lec11
advertisement
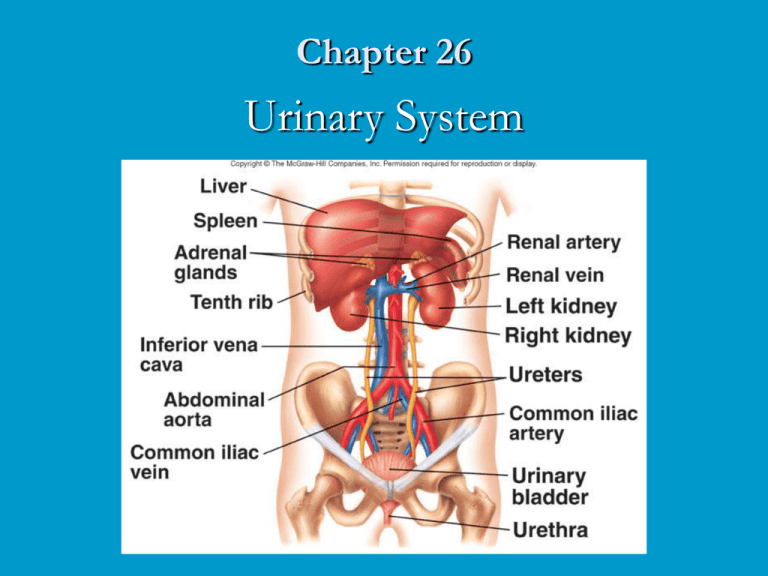
Chapter 26 Urinary System Urinary System Functions Filtering of blood Regulation of blood volume concentration of blood solutes pH of extracellular fluid blood cell synthesis Synthesis of Vitamin D Urinary System Anatomy: Location and External Anatomy of Kidneys Location Lie behind peritoneum on posterior abdominal wall on either side of vertebral column Lumbar vertebrae and rib cage partially protect Right kidney slightly lower than left External Anatomy Renal capsule Perirenal fat Engulfs renal capsule and acts as cushioning Renal fascia Surrounds each kidney Anchors kidneys to abdominal wall Hilum Renal artery and nerves enter and renal vein and ureter exit kidneys Internal Anatomy of Kidneys: Cortex: Outer area Medulla: Inner area Renal pyramids Calyces Renal columns Major: Converge to form pelvis Minor: Papillae extend Nephron: Functional unit of kidney Juxtamedullary Cortical The Nephron: Histology of the Nephron Internal Anatomy of Kidneys Renal corpuscle Bowman’s capsule Parietal layer Visceral layer Network of capillaries Afferent Blood to glomerulus Efferent Drains Proximal (convoluted) tubule Loops of Henle Arterioles Tubules Glomerulus Descending limb Ascending limb Distal (convoluted) tubules Collecting ducts Renal Corpuscle Kidney Blood Flow: Ureters and Urinary Bladder Ureters Tubes through which urine flows from kidneys to urinary bladder Urinary bladder Urethra Stores urine Transports urine from bladder to outside of body Difference in length between males and females Sphincters Internal urinary External urinary Ureters and Urinary Bladder Urine Formation Filtration Filtration Renal filtrate Plasma minus blood cells and blood proteins Most (99%) reabsorbed Filtration pressure Filtration membrane Fenestrated endothelium, basement membrane and pores formed by podocytes Responsible for filtrate formation Glomerular capillary pressure (GCP) minus capsule pressure (CP) minus colloid osmotic pressure (COP) Changes caused by glomerular capillary pressure Filtration Pressure Tubular Reabsorption Reabsorption Passive transport Active transport Cotransport Specialization of tubule segments Substances transported Active transport moves Na+ across nephron wall Other ions and molecules moved by cotransport Passive transport moves water, urea, lipidsoluble, nonpolar compounds Reabsorption in Proximal Nephron: Reabsorption in Loop of Henle Reabsorption in Loop of Henle Tubular Secretion Substances enter proximal or distal tubules and collecting ducts H+, K+ and some substances not produced in body are secreted by countertransport mechanisms Secretion of Hydrogen and Potassium Urine Production In Proximal tubules Na+ and other substances removed Water follows passively Filtrate volume reduced In descending limb of loop of Henle Water exits passively, solute enters Filtrate volume reduced 15% In ascending limb of loop of Henle Na+, Cl-, K+ transported out of filtrate Water remains In distal tubules and collecting ducts Water movement out regulated by ADH If absent, water not reabsorbed and dilute urine produced If ADH present, water moves out, concentrated urine produced Filtrate and Medullary Concentration Gradient Medullary Concentration and Urea Cycling Urine Concentration Mechanism When large volume of water consumed Eliminate excess without losing large amounts of electrolytes Response is kidneys produce large volume of dilute urine When drinking water not available Kidneys produce small volume of concentrated urine Removes waste and prevents rapid dehydration Urine Concentrating Mechanism I: Urine Concentrating Mechanism II: Hormonal Mechanisms ADH Secreted by posterior pituitary Increases water permeability in distal tubules and collecting ducts Aldosterone Produced in adrenal cortex Affects Na+ and Cltransport in nephron and collecting ducts Renin Produced by kidneys, causes production of angiotensin II Atrial natriuretic hormone Produced by heart when blood pressure increases Inhibits ADH production Reduces ability of kidney to concentrate urine Effect of ADH on Nephron Aldosterone Effect on Distal Tubule Autoregulation and Sympathetic Stimulation Autoregulation Involves changes in degree of constriction in afferent arterioles As systemic BP increased, afferent arterioles constrict and prevent increase in renal blood flow Sympathetic stimulation Constricts small arteries and afferent arterioles Decreases renal blood flow Clearance and Tubular Load Plasma clearance Volume of plasma cleared of a specific substance each minute Used to estimate GFR Used to calculate renal plasma flow Used to determine which drugs or other substances excreted by kidney Tubular load Total amount of substance that passes through filtration membrane into nephrons each minute Normally glucose is almost completed reabsorbed Tubular Maximum Tubular maximum Maximum rate at which a substance can be actively absorbed Each substance has its own tubular maximum Urine Flow and Micturition Reflex Urine flow Hydrostatic pressure forces urine through nephron Peristalsis moves urine through ureters Micturition reflex Stretch of urinary bladder stimulates reflex causing bladder to contract, inhibiting urinary sphincters Higher brain centers can stimulate or inhibit reflex Micturition Reflex Effects of Aging on Kidneys Gradual decrease in size of kidney Decrease in kidney size leads to decrease in renal blood flow Decrease in number of functional nephrons Decrease in renin secretion and vitamin D synthesis Decline in ability of nephron to secrete and absorb Kidney Dialysis