OBS and GYN orders - Medical Education Online
advertisement

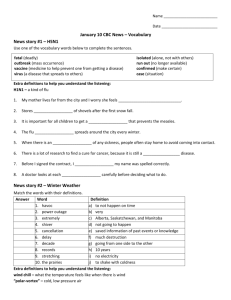
Sample Obstetrics Orders By: Mitra Ahmad Soltani References: 1-Williams Obstetrics / 22nd Edition/ MC. Graw Hill/ 2005 2-Novak’s Gynecology/ 13 th Edition/ Williams and Wilkins/ 2002 3-TE Linde’s (Operative Gynecology) 9 th Edition / Williams and Wilkins / 2003 4-Iranian Council for Graduate Medical. Education. Promotion and board Exam questions.(2000-2007) 5- www.cdc.gov/asthma/speakit/slides/managing_asthma.ppt 6- An extract from Tan T& Yeo G. IUGR. Current Opinion in Obstetrics and Gynecology 2005, 17: 135-142 7-Panda S . IUGR. Department of Obstetrics & Gynecology Medical College of India 2002 8-med-ed-online.org/rcurricula/med_decision_making. med-ed-online 2008 Recommended laboratory tests in the initial prenatal care visit 1. 2. 3. 4. 5. 6. 7. 8. 9. Hct, Hb U/A,U/C BG,Rh Pap smear Antibody screen Rubella status Syphilis screen Hbs Ag Offer HIV testing med-ed-online 2008 Impression: normal labor • General: condition/position/diet • Lab: CBC, BG, Rh, U/A, reserve of 2 units of PC • IV : 1000cc Ringer at KVO for long labors 1/3,2/3 60-120mL/h • PO:• OTHER: Control of vital sign q4hrs, control of FHR q30 min in 1st stage of labor q15 min in the 2nd stage, amniotomy if fetal head is fix med-ed-online 2008 Impression: NVD+Epi • • • • General: condition/position/diet Lab: F/U CBC IV : 1000cc Ringer +20 units of oxytocin PO: cap cephalexin 500 mg qid Tab ferrus sulfate daily, cap mefenamic acid TDS • OTHER: Control of vital sign q15 min for the1st hr then q1hr for 4 hrs then as routine • Inform if BP is abnormal/bleeding is excessive/ no voiding after 4 hrs med-ed-online 2008 7 contraindications for lactation • • • • • • • Alcohol and Drug abusers Galactosemia of the newborn HIV Active, untreated TB Ongoing breast cancer treatment Cytomegalovirus Hepatitis B virus (not contraindicated if hepatitis B immune globulin is given to infants of seropositive mothers) med-ed-online 2008 10 drugs contraindicated in lactation • • • • • • • • Bromocriptine Cocaine Cyclophosphamide Cyclosporine Doxorubicin Lithium Methotrexate Phencyclidine • phenindione • Radioactive iodine and other radiolabled elements med-ed-online 2008 IMP:Mastitis (out patient) • Lab:, Milk culture , CBC diff • PO: dicloxacillin 500 mg qid 7-10 days • Or erythromycin to penicillin sensitive women • Or vancomycin to MRS • OTHER: Control of vital sign q 4 hrs, pumping breasts until nursing can be resumed med-ed-online 2008 Postoperative infection • General: condition/position/diet • Lab: CBC diff, MP, WW, B/C X2, U/A , U/C,CXR,BUN/Cr • IV : 1000cc Ringer at KVO AMP clindamycin 900 mg iv TDS +gentamicin im 80mg stat then 60 mg TDS add amp ampicillin 2gr iv qid and pelvic exam and imaging study if fever persists 72 hours, OTHER: Control of vital sign hourly med-ed-online 2008 Imp:chorioamnionitis • General: condition/position/diet=NPO • Lab: CBC diff, MP, WW, B/C X2, U/A , U/C,CXR,BUN/Cr • IV : 1000cc Ringer +10 units of oxytocin