ADMINISTRATION OF TOPICAL AND INHALANT MEDICATION
advertisement

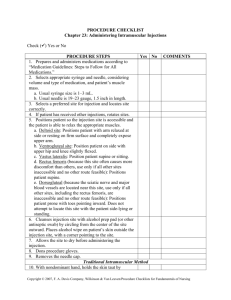
PART C: ADMINISTRATION OF TOPICAL AND INHALANT MEDICATION Topical Medications • Topical agents commonly used for a local effect • • Dermal medications (lotions, creams) are applied to rashes, lesions or burns for their local anti-inflammatory, antiinfective or anesthetic effect Inflamed, abraded or denuded skin will absorb drugs readily as will hydrated skin • • Most topical drugs act on the skin but are not absorbed through the skin Some medications are specially formulated to be applied (via adhesive patch or disc) for slow absorption thru the skin (transdermally) >>>>>>>>> Topical/Transdermal • • • Transdermal preparations allow drugs to be delivered at constant rates over several days (nicotine, nitrodur, duragesic, estrogen) Advantage of this system is much less of the drug is lost to metabolism in the GI tract or liver before it reaches the blood stream Another benefit is to Home Clients on medication as allows for fewer administration times allowing clt more mobility Topical/ophthalmic medications • Most often administered for • • • • • Infections or inflammations of eye Glaucoma Diagnostic purposes Topically applied eye meds used mostly for their local effects Unwanted systemic effects are possible if the drops drain thru the tear duct & enter the systemic circulation via the nasal mucousa absorption Topical/Nasal Drops • • Most administered for local effect (as in antihistamines), some can be given for a systemic effect Since nasal mucous membranes absorb drugs readily, an intended local may sometimes result in systemic toxicity • it is essential you understand purpose for drug being administered as well as rationale for particular drug route of administration Topical/otic meds • Usually come in liquid form & administered to treat conditions of external ear. If not effective, systemic drugs used • eg. Chloromycetin otic gtts are antibiotic for external ear canal infections • Can also have systemic effects (chloromycetin gtts can cause bone marrow depression) Inhalant medications • Drug droplets, vapor or gas are administered through mucous membranes of respiratory tract via use of • • • • • Face mask Nebulizer Positive pressure machine Metered dose inhalers Some drugs administered by inhalation will be bronchodilator, mucolytic & some antiinflammatory drugs. Primary effect will be local in the lungs Describe the procedure for: • • • • • • • Instilling eye drops Applying ointment to the eye Instilling nose drops Administering ear drops and ear irrigation Administering rectal and vaginal suppositories Skin applications Metered dose inhalants Instilling eye drops Applying ointment to the eye Instilling nose drops Administering ear drops Straightening the ear canal of a child by pulling the pinna down and back. rectal suppositories vaginal suppositories Skin applications Transdermal patch = prepared medicated PART D: PREPARATION OF MEDICATION FROM AMPULES AND VIALS • Identify parts of a needle and syringe Syringe – has three parts: • • • tip, which connects with the needle; barrel or outside part, on which the scales are printed; plunger, which fits inside the barrel. • Most commonly used types of syringes: hypodermic, the insulin, the tuberculin syringe Size of needle, type and size of syringe Syringe • Hypodermic syringes come in • 2, • 2.5, • and 3ml or 5ml sizes. Hypodermic syringe marked in tenths of a ml & in minims •They usually have two scales marked on them: •the minim = used for very small dosages •the milliliter = the one normally used Size of needle, type and size of syringe … • Insulin syringes are similar to hypodermic syringes (not interchangeable!), but they have a scale specially designed for insulin: • 100-unit calibrated scale intended for use with U-100 insulin. • Several low-dose insulin syringes are also available and frequently have a nonremovable needle. Insulin syringe marked in 100 units Size of needle, type and size of syringe … • Tuberculin syringes (originally designed to administer tuberculin) are narrow, calibrated