single dose or 200 mg/day for 5 days) Dermatophytosis, seborrhoeic dermatitis, mycetoma sporotrichosis and chromomycosis. Hepatotoxic, gynaecomastia, and menstrual irregularities Fluconazole Primary and secondary drug resistance common, Safe drug Candidiasis (100-200 mg/day) Pityriasis versicolar (400 mg single dose) Dermatophytosis (150 mg/week) Antifungals Itraconazole Common Indications Candidiasis (100-200 mg/day) Pityriasis versicolar (200 mg/day) Dermatophytosis (200 mg/day) Pulse therapy in onychomycoses (400 mg/day for 1 week every month for 2 or 3 months for finger & toenails, respectively) Deep fungal: mycetoma, sporotrichosis and chromomycosis., aspergillosis and histoplasmosis Comments Expensive, effective against most fungi Extensive tinea Kerion Mycetoma Onychomycosis Systemic antifungal : ALLYLAMINES Terbinafine is highly effective against dermatophytoses Mechanism Of Action Acts by inhibiting squalene epoxidase, results in the accumulation of squalene and ergosterol INDICATIONS Used to treat dermatophytoses, mould fungi such as Aspergillus, dimorphic fungi and pigmented fungi Only the topical formulation acts against Candida species and Malassezia Also used in sporotrichosis and chromomycosis Terbinafine Dosage Schedule In tinea corporis – 250 mg/day for 1-2 weeks Fingernail infections – 6 weeks Toenail infections – 12 weeks SIDE EFFECTS Headache, GI symptoms and skin rash. Caution is to be observed on concomitant usage of rifampicin and warfarin. Polyenes The oldest of systemic antifungals, they are macrolides derived from Streptomyces species. Drugs in current usage include Amphotericin B, Nystatin and Natamycin. Mechanism of action These binds on to the cell membrane and cause cell leakage. Amphotericin B Effective against systemic mycoses such as Candidiasis & aspergillosis. Amphotericin B is available in four parenteral forms: • Amphotericin B deoxycholate (0.5-1 mg/kg/day) • Liposomal amphotericin B (AmBisome) (3mg/kg/day) • Amphotericin B lipid complex (Abelcet) • Amphotericin colloid dispertion (Amphotec, Amphocil) S/E : Nephrotoxicity , which is countered to a certain extent by tagging liposomes to the drug. Griseofulvin Derived from Penicillium griseofulvum. Mechanism of Action It is fungistatic and acts by the inhibition of intracellular microtubules and so inhibits the formation of mitotic spindles. The defective fungal filaments dehydrate and curl; hence griseofulvin was also called – curling factor. It is also known to inhibit leucocyte movement and has an antiinflammatory action. Griseofulvin Indications Effective only against dermatophytes and is currently used in tinea capitis. The oral dose is 6-8 mg/kg/day in two divided doses. SIDE EFFECTS Nausea, gastritis, intolerable headache, photosensitivity and antabuse-like effects with alcohol. Drug interactions with phenytoin and phenobarbitone are known. Antiviral Drugs There is limited array of antiviral drugs for dermatological disorders. The early use of antivirals is advisable to reduce viraemia and fulminant infection and to minimize nerve damage. In herpes simplex, varicella and herpes zoster antiviral drugs should be used within 24, 48 and 72 hours of skin eruption respectively. Herpes Zoster Acyclovir Synthetic purine analogue used orally, intravenously, and topically. It is converted by thymidine kinase to acyclovir triphosphate which subsequently inhibits viral DNA polymerase. Resistance due to alteration to or deficiency of thymidine kinase. Commonly used orally to treat herpes simplex and varicella zoster virus infection Intravenous acyclovir is used in fulminant infections, the occurrence of CNS complications and in immunocompromised patients. Dosage schedule of antivirals Aciclovir Valaciclovir Famiciclovir Herpes simplex Primary 200mg, 5 times a day for 7-10 days 1g, twice a day for 7-10 days 250mg, orally 3times a day for 7-10 days Recurrence 400mg, 3times a day for 5days 500mg, twice a day for 5days 125mg, twice a day for 5 days Suppressive 400mg, twice a day 500mg, twice a day 250mg, twice a day Herpes