C3 Semi-Solids 2015
advertisement

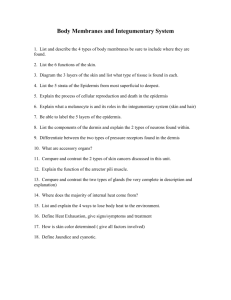
ELECTRICAL BARRIER Dry skin offers a highimpedance to the flow of an electric current. To ensure adequate electrical conductance during ECGs and EEGs, creams and pastes containing high electrolyte concentrations, are placed between the electrode surface and the skin. TOPICALS - why do we use them? 1. -to manipulate or assist the barrier function e.g. applying sunscreen, topical antibacterials and emollient topicals to restore the barrier 2. - certain drugs are able to diffuse into the viable epidermis and dermis in adequate amounts to produce a pharmacological effect in local tissues - if they diffuse beyond this region they are taken up systemically but generally these levels are very low. eg. a patient with a myocardial infarction - given warfarin (anticoagulant), happens to get a cramp - Voltaren rubbed on area - absorbed systemically & also affects coagulation - patient bleeds too much. 3. - drugs put on skin to produce systemic effects - this can happen with very potent drugs that have the physico-chemical requisites to permeate the skin. Factors to consider (to determine whether topical use of the drug is suitable) - what the drug within its delivery system is intended to do suppress inflammation (Voltaren gel - diclofenac) destroy microorganisms (Bactroban (mupirocin)} provide protection from the sun (sunblock with zinc oxide) stop glandular secretions, etc. - the target site for the drug and its accessibility - each drug system has a specific locus of action and if the drug does not reach and produce the desired effect at the specific location, there will be no therapeutic benefit Targets for topical drugs 1 Skin surface (external target) 2 Stratum corneum 3 Viable epidermis and upper dermis 4 Different skin glands 5 Systemic target Starting from the surface of the skin and moving inwards, the targets become more and more remote and inaccessible and the attainment of the desired effects becomes less and less certain. Surface Effects This is the most accessible target and surface therapy begins where cosmetics leave off e.g. Hiding unsightly blemishes Formation of a continuous protective film - if it has a UV light-absorbing chemical it becomes a sunscreen Film may absorb irritating chemicals such as a protective paste which absorbs and neutralizes ammonia formed by bacterial action on an infant's urine. Film may be applied to prevent moisture loss from the SC thus minimizing problems of windburn and chapping. In all these examples, the physical presence of the film itself is therapeutic, so bioavailability has no meaning. Surface bioavailability is important if topical antiseptics or antibiotics are used - the targets here are microorganisms, so the formulation must promote penetration of the chemical agent into the fissures and small cracks in the skin surface where the organisms resides as well as into the microorganisms themselves. The agent must partition from the film and be available at the surface of the microorganisms, and not be entrapped in the film. Activity is reasonably assured as long as a reasonable fraction of the drug is in solution. Deodorants inhibit or destroy surface organisms, preventing them from rancidifying apocrine secretions. Adsorptive products have surface actions e.g. calamine lotion - supposedly binds and inactivates contact allergens, but more likely benefits the patient by drying secretions and relieving itching. Stratum Corneum Effects It consists of dead layers of tissue and its function is dependent on the presence of adequate natural lipids, hydroscopic substances and moisture. There are 2 activities of topicals involving the SC: I) Emolliency This involves the remoisturizing of partially dehydrated SC i.e. "Softening" of the skin. This is accomplished by applying a lotion, cream or wax containing fatty acids and fatty acid esters to replace lost lipid constituents of the SC. They fill the cracks and crevices in the horny layer and seal it, allowing it to retain moisture drawn from living tissue. 2) Keratolysis This involves the chemical digestion and removal of thickened or scaly SC tissue. Such tissue is found in e.g. callouses , corns, dandruff, psoriasis. Common agents used are salicylic acid and sulphur- Uptake Into the horny layer is not necessarily easily achieved so e.g. salicylic acid may be made up as a concentrated non-aqueous solution in a volatile solvent (collodion flex) to maximize penetration into the SC. As the volatile solvent evaporates, the drug is concentrated in the film and driven into the tissue. PERCUTANEOUS ABSORPTION (Modern Pharmaceutics, Percutaneous Absorption: Clinical Insights pg 284-286) When the therapeutic target lies beneath the SC topical drug delivery becomes more difficult, as it is difficult to deliver sufficient drug to the target site. Percutaneous absorption is the phenomenon of diffusive penetration by drugs and chemicals into and through the skin. With local therapy, the concern has been to get enough drug into the living epidermis and dermis to effect a pharmacological action without, at the same time, producing a systemic load of the drug. However, because of permeability constraints, the emphasis is usually on getting enough drug to the target site, with very little chance of toxicity occurring. Variability in the permeability of healthy skin The permeabilities of skins of healthy individuals may vary as much as tenfold. Age: premature neonates have very permeable skins, thus incubators have to be used to maintain their body temperatures and prevent dehydration due to excessive perspiration. Gender: little evidence that permeability differs between the sexes. Race: the horny layers of Caucasian and black skin are of equal thickness, but the latter contains more cell layers and is more dense and therefore severalfold less permeable. Environmentally influenced differences: The hydrated SC is more permeable than the dry SC. Occlusive films placed over topical applications to seal off water loss and to induce hydration increase permeability. Otherwise, the state of dryness of the SC is determined by the prevailing humidity. Variability in the permeability of damaged skin The overall health of the skin determines its physical and physiological condition and thus its permeability. Broken skin will allow a high degree of permeability. Even when the skin is unbroken, its permeability changes in response to irritation and mild trauma e.g. sunburn - marked vasodilation with increased blood flow results in reddening of the skin (erythema) and the skin is warm to the touch - both characteristics of inflammation. After a day or two, repair of the epidermis begins a) Process of Percutaneous Absorption When a drug system is applied topically, the drug diffuses passively out of its carrier or vehicle and into the SC and the sebum-filled pilosebaceous gland ducts. Drug continues to diffuse inwardly through the full thickness of the SC and ducts and into the viable epidermis and dermal strata. A concentration gradient is established across the skin up to the outer reaches of the skin's microcirculation in the dermal layer. The systemic circulation acts as a reservoir or "sink" for the drug and a near-zero concentration of the drug is maintained at the plane formed at the edge of the capillaries, where the drug is passed into the general circulation and diluted. The drug then distributes very rapidly in the general circulation. Relatively high local epidermal concentrations of some drugs may be obtained as the epidermis is without a blood supply. Two main absorption routes have been identified: (1) transepidermal route where the drug diffuse directly across the SC. (2) transfollicular route where the drug diffuses through the follicular pore. If the skin is intact, the mian route for the penetration of drugs is generally through the epidermal layers. The film covering the horny layer is not generally continuous. The composition of this film varies with the proportion of sebum and sweat produced and the degree of their removal through washing and sweat evaporation and so has no definite composition, thickness or continuity. It is thus not a true barrier to drug transfer.