Mental Status
advertisement

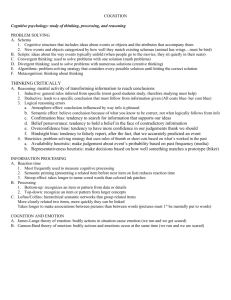
MENTAL STATUS EXAMINATION Outline • Operational definition • Purposes • Components – Behavior – Cognition – Emotion • Cognitive examination • Mini Mental Status MENTAL STATUS EXAMINATION: What is it? ASSESSMENT of the: • Behavior (see it all) • Emotion (see some of it) • Cognition (see none of it) Exhibited by the patient during the entire medical encounter PURPOSES • • • • Detect Describe Neuroanatomical localization Assess functional implications of Abnormalities/deficits in: • Behavior • Emotion • Cognition ABNORMALITIES & DEFICITS Require diagnostic explanation May compromise capacity • to coherently and reliably describe medical state • to give informed consent • to adhere to a therapeutic plan MEDICAL ENCOUNTER Comprehensive global assessment BEHAVIOR Appearance Attitude Activity Speech Dress Grooming Hygiene BEHAVIOR Appearance Attitude Activity Speech Dress Grooming Hygiene COGNITION Thought content Thought progression Insight/judgment BEHAVIOR Appearance Attitude Activity Speech Dress Grooming Hygiene COGNITION Thought content Coherence Goal directedness Insight/judgment Operations Arousal Attention Memory Emotion Language Reasoning BEHAVIOR Appearance Attitude Activity Speech Dress Grooming Hygiene COGNITION Thought content Coherence Goal directedness Insight/judgment Operations Arousal Attention Memory Emotion Language Reasoning EMOTION Affect Mood Suicide Homicide BEHAVIOR Appearance appears stated age, uses a cane to walk Attitude cooperative, hostile, detached Activity normal, increased, agitated, subdued Speech normal rate/rhythm, dysarthric Dress casual, provocative, dirty Grooming disheveled, meticulous Hygiene clean, malodorous COGNITIVE EXAM (“Mental status”) REASONING LANGUAGE MEMORY ATTENTION AROUSAL COGNITIVE EXAM (“Mental status”) Must know education REASONING LANGUAGE MEMORY ATTENTION AROUSAL Can the patient hear? MEMORY Immediate memory = attention Recent memory (episodic) Recall of three words at 5 minutes Ensure that pt has registered the items “Repeat these words after me, I want you to remember them.” Remote memory (semantic & episodic) Tends to overlap with knowledge, most of what we ask is overlearned Presidents, date of W.W.II, etc.. REASONING (Higher cognitive fx) Tests problem solving, abstract thinking Fund of knowledge - overlaps with remote memory How many weeks in a year? Name four presidents since 1940? What causes rust? Calculations Add, subtract, multiple, divide Sequences 1, 2, 3, ... 1, 4, 9, 16, .... 2, 3, 5, 7, 11, ... REASONING (continued) Similarities Apple - orange Car - airplane Poem - novel Proverbs Don’t cry over spilt milk A stitch in time saves nine People who live in glass houses shouldn’t throw stones BEHAVIOR Appearance Attitude Activity Speech Dress Grooming Hygiene COGNITION Thought content Thought progression Insight/judgment Arousal Attention Memory Language Reasoning EMOTION Affect Mood Suicide Homicide EMOTION AFFECT “Affect is to weather as mood is to climate” • predominate sad, euphoric, angry, anxious • intensity unmodulated • range narrow, broad • congruence incongruent with content MOOD euthymic, dysthymic, elated SUICIDE Do you ever wish you won’t wake up? Does it ever seem that life isn’t worth it? HOMICIDE Is there someone who deserves to be hurt? MEDICAL ENCOUNTER Comprehensive global assessment Focused selected assessment IN PRACTICE, MOST ENCOUNTERS ARE FOCUSED • Accordingly the formal mental status exam is often limited to an assessment of COGNITION • Further cognition is often assessed solely using: • ORIENTATION TO ORIENT To understand one’s relationship to the environment Person Place Time Situation “Oriented X 3” “O X3” Person Place Time Situation “Oriented X 3” “Oriented X 4” “O X3” “OX4” Person Place Time “Oriented X 3” “Oriented X 4” “O X3” “OX4” Situation ORIENTATION ASSESSES: • • • • • language perception reasoning remote memory recent memory Less precise Less comprehensive Shorter Examiner norms More precise More comprehensive Longer Statistical norms Mini Mental Status Orientation Full mental status Neuropsychological Testing MINI MENTAL STATE EXAM ADVANTAGES • brief (10 min), systematic bedside instrument • wide recognition among physicians • since it is standardized, the score it yields is meaningful to physicians familiar with it DISADVANTAGES • specific deficits may be ignored if the overall score is not low (less than 25 out of 30) • the global score has no localizing valve • repeated use with intact patients produces a mechanical transaction • Examiner uses paper and pencil • Total of 30 points orientation (10) recent memory (3) attention (3) calculation, spell backward (5) name, read, repeat (4) write (1) constructional ability (1) ideomotor praxis (3) • Not timed What is the (year) (season) (date) (day) (month)? Where are we? (state) (county) (city) (hospital) (floor)(10) Ask pt to repeat three objects - give one per second. Number repeated first trial = score (3). Present till all repeated or 6 presentations. Serial 7’s - 5 subtractions (93, 86, 79, 72, 65) (5). Score number of correct answers or spell “world” backward, score is number of letters in correct order. “dlorw” is 3 points. Ask the patient to name a watch and a pencil. (2) Ask the patient to say “No ifs, ands or buts” (1). Ask the patient to recall the three words (3). Ask the pt to read and follow the command: “Close your eyes”. Score (1 ) only if closes eyes. Ask the pt to write a sentence. It must have a subject and a verb and be sensible. Ignore grammar and punctuation (1). Place a piece of paper where the patient can reach it with either hand. Ask him/her to: (1) pick it up, (2) fold it in half, (3) lay it on the floor. 1 pt for each step executed correctly (3). Ask the patient to copy a drawing of intersecting pentagons. All 10 angles must be present and two must intersect to create a 4 sided figure. Ignore tremor and rotation (1). Normals can be expected to score > 25 However, even with > 25, if 0/3 or 1/3 for recent memory or problems with naming, repeating, writing or reading suggest focal deficits. It is most sensitive to disturbances which broadly effect function, it may miss subtle, focal problems. You may not always do a MMS: •Too little time •Patient becomes agitated at challenge However, even without an MMS Interacting with the patient and obtaining a history have provided information to write up a mental status exam Lesson: YOU DO NOT HAVE TO DO AN MMS TO THOROUGHLY EXAM A PT