in tenths and hundredths of a milliliter (up to 1ml) on one scale and in sixteenths of a minim (up to 1 minim) on the other scale. • also useful in administering other drugs, particularly when small or precise measurement is indicated (peds). Tuberculin syringe marked in tenths & hundreds of cubic ml & in minims • When handling a syringe the tip and inside of the barrel, the shaft of the plunger, and the shaft and tip of the needle must remain sterile. hypodermic insulin tuberculin • Needle – has three parts: the hub, which fits onto the syringe; • the cannula, or shaft, which is attached to the hub; • the bevel, which is the slanted part at the tip of the needle. • Size of needle, type and size of syringe … Needle • The bevel of the needle may be short or long. • • Longer bevels provide sharpest needles and cause less discomfort and are commonly used for subcutaneous and intramuscular injections. Short bevels are used for intradermal and intravenous injections. Size of needle, type and size of syringe … • • The shaft length of commonly used needles varies from ½ to 2 inches. The appropriate needle length is chosen according to the • • • client’s muscle development, client’s weight, type of injection. Size of needle, type and size of syringe … • The gauge (or diameter) of the shaft varies from #18 to #28. • • The larger the gauge number, the smaller the diameter of the shaft. Smaller gauges produce less tissue trauma, but larger gauges are necessary for viscous medications, such as penicillin. • Demonstrate the ability to assemble a needle and syringe, withdraw solutions from ampules and vials, mix medications from an ampule and vial, and prepare an injection from an ampule and a vial. Ampules versus Vial Drawing medication from an ampule. Break neck of amp Away from hands Draw up medication with ampule upright Medication can also be drawn upwards from ampule Drawing from a vial Mixing meds in 1 syringe P. 33-4 Figure 33.26 Administering SC, ID & IM All well covered in Perry & Potter pp.889-900 Administering sc Administering IM For Labs, Know your Land marking Administration Intradermal Figure 33.28a Figure 33.28b Subcutaneous • Only small doses of meds via sc • • Use syringe appropriate to med • • • • 0.5 to 1ml E.g. hypodermic, tuberculin or insulin Usually a #25, 5/8 inch needle used for normal sized adult pt Insert at 90 or 45 degree angle dependent upon size Sites need to be rotated systematically Sites for subcutaneous injections Figure 33.29 Insertion for sc at 45 or 90 degree angle Figure 33.30 Intramuscular injections • • • • Absorbed quicker than by sc (as more blood flow) Can also tolerate more volume by IM than sc • Well developed muscles can tolerate up to 4ml (in gluteus medius & gluteus maximus). • If they have less developed muscles can tolerate 1 – 2 ml • Deltoid tolerates 0.5 to 1ml Usually a 2 to 5 ml syringe used Standard needle size is #21 or #22, 1½ inch To form the Z track at the injection site, use the ulnar side of your nondominant hand to pull the skin and subcutaneous tissue about 1 inch (2.5 cm) to the side. Hold the skin in this position until you've administered the injection. Quickly withdraw the needle and release the displaced tissue. Apply gentle pressure to the site with a dry sponge. Factors to determine needle size & length • • • • Muscle to be used (if deltoid, often #23 to #25, 1 inch) Type of solution (if very thick, may need #20) Amount of adipose tissue (very obese may require 2 inch needle, very thin may require 1 inch) Age of client (infants & children will usually require smaller, shorter needles (#22 to #25, 5/8 to 1 inch) Intramuscular sites 1. 2. 3. 4. 5. Ventrogluteal (von Hochsterer’s site) is in gluteus medius muscle is preferred site Vastus lateralis – esp for children Dorsogluteal – not used in children < 3yrs Deltoid – no more than 1ml tolerated Rectus femoris – rarely used as causes discomfort Shows gluteal muscles used for IM Figure 33.32 Marking ventrogluteal site Figure 33.33 Vastus lateralis site Figure 33.35 Dorsogluteal site Figure 33.36 Deltoid muscle Figure 33.37 Deltoid landmarking Figure 33.38