start at 2 drops /min, add 4 drops every 15 min if FHR and contractions are normal Amp ampicillin 2gr iv qid +gentamicin im 80mg stat then 60 mg TDS AMP clindamycin 900 mg iv TDS for allergic women to penicillin(continue antibiotics after delivery until the mother is a febrile OTHER: Control of vital sign hourly med-ed-online 2008 Sepsis syndrome • General: condition/position/diet • Lab: CBC diff, hct, MP, WW, B/C X2, U/A , U/C , CXR, BUN/Cr • IV : AMP clindamycin 900 mg iv TDS +gentamicin im 80mg stat then 60 mg TDS add amp ampicillin 2gr iv qid and pelvic exam and imaging study if fever persists 72 hours Amp dopamine 5 mcg/kg/min or dubotamine iv drip OTHER: Control of vital sign hourly ,oxygen therapy, correct acidosis, excise infected tissue, fix foley , med-ed-online 2008 Low output cardiogenic shock-1 SBP<70 mmHg +sign/symptoms of shock: Noreinephrine IV 0.5 to 30 mcg/min med-ed-online 2008 Low output cardiogenic shock-2 SBP=100-70+sign/symptoms of shock: DOPAMINE: 5-15 mcg/kg/min IV med-ed-online 2008 Low output cardiogenic shock-3 SBP=100-70 no sign/symptoms of shock: Dobutamine: 2-20 mcg/kg/min IV med-ed-online 2008 Low output cardiogenic shock-4 SBP>100 NTG=10-20 mcg/min IV Consider SNP: 0.1-5 mcg/kg/min IV ACEinh. if SBP is not<30 mmHg below baseline. med-ed-online 2008 Glasgow Coma Scale med-ed-online 2008 Eye 3 To Voice Opening 4 Spontaneous 2 To Pain 1 Nil Verbal 4 Response 5 Confused Orientated 3 Words 2 Groans Motor 5 Response 6 Localizes Pain Obeys Commands 4 3 Withdraws Flex from Pain med-ed-online 2008 1 Nil 2 Ext 1 Nil IMP: R/O abruption • • • • • Condition/position/diet:NPO Lab: CBD-BG-Rh-U/A-U/C-PT-PTT-Fib-FDP-D-DimerPrep 4 units of crossmatched packed red blood cells Continuous high-flow supplemental oxygen One or 2 large-bore IV lines with normal saline (NS) or lactated Ringer (LR) solution+10 units of oxytocin in 1 lit of ringer start at 2 drops/min add 2 drops every 15 min if fetal heart rate and uterine contractions are favorable. • perform amniotomy • Closely observe the patient. Monitor vital signs and urine output, fetal heart rate and uterine height measurement. • Prepare OR for emergent C/S med-ed-online 2008 Class 1 Class 2 Class 3 Class 4 Blood Loss Volume (mls) in adult 750mls 800 - 1500mls 1500 - 2000mls >2000mls Blood Loss % Circ. blood volume <15% 15 - 30% 30 - 40% >40% Systolic Blood Pressure No change Normal Reduced Very low Diastolic Blood Pressure No change Raised Reduced Very low / Unrecordable Pulse (beats /min) Slight tachycardia 100 - 120 120 (thready) >120 (very thready) Capillary Refill Normal Slow (>2s) Slow (>2s) Undetectable Respiratory Rate Normal Normal Raised (>20/min) Raised (>20/min) Urine Flow (mls/hr) >30 20 - 30 med-ed-online 2008 10 - 20 0 - 10 Estimated blood loss Suitable fluid regimes 1000 mls 3000 mls crystalloid o r 1000 mls colloid 1500 mls 1500 mls crystalloid & 1000mls colloid o r 4500 mls crystalloid 2000 mls 1000 mls crystalloid, 1000mls colloid & 2 units blood o r 3000 mls crystalloid & 2 units blood