zoster 800mg, 5times a day for 7 days 1g, 3times a day for 7 days 500mg, 3times a day for 7days Interferons Interferone α, β and γ belong to the cytokine network and are implicated in host defense. They have antiviral, antiproliferative and immunomodulatory properties. α-interferon is frequently used in dermatology in subcutaneous (HSV and HPV) or intralesional form (HPV infection ). Dosing : daily or pulse basis 5-10IU/kg/day for 7-10days. Side effect: flu-like system and fatique. Caution: cardiac disease and psychiatric illness. Antiparasitic Drugs Ivermectin Originally approved for strongyloidisasis and onchocerciasis, this drug is often used in the treatment of scabies and pediculosis capitis. A single dose of 200µg/kg is advocated on an empty stomach. It block blocks glutamate-gated chloride ion channels,causing neuromuscular paralysis in the parasite. Thiabendazole It is antihelmenthic and acts by inhibition of the enzyme fumarate reductase. It is useful in larva migrans and currens Dosage:1.5g/day for 2 days GIT discomfort is frequent on oral administration. Retinoids First generation (non-aromatic) - isotretinoin and tretinioin (all-trans retinoic acid) Second generation (monoaromatic) - etretinate and acitretin Third generation (polyaromatic) – bexarotene FDA-Approved indications : • Severe acne (isotretinoin) • Severe psoriasis (acitretin) • Cutaneous T-cell lymphoma (bexarotene) Retinoids : Dosing and Onset of Action Retinoid Dermatological condition Isotretinoin Nodulo cystic acne Acitretin Bexarotene Severe Psoriasis Cutaneous T cell lymphoma Dose Onset of action 0.5-1 mg/kg/day 3-4 weeks 0.5-1 mg/kg/day 4-6 weeks 300 mg/m² 3-6 months Retinoids : Mechanism of action It include all synthetic and natural compounds that have activity similar to vit-A. At the cellular level, the cytosolic RBP⟹transfers it to the nucleus. Retinoids activate the nuclear recepters and regulate gene transcription. They induce cellular differentiation, and have anti-inflamatory and antproliferative action. In the skin they have an anti-keratinising effect, and in sebaceous glands, they reduce sebum production and decrease maturation of sebocytes. Retinoids : Mechanism and Indications They induce cellular differentiation, and have anti-inflamatory and antproliferative action. In the skin they have an antikeratinising effect, and in sebaceous glands, they reduce sebum production and decrease maturation of sebocytes. Indications Retinoids are the drugs of choice for nodulocystic acne. Off label uses are rosacea, hydradenitis suppurativa, Darier’s disease,icthyosis and keratodermas. Retinoids : Dosage Schedule Acitretin (25-75mg/day) is the chosen retinoid for psoriasis, although uses is limited to pustular and palmoplanter psoriasis. Acitretin with PUVA is termed Re-PUVA. Isotretinoin (0.5-1 mg/day) is used in acne. An initial response is seen within 8 weeks and improvement continues through 20-24 weeks, Intermittent pulse therapy 0.5 mg/day for 7 days/month for 6 months is also used in acne. POST PRE Treatment with Oral Isotretinoin Methotrexate Dosage Schedule It can be taken orally, IV or IM. Oral dose commonly used is 2.5-15 mg/week in single dose. The ‘Winstein-Frost’ schedule recommends usage in 3 divided doses, given at an interval of 12 hours, on a weekly basis. SIDE EFFECTS Side effects infrequent when used as per standard therapeutic guidelines. Hepatotoxicity, pneumonitis, diffuse interstitial fibrosis, pancytopenia, gastritis. MTx is a potential teratogen and abortifacient. Plaque Psoriasis Methotrexate toxicity Methotrexate Monitoring Guidelines Includes complete haemogram, LFT and USG scan of the liver. Test are best done at 0,1,2,4,8, & 12 weeks, and later regularly every third month in long term therapy. Baseline liver biopsy is indicated at a cumulative dose of 1.5 g of total MTx usage in high risk patients while in others at 4g. Patients with grade I and II disease- can continue therapy Grade IIIA-can continue with repeat biopsy after 6 months. Grade IIIB and IV- calls for total discontinuation of