Pulmonary Embolism and COPD
advertisement

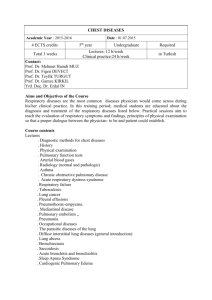
Pulmonary Embolism and COPD Fall Semester Pulmonary Embolism Obstruction of pulmonary artery or branch by blood clot (most common & usually arises from peripheral vein), air, fat, amniotic fluid, or septic thrombus Obstructed area has diminished or absent blood flow ◦ Although area is ventilated, no gas exchange occurs (dead space) Inflammatory process causes regional blood vessels, bronchioles to constrict, further increasing pulmonary vascular resistance, pulmonary arterial pressure, right ventricular workload Ventilation-perfusion imbalance, right ventricular failure, shock Risk Factors: Venous stasis: Prolonged immobility, Hypercoagulabilty Venous endothelial disease: DVT & thrombophlebitis Certain disease states: heart disease (HF), trauma (fracture of hip), postoperative (orthopedic, abdominal) /postpartum, diabetes mellitus (DM), COPD. Other conditions:Advance age (>50 years), pregnancy, obesity, oral contraceptive use, constrictive clothing, history of PE, DVT, & thrombophlebitis Review chart 23-8 page, 582 Clinical Manifestation: depend on the size of thrombus and the area occluded Dyspnea most frequent symptoms Tachypnea most frequent sign Chest pain (sudden, substernal, pleuritic in origin) Anxiety, fever, tachycardia, cough, apprehension, hemoptysis, diaphoresis and syncope Diagnostic Finding Death occurs within one hour CXR ( show infiltrate, atelectasis, elevation of diaphragm on the affected side, pleural effusion) ECG (sinus tachycardia, PR interval depression, ABG’s ( hypoxemia, hypocapnia from tachypnea) V\Q scan: second choice, evaluate different areas in the lungs and compare the V/Q in each area after IV administration of contrast agent and scan. Diagnostic Finding CT scan for the lung D-diamer assay: blood test for evidence of blood clot. ↑ indicates clotting abnormality such as (hypercoagulability) Pulmonary angiography, (first choice): injection of dye under fluoroscopy through a catheter that goes to vena cava (right side of the heart) to discover the thrombus Prevention ◦ Exercises to avoid venous stasis ◦ Early ambulation ◦ Anticoagulant therapy (heparin, and low molecular weight heparin: Enoxaparin) ◦ Sequential compression devices (SCDs) as elastic stocking: prevent venous stasis, ◦ Review chart 23-9 p 584. (Prevention of recurrent pulmonary embolism) Medical Management: Purpose to lyse the emboli and prevent new one from forming General measures to improve respiratory and vascular status Anticoagulant therapy: (Heparin and Warfarin) Thrombolytic therapy: ( streptokinase, urokinase) Check PTT, INR, HCT, & platelets count Surgical intervention: (embolectomy) done for Pts who fail to improve with medications or medications were contraindicated Nursing Management Minimize the risk of PE Preventing thrombus formation: - Early ambulation after surgery, - Leg exercises to avoid venous stasis, avoid dangling of legs, and feet should rest on floor. - Care of IV devices, Assessing potential of PE: risk factors Monitoring thrombolytic therapy Managing O2 therapy Relieving anxiety Providing post op care: VS, UO, elevation of legs, isometric exercise, elastic stocking, and avoid sitting to prevent hip flexion Monitoring for complications Chronic obstructive pulmonary disease, COPD A disease state characterized by airflow limitation that is not full reversible (GOLD: Global initiative for chronic obstructive lung disease). COPD is currently the 4th leading cause of death and the 12th leading cause of disability in US. COPD includes diseases that cause airflow obstruction (emphysema, chronic bronchitis) or a combination of these disorders. Asthma is now considered a separate disorder but can coexist with COPD. Pathophysiology Airflow limitation is progressive and associated with abnormal inflammatory response of the lungs to noxious agents or gases Inflammatory response occurs throughout the airways, lung parenchyma, and pulmonary vasculature. Scar tissue and narrowing occur in airways. Substances activated by chronic inflammation (proteinase and antiproteinase) damage the parenchyma of lungs. Inflammatory response causes changes in pulmonary vasculature. Chronic Bronchitis Cough with sputum production on most days for 3 months of a year for 2 consecutive years. Smoke and air pollutants irritation of airways results in inflammation and hypersecretion of mucus. Hallmark goblet cell and mucus glands increase in number & size Ciliary function is reduced (more mucus produced), bronchial walls thicken (due to infiltration of the bronchial wall with inflammatory cell), bronchial airways narrow, and mucus may plug airways Alveoli become damaged and fibrosed, and alveolar macrophage function diminishes. The patient is more susceptible to respiratory infections. Pathophysiology of Chronic Bronchitis Emphysema Abnormal distention of air spaces beyond the terminal bronchioles with destruction of alveoli walls Decreased alveolar surface area causes an increase in “dead space” & impaired O2 diffusion (hypoxemia). Reduction of the pulmonary capillary bed increases pulmonary vascular resistance and pulmonary artery pressures. Hypoxemia is the result of these pathologic changes. Increased pulmonary artery pressure may cause right-sided heart failure (cor pulmonale). Changes in Alveolar Structure with Emphysema Risk Factors for COPD (see chart 24-1, ) Tobacco smoke causes 80-90% of COPD cases! Passive smoking Occupational exposure Ambient air pollution Genetic abnormalities ◦ Alpha1-antitrypsin deficiency: enzyme that protect the lungs’ tissues from destruction Clinical Manifestation 1. 2. 3. 