med-ed-online 2008 Infection Suggested oral adult dose Price Acute cystitis Trimethoprim 200 mg bd or Augmentin 625 mg tid or Nitrofurantoin 50 mg qid Nalidixic acid 500 mg qid TRIMETHOPRIM 100MG TAB= 66 Rls. CO-AMOXICLAV 625 (500/125) TAB = 2,970 Rls. NITROFURANTOIN 100MG TAB = 57 Rls. Acute pyelonephritis (pre- hospital admission) Ciprofloxacin 750 mg bd CIPROFLOXACINEXIR® 250MG TAB = 350 Rls. med-ed-online 2008 PE med-ed-online 2008 Is PaCO2 increased? Is PAO2-PaO2 increased? Yes=hypoventilation Is PAo2-PaO2 increased? Hypoventilation alone Decreased inspired PO2 Yes=hypoventilation +another mechanism If yes then find out if low PO2 is correctable with O2? Yes=V/Q mismatch med-ed-online 2008 Shunt ABG reading med-ed-online 2008 med-ed-online 2008 Check if the blood is from an artery (CO2=15+HCO3) Calculate Anion Gap (AG=Na – (Cl +HCO3) Calculate if the response is compensatory or not If there’s no significant AG (more than10-12), then it must be either RTA or GI loss. In GI loss this formula med-ed-online 2008 applies => Urinary Cl>Urinary Na +K PE, DVT • IV heparin 5000 unit q4h • Check of PTT Q6h • Discharge with warfarin 5 mg /day for 4-6 months med-ed-online 2008 PTT (sec) Heparin Dosing Instructions Recheck PTT Repeat Bolus Dose Hold Infusion Change Rate of Infusion units minutes ml/h (units/h) 50 - 59 0 0 +2 cc/h (+80 u/h) 6h 60 - 85 0 0 no change next am 86 - 110 0 0 -2 cc/h (- 80 u/h) next am < 50 5000 0 +4 cc/h (+160 u/h) 6h >110 0 60 2008 med-ed-online -4 cc/h (- 160 u/h) 6h IMP:PLP before 37 weeks out patient: (contractions 4 in 20 min or 8 in 60 min +progressive change in cervix cervical dilation of more than one cervical effacement of more than 80 % or greater) if: Check of contractions:+ U/A, U/C: Fern:Then: Hydrate and sedate Stop of contractions: discharge With:isoxsuprine 10 mg TDS for 10 days Contractions persist: hospitalize Next slide med-ed-online 2008 IMP:PLP before 37 weeks, hospitalized • General: condition/position/diet • Lab: CBC, BG, Rh, U/A, U/C, fern, reserve of 2 units of PC • IV : 1-1000cc Ringer free 2-MgSO4 (4 gr) in 200cc DW5% in 20 min then 20 gr in 1000cc infused in 100cc/hrs (check of I/O, RR,DTR, prep CPR set- I/O with measure) 3-Amp pethidine 25 mg iv 25 mg im 4-Amp ampicillin 2 gr IV qid 5-Amp erythromicin 400 mg QID 6- Amp betamethasone 12 mg im, repeat after 24 hrs for GA below 34 wks • OTHER: Control of vital sign q4hrs, Inform if LP, leakage, VB, ab VS or FHR med-ed-online 2008 Contraindication to tocolysis • • • • • • Acute fetal distress Chorioamnionitis Eclampsia or sever preeclampsia Fetal demise Fetal maturity Maternal hemodynamic instability med-ed-online 2008 Contraindication for beta mimetics Maternal • cardiac disease • Diabetes • Thyrotoxicosis • HTN med-ed-online 2008 Contraindication for MgSO4 • Hypocalcemia • Myasthenia gravis • Renal failure med-ed-online 2008 Contraindication for indomethacin • • • • • • Asthma CAD Gastrointestinal bleeding Oligohydramnios Renal failure Suspected fetal cardiac or renal anomaly med-ed-online 2008 