Semester 9 - Dysphagia PBL to be conducted on Tuesday
advertisement
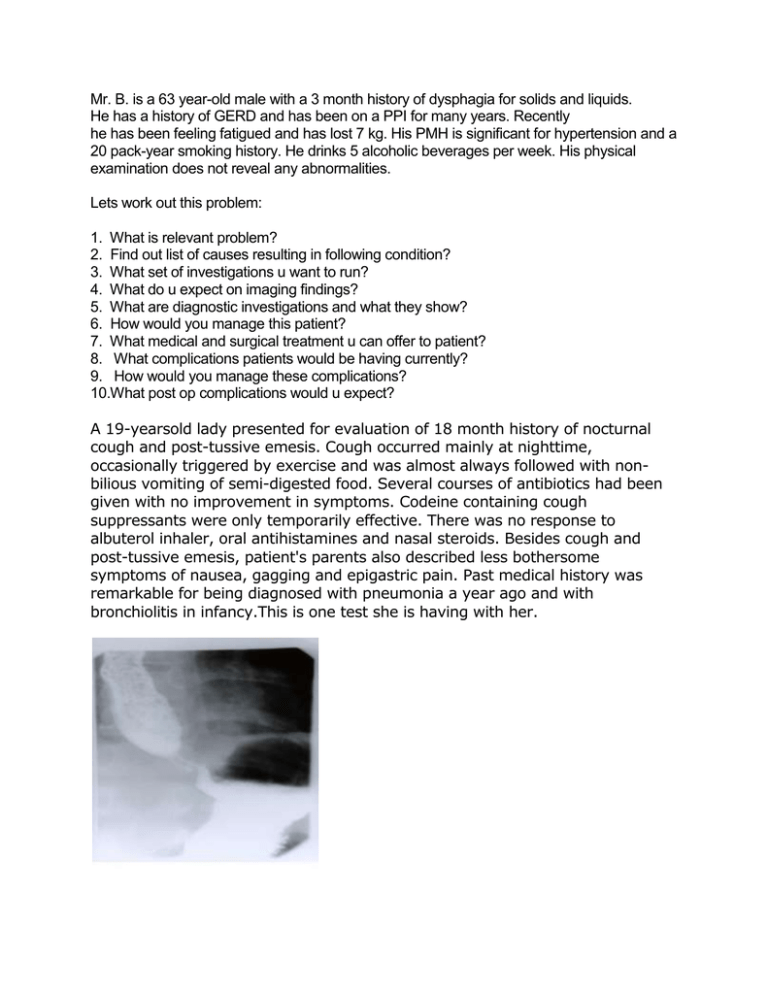
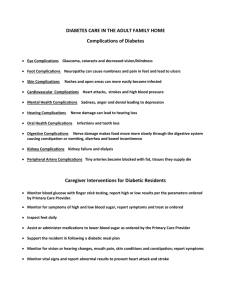
Mr. B. is a 63 year-old male with a 3 month history of dysphagia for solids and liquids. He has a history of GERD and has been on a PPI for many years. Recently he has been feeling fatigued and has lost 7 kg. His PMH is significant for hypertension and a 20 pack-year smoking history. He drinks 5 alcoholic beverages per week. His physical examination does not reveal any abnormalities. Lets work out this problem: 1. What is relevant problem? 2. Find out list of causes resulting in following condition? 3. What set of investigations u want to run? 4. What do u expect on imaging findings? 5. What are diagnostic investigations and what they show? 6. How would you manage this patient? 7. What medical and surgical treatment u can offer to patient? 8. What complications patients would be having currently? 9. How would you manage these complications? 10.What post op complications would u expect? A 19-yearsold lady presented for evaluation of 18 month history of nocturnal cough and post-tussive emesis. Cough occurred mainly at nighttime, occasionally triggered by exercise and was almost always followed with nonbilious vomiting of semi-digested food. Several courses of antibiotics had been given with no improvement in symptoms. Codeine containing cough suppressants were only temporarily effective. There was no response to albuterol inhaler, oral antihistamines and nasal steroids. Besides cough and post-tussive emesis, patient's parents also described less bothersome symptoms of nausea, gagging and epigastric pain. Past medical history was remarkable for being diagnosed with pneumonia a year ago and with bronchiolitis in infancy.This is one test she is having with her. Lets work out: 1. What is relevant problem? 2. Find out list of causes resulting in following condition? 3. What set of investigations u want to run? 4. What do u expect on imaging findings? 5. What are diagnostic investigations and what they show? 6. How would you manage this patient? 7. What medical and surgical treatment u can offer to patient? 8. What complications patients would be having currently? 9. How would you manage these complications? 10. What post op complications would u expect? A 52-year-old man is referred to your gastroenterology practice for a history of gastroesophageal reflux disease (GERD). The patient reports a long history of heartburn symptoms, dating back at least 5 years. His symptoms were responsive to over-the-counter remedies including antacid tablets and liquids, but eventually became such a regular occurrence that he sought medical care from his primary care physician. He was initially prescribed an H2 blocker, which was incompletely effective, so he was started on proton pump inhibitor therapy. He currently takes 20 mg of omeprazole daily which is effective, but notes that if he misses a dose, he sometimes experiences heartburn. He denies dysphagia, nausea or vomiting, blood in his stool, or unintentional weight loss. He has no other chronic medical conditions and takes no other medications. He is a nonsmoker who drinks alcohol in moderation, and has no family history of gastrointestinal cancer. Noe hes having severe heartburn not responding to treatments. 1. 2. 3. 4. 5. 6. 7. What is relevant problem? Find out list of causes resulting in following condition? What set of investigations u want to run? What are diagnostic investigations and what they show? How would you manage this patient? What complications patients would be having currently? How would you manage these complications?