3 primary symptoms: Chronic cough Sputum production Dyspnea on exertion Wt loss Barrel chest (A-P diameter/ Transverse diameter : 2/1) Retraction in the supraclavicular area on inspiration Shrug shoulder Abdominal muscle contraction on inspiration. Typical Posture of a Person with COPD Diagnostic finding Health history (exposure to risk factor, past medical history, family Hx) Pulmonary function test Spirometry (FEV1\FVC) = <70% ABG’s (PaO2, PaCo2) hypoxemia CXR seldom used Screening for Alpha1-antitrypsin deficiency Medical Management Risk reduction especially smoking Pharmacologic therapy ( bronchodilators and corticosteroids) Management of exacerbation (worsening of the S&S) O2 therapy gradually because of hypercapnia Pulmonary rehabilitation Nursing Process Assessment: • Health history • Inspection and exam findings • See Chart 24-2 and Chart 24-3 • Review of diagnostic tests Nursing Process: The Care of Patients with COPD- Diagnoses Impaired gas exchange R\t V\Q inequality ineffective airway clearance R\t increased mucous secretion Ineffective breathing pattern R\t bronchospasm, mucus Activity intolerance R\t fatigue, hypoxemia Deficient knowledge regarding self care Ineffective coping R\t anxiety, lower activity level Collaborative Problems Respiratory insufficiency or failure Atelectasis Pulmonary infection Pneumonia Pneumothorax Pulmonary hypertension: Cor pulmonale- (Rt side heart failure) Planning Promote smoking cessation Improve gas exchange Maintain airway clearance Improve breathing pattern Improve activity tolerance Increase knowledge Enhance individual coping mechanism Improving Gas Exchange - Proper administration of bronchodilators and corticosteroids - Reduction of pulmonary irritants - Directed coughing (“huff” cough after deep breathing) - Chest physiotherapy - Breathing exercises to reduce air trapping ◦ Diaphragmatic breathing ◦ Pursed-lip breathing - Use of supplemental oxygen Improving Activity Tolerance Focus on rehabilitation activities to improve ADLs and promote independence. Pacing of activities Exercise training Walking aides Utilization of a collaborative approach Other Interventions Set realistic goals Avoid extreme temperatures Enhancement of coping strategies Monitor for and management of potential complications Patient Teaching Disease process Medications Procedures When and how to seek help Prevention of infections Avoidance of irritants; indoor and outdoor pollution and occupational exposure Lifestyle changes, including cessation of smoking Bronchiectasis and Asthma Chapter 24 Bronchiectasis - A chronic, irreversible dilation of the bronchi and bronchioles. Under the new definition of COPD, it is considered a separate disease process from COPD (NIH,2001). It may be caused by a variety of conditions, including: Airway obstruction Diffuse airway injury Pulmonary infections and obstruction of the bronchus or complications of long-term pulmonary infections Genetic disorders such as cystic fibrosis Abnormal host defense (eg, ciliary dyskinesia or humoral immunodeficiency) Idiopathic causes Pathophysiology The inflammatory process associated with pulmonary infections damages the bronchial wall, causing a loss of its supporting structure and resulting in thick sputum that ultimately obstructs the bronchi. The walls become permanently distended and distorted, impairing mucociliary clearance. The inflammation and infection extend to the peribronchial tissues; Bronchiectasis is usually localized, affecting a segment or lobe of a lung, most frequently the lower lobes. The retention of secretions and subsequent obstruction ultimately cause the alveoli distal to the obstruction to collapse (atelectasis). Inflammatory scarring or fibrosis replaces functioning lung tissue. In time the patient develops respiratory insufficiency with reduced vital capacity, decreased ventilation, and an increased ratio of residual volume to total lung capacity. There is impairment in the matching of ventilation to perfusion (ventilation–perfusion imbalance) and hypoxemia. Clinical Manifestations Characteristic symptoms of Bronchiectasis include: Chronic cough Production of purulent sputum in copious amounts. Many patients with this disease have hemoptysis. Clubbing of the fingers also is common because of respiratory insufficiency. Repeated episodes of pulmonary infection. Assessment and Diagnostic Findings Bronchiectasis is not readily diagnosed because the symptoms can be mistaken for those of simple chronic bronchitis. A definite sign is offered by the prolonged history of productive cough, with sputum consistently negative for tubercle bacilli. The diagnosis is established by a computed tomography (CT) scan, which demonstrates either the presence or absence of bronchial dilation. Medical Management Treatment objectives are to: - Promote bronchial drainage - Clear excessive secretions from the affected portion of the lungs - Prevent or control infection. Postural drainage: draining the Bronchiectasis areas by gravity reduces the amount of secretions and the degree of infection. Sometimes mucopurulent sputum must be removed by bronchoscopy. Chest physiotherapy, including percussion and postural drainage, is important in secretion management. Smoking cessation: smoking impairs bronchial drainage …by paralyzing ciliary action, increasing bronchial secretions, causing inflammation of the mucous membranes, & hyperplasia of the mucous glands. Infection is controlled: antimicrobial therapy (based on sensitivity studies & sputum culture). A year-round regimen of antibiotic agents (different types of antibiotics) may be prescribed at intervals. It may be prescribed throughout the winter (or when acute upper respiratory tract infections occur). Vaccination against influenza & pneumococcal pneumonia Bronchodilators: assist with secretion management. Surgery: to conserve normal pulmonary tissue & avoid complications Nursing Management Focuses on alleviating symptoms & to clear pulmonary secretions. Patient teaching: smoking & other factors that increase the production of mucus and hamper its removal Patient and family teaching: to perform postural drainage & to avoid exposure to others with upper respiratory or other infections. Teaching pt: early signs of respiratory infection & progression of disease (so appropriate treatment can be implemented promptly). Assess pt nutritional status, & teach pt strategies to ensure adequate diet and energy conservation