Dosage of Ritodrine or Terbutaline for tocolysis • 50-100 mcg/min increase by 50 mcg/min every 10 min • max dose:350mcg/min If labor is arrested continue the infusion for at least 12 hrs • SC: 250 mcg q3-4 hrs med-ed-online 2008 Endocarditis Prophylaxis med-ed-online 2008 GI or GU surgery High Risk patient Standard Ampicillin +Gentamycin 30 min before the procedure and have to be repeat Ampicillin after 6 hours Moderate Risk Allergy Standard Gentamycine + Vancomycine Amoxycillin med-ed-online 2008 Allergy Vancomycine Should be infused One hour before to 30 minutes after the procedure IMP: Hyperemesis Gravidarum • General: condition/position/diet • Lab: CBC, BG,Rh, U/A, U/C, k, Na, BUN/Cr, TFT • reserve of 2 units of PC • IV : 3000cc(DW10%+ DW5%+1/3,2/3)divided in 24 hrs • AMP Promethazine 25 mg iv qid • Amp plazil 10 mg qid • Tab navidoxin daily • OTHER: Control of vital sign q4hrs, daily weight, check of I/O with measure sono OB med-ed-online 2008 Suspecting Acute Hepatitis • • • • HBS Ag, Ab Anti HBC (IgM) ANTI HAV (IgM) Anti HCV med-ed-online 2008 Suspecting Chronic Hepatitis • HBe Ag, Ab • HBS Ag ,Ab • Anti HCV med-ed-online 2008 IMP: Pyelonephritis • General: condition/position/diet • Lab: CBC diff, BG, Rh, U/A,U/C, k, Na, BUN/Cr, WW, MP,B/CX2 (Repeat of U/C after initiation of antibiotics if positive then kidney sono) • reserve of 2 units of PC • IV : 1000cc DW5% free • AMP keflin 2 gr stat then 1 gr q6h • Amp gentamicin 80 mg im stat then 60 mg tds • OTHER: Control of vital sign q4hrs, control of FHR,FAD chart , check of I/O with measure, sono OB med-ed-online 2008 GFR=(140-age)/72x PCr x 85% for females med-ed-online 2008 Blood sugar • For pregnancy Ab>105 FBS Ab>120 2hr PP POSTPARTUM Ab>140 FBS Ab>200 2hr PP med-ed-online 2008 IMP: Diabetes • General: condition/position/diet =diabetic • Lab: CBC diff ,BG, Rh, U/A,U/C, BUN/Cr, BS(FBS, 10AM,4 PM,8PM), (PT, PTT, Fib) (reserve of 2 units of PC • IV :Ringer at heparin lock • Insulin morning (10 units NPH +4 Reg) • Insulin afternoon(4 NPH+4 Reg) • OTHER: Control of vital sign q4hrs, control of FHR, FAD chart , NST, sono OB, ophthalmologic consultation med-ed-online 2008 • For each increase in BS more than 200 add 2 units to regular to each 50 mg of BS • Insulin is used before breakfast and evening meal med-ed-online 2008 IMP: mild preeclampsia • General: condition/position/diet =low salt,high prot • Lab: CBC ,BG, Rh, U/A,24hr urine (prot,cr,vol), BUN/Cr, PT,PTT,Fib, ALT,AST,Al P, Bil (T, D) • reserve of 2 units of PC • IV :Ringer at heparin lock • OTHER: Control of vital sign q4hrs, control of FHR, FAD chart , NST, sono OB, daily weight inform if BP>160/110, blurred vision, head ache, epigastric pain, seizure med-ed-online 2008 IMP: Severe preeclampsia • • • • • General: condition/position/diet =NPO Lab: CBC ,BG, Rh, BUN/Cr, PT, PTT,Fib ,ALT,AST,Al P, Bil (T, D) prep 2 units of PC IV :Ringer 1000cc +10 u of oxytocin if BP>160/110,blurred vision, head ache, epigastric pain, seizure then amp hydralazine 5 mg iv prn MgSO4 (4 gr) in 