therapy. Azathioprine It derived from 6-mercaptopurine, and considered a safer immunosuppressant because of infrequent toxicity. Indications Used for its both immunosuppressive and antiinflammatory effects. Commonest indication is pemphigus vulgaris. Other indications include vasculitis, neutrophilic dermatoses,CTD and recalcitrant photodermatoses. Pemphigus vulgaris Azathioprine Absolute contraindications include pregnancy, TPMT (thiopurine methyltransferase) levels of <5 U and the presence of fulminant infections. Dosage Schedule 0.5-2.5mg/kg/day, while the commonly used dosage 50-100 mg/day. SIDE EFFECTS Pancytopenia, precipitation of infections and drug hypersensitivity syndromes. A TPMT assay prior to starting treatment is always advisable. Cyclophosphamide It is derivative of nitrogen mustard acts by damaging the DNA molecule through its active metabolites. It is cell cycle nonspecific and depresses B cell functions more than T cells. Acrolein, an inactive metabolite, is the responsible for bladder toxicity. Hence proper hydration and good urinary output is needed Indications Used in severe pemphigus alone or as a constituent of Dexamethasone-Cyclophosphamide pulse therapy. Advanced mycosis fungoides, lupus erythematosus and Wegener’s granulomatosis. Cyclophosphamide Dosage Schedule It is used orally in a dose of 1-5 mg/kg/day in equal divided doses or as a single dose of 50-200 mg/day. Parental usage is in dose of 5-9mg/kg/day in lupus nephropathy and serious lupus vasculitis. SIDE EFFECTS Haemorrhagic cystitis, bladder carcinoma, leucopenia, anagen effluvium are common toxicities. The risk of transitional cell bladder cancer is 8-10 fold higher in these patients. Hydroxyurea This affects DNA synthesis & repair and gene regulation through inhibition of ribonucleotide reductase. Withdrawal of drug results in a rapid reversal of its effect. Oral tab are used in a dose of 1-1.5 g/day in divided doses. It is used infrequently in recalcitrant psoriasis. Adverse Reactions Marrow suppression, elevated transaminases, altered renal function and poikiloderma. Cyclosporine-A Acts by decreasing T-cell & keratinocyte proliferation. It also reduces levels of ILs & TNF. It is used in wide spread erythrodermic or pustular psoriasis. It’s a rapid ‘cooldown’ of the inflammatory component of a florid psoriasis. Also used in atopic dermatitis, recalcitrant urticaria & pyoderma gangrenosum. Dose : 3-5 mg/kg/day. SIDE EFFECTS Renal dysfunction, hypertension, tremors, dysaesthesia & gingival hyperplasia. Mycophenolate Mofetil MPA was used widely in psoriasis in previous years and mycophenolate mofetil, an esterified form with greater bioavailability is now used in atopic dermatitis, lupus erythematosus, psoriasis, refractory P.G. and bullous diseases. Mycophenolate mofetil gets cleaved to MPA after absorption. It acts by inhibiting de novo purine synthesis. It affects T & B- cells predominantly. SIDE EFFECTS include nausea, diarrohea, strangury and an increased incidence of viral & bacterial infections. Antimalarials : Hydroxy chloroquine (HCQ) Metabolized in liver but only 15 to 25 % of total clearance is through kidney Usual dose : 400 mg/day Photoprotective effects: high concentration in epidermis because of their affinity for pigment Immunologic and anti-inflammatory effects: decrease in T cell release of IL-1, IL-6, TNF and interferon gama Dermatologic indications : SLE, Discoid lupus, porphyria cutanea tarda, PMLE, Chronic cutaneous vasculitis, solar urticaria. Drugs Used During Pregnancy and Lactation Antihistamines Safer-diphenhydramine, chlorpheniramine, cyproheptadine and loratidine Avoid-hydroxyzine, fexofenadine and cetirizine Antihistamines may suppress lactation and create infantile irritability. Systemic Steroids Systemic steroids are avoided in the first trimester because of a risk of multiple-organ anomalies Short-term therapy is best advocated in the second and third trimesters. Drugs Used During Pregnancy and Lactation A short-term usage of topical steroids is also preferred; Potent and superpotent