200cc DW5% in 20 min then 10 gr(1/2) im in each buttock then 5 gr im q4h If platelet is below 100000 then 20 gr in 1000cc infused in 100cc/hrs (check of I/O,RR,DTR, prep CPR set with 2 gr 20% MgSO4 ready) +Amp Dexa 6 mg im bid for 4 doses OTHER: Control of vital sign q15 min , control of FHR, fix foley, med-ed-online 2008 Emergency C/S • • • • Prep 2 units of pc Amp keflin 2 gr iv Prepare for C/S Transfer to OR med-ed-online 2008 The night before elective C/S • • • • • CBC, BG, Rh, (FBS,BUN/CR, CXR, ECG) Prep 2 units of pc NPO from 12 am Iv Ringer KVO Check of FHR and contractions med-ed-online 2008 8 hours after C/S • • • • fair, RBR, surgical diet, IV 2 lit Ringer Continue keflin Supp bisacodyl 2 stat then tab bisacodyl bid • Foley DC, • I/O DC • F/U CBC med-ed-online 2008 24 hours after C/S • • • • Condition good ,RBR, reg diet, IV as heparin lock Continue keflin tab bisacodyl bid med-ed-online 2008 36-48 hours after C/S • Remove dressing • Discharge with Cap cephalexin 500 mg qid Cap mefenamic acid 500 mg tds Cap hematinic (according to Hb) med-ed-online 2008 Diabetic C/S NPO from 12 am Prep 2 units of PC 1000 cc Ringer IV fluid q8 hrs the night before surgery Amp keflin 2 gr iv stat half an hour before surgery • Before operation: 10 units of regular +1000 cc DW5% 150cc/hr • Check of BS q6h after operation Inform in cases of ROM or bleeding or pain med-ed-online 2008 Asthma management med-ed-online 2008 med-ed-online 2008 Heavy vaginal bleeding in a 14 year old girl with Hb value of 7 gr/dl and normal coagulation tests and platelets and pelvic sonography: Conjugate estrogen 25-40 mg IV q6h or Conjugated estrogen 2.5 mg q6h PO until bleeding is controlled followed by medroxy progesterone med-ed-online 2008 Prolonged spotting in a 14 year old anemic girl Low dose OCP 21 days for 3-6 cycles med-ed-online 2008 DUB in a 16 year old girl with stable vital signs: Monophasic OCP q6h for 7 days + Iron supplements med-ed-online 2008 Recurrent abortion tests • • • • • • • Karyotype HSG Luteal phase biopsy of endometrium TSH and prolactin level ACL ab LAC CBC med-ed-online 2008 Abortion without fever: Doxy 100 mg bid or tetracycline 250 mg qid for 5-7 days med-ed-online 2008 Beta HCG below 2000+ no visible intrauterine sac+ mass in tube below 3.5 cm ______________________ control of beta HCG q 48 h A-If a dead IP is confirmed (beta HCG increase less than 50% or below 1000mIu/mL- P below 5 ng/mL + visible intrauterine sac) then curettage B-If EP is confirmed (beta HCG more than 2000 and mass >3.5 cm) then laparascopy C-If a dead IP and EP is confirmed (beta HCG more than 2000 and mass < 3.5 cm) then MTX FETUS SHOULD BE VISIBLE ON DAY 45 OF GESTATION med-ed-online 2008 Indication of MTX for EP • Hemodynamic stability • No intra uterine pregnancy • Max sac diameter not equal or more than 4 cm med-ed-online 2008 EP • Adenexal mass< 3.5 cm-> MTX • adenexal mass=> 3.5 cm -> laparascopy • uncertain US + beta HCG increase less than 50% -> D&C • unstable conditions->laparatomy med-ed-online 2008