steroids are avoided because of the risk of systemic absorption. Antibacterial Agents SAFE : macrolide, penicillins and cephalosporins. AVOID : quinolones, tetracycline. Silver suphadiazine is not advised in the third trimester because of foetal haemorrhage. Drugs Used During Pregnancy and Lactation Antifungal Drugs Single-dose fluconazole is safe, while prolonged use is best avoided. Ketoconazole, terbinafine and griseofulvin are not advised in pregnancy and lactation. Antiviral Drugs Systemic antivirals are safe in all trimesters. An assessment of the risk-benefit ratio is done, and their usage is reserved for severe cases or near the end of the pregnancy. Drugs Used During Pregnancy and Lactation Antiparasitic Drugs Topical antiscabetics are considered safe, but large dose of lindane is not advised in pregnancy. Retinoids Systemic retinoids are totally contraindicated during pregnancy and lactation. Topical retinoids are avoided in the first trimester, whereas benzyol peroxide and azelaic acid are considered safe. Effect of Drug with respect to the Trimesters of Pregnancy & Lactation Before Conception (contraception Failure) The use of azathioprine, mtx, NSAIDs, Griseofulvin, Itraconazole, Tetracycline and rifampicin may result in contraceptive failure either directly or though hepatic enzyme induction First Trimester Drugs at this stage affect all cell equally, and cell death often results in spontaneous abortion. Differentiating cells, when affected, result in defective organogenesis and congenital anomalies. Hence, FDA pregnancy Category X and D drugs are totally avoided; they include retinoids, finasteride, methotrexate, thalidomide, colchicine, spironolactone, griseofulvin and cyclophosphamide. Effect of Drug with respect to the Trimesters of Pregnancy & Lactation Second Trimester Metabolism of drugs may be at a slower pace in the foetus compared to the mother, for example, foetal hypothyroidism with maternal iodine use. Drug excretion into the amniotic fluid results in a prolonged contact of the foetal skin with the drug. Third Trimester Non-teratogenic conditions occur; for example, sulphonamide-induced kernicterus, rifampicin-related foetal haemorrhage and immunosuppression and NSAIDs causing oligohydroamnios. Lactation Teratogenic drugs are best avoided. This include anti-neoplastics which may induce immunosuppression or a possible carcinogenesis. MCQ’s Q.1) A. B. C. D. Which is known as curling factor? Methotrexate Interferones Griseofulvin None Q.2) A. B. C. D. Which of the following is incorrect about retinoids? First generation-isotretinoin Second generation-acitretin Third generation-bexarotene Fourth generation-etretinate MCQ’s Q.3) Fexofenadine is given in infants above? A. 3 month of age B. 6 month of age C. 1 year of age D. 2 year of age Q.4) The dosage of intravevous methylene blue in the treatment of dapsoneinduced methaemoglobinemia? A. 50-60mg/kg B. 0.1-0.2mg/kg C. 5mg/kg D. 1-2mg/kg Photo Quiz A 23 yr old male presented with grouped vesicles on a erythematous base in a dermatomal distribution for 2 days, drug of choice for this patient is : A. B. C. D. Oral Steroids Oral Acyclovir Tetracycline Topical Steroids Photo Quiz A 10 month old male brought by mother with ruptured bullae and erosions with honey crust for 3 days. Identify the condition and its treatment : A. Bullous impetigo, oral antistaphylococcal B. Tinea faciei, oral anti fungal C. Scabies, topical permethrin D. Psoriasis, topical steroid Photo Quiz A 19 yr old male with nodulocystic lesions on face for 10 months, identify the lesions, its grade and best treatment : A. B. C. D. Acne grade 2, oral antibiotics Acne grade 3, topical antibiotics Acne grade 4, topical steroids Acne grade 4, oral retinoids Photo Quiz A 35yr old female presented with erythematous itchy plaques with silver white scaling all over body(BSA=12%). Identify the condition and best treatment for patient : A. B. C. D. Tinea corporis,oral antifungal Lichen planus, topical steroid Psoriasis, Oral methotrexate Psoriasis, oral steroids Thank You!