Nutrition

Nutrition
. . . and the surgical patient
Carli Schwartz, RD/LDN
Nutrition and Surgery
Malnutrition may compound the severity of complications related to a surgical procedure
A well-nourished patient usually tolerates major surgery better than a severely malnourished patient
Malnutrition is associated with a high incidence of operative complications and death.
Normal Nutrition
(EatRight.org)
Nutrition
Carbohydrates
Limited strorage capacity, needed for CNS
(glucose) function
Yields 3.4 kcal/gm
Recommended 45-65% total daily calories.
Nutrition
Fats
Major endogenous fuel source in healthy adults
Yields 9 kcal/gm
Too little can lead to essential fatty acid
(linoleic acid) deficiency and increased risk of infections
Recommended 20-30% of total caloric intake
Nutrition
Protein
Needed to maintain anabolic state (match catabolism)
Yields 4 kcal/gm
Must adjust in patients with renal and hepatic failure
Recommended 10-35% of total caloric intake.
Normal Nutrition
Requirements
HEALTHLY male/female
(weight maintenance)
• Caloric intake=25-30 kcal/kg/day
• Protein intake=0.8-1gm/kg/day
(max=150gm/day)
• Fluid intake=~ 30 ml/kg/day
Nutrition
Requirements
? SURGICAL PATIENT ?
Special considerations
Stress
Injury or disease
Surgery
Pre-hospital/presurgical nutrition
Nutrition history
The surgical patient . . . .
Increased risk of malnutrition due to:
Inadequate nutritional intake
surgical stress
subsequent increase in metabolic rate.
Extraordinary stressors (hypovolemia, bacteremia, medications)
Wound healing
Anabolic state, appropriate vitamins
Poor nutrition=poor outcomes
For every gm deficit of untreated hypoalbuminemia there is ~ 30% increase in mortality
Nutrition
HEALTHLY 70 kg MALE
Caloric intake
25-30 kcal/kg/day
Protein intake
0.8-1gm/kg/day
(max=150gm/day)
Fluid intake
30 ml/kg/day
SURGERY PATIENT
Caloric intake
*Mild stress, inpatient
25-30 kcal/kg/day
*Moderate stress, ICU patient
30-35 kcal/kg/day
*Severe stress, burn patient
30-40 kcal/kg/day
Protein intake
1-2 gm/kg/day
Fluid intake
INDIVIDUALIZED
Measures of success: serum markers
Albumin
Synthesized in and catabolized by the liver
Pro: often ranked as the strongest predictor of surgical outcomes- inverse relationship between postoperative morbidity and mortality compared with preoperative serum albumin levels
Con: lack of specificity due to long half-life
(approximately 20 days).
Normal range: 3.5-5 g/dL.
The National Veterans Affairs Surgical Risk Study evlauated 87,000 noncardiac surgeries in 44 Veteran’s
Administration medical centers and found preoperative serum albumin to the bet strongest predictor of postoperative mortality
Measures of success: serum markers (cont’d)
Prealbumin (transthyretin) - transport protein for thyroid hormone, synthesized by the liver and partly catabolized by the kidneys.
Normal range:16 to 40 mg/dL; values of <16 mg/dL are associated with malnutrition.
Levels may be increased in the setting of renal dysfunction, corticosteroid therapy, or dehydration, whereas physiological stress, infection, liver dysfunction, and overhydration can decrease prealbumin levels.
[8,30,37]
Pro: Shorter half life (two to three days) making it a more favorable marker of acute change in nutritional status. A baseline prealbumin is useful as part of the initial nutritional assessment if routine monitoring is planned.
Cons: More expensive than albumin.
Reasonable goal would be to increase prealbumin by 3-5 mg/dL/wk until values are within normal limits.
[ This goal would be valid only in the absence of other factors that can influence prealbumin
(Elevated concentrations of C-reactive protein (>10 mg/dL) suggest physiological stress that requires continued hepatic synthesis of acute-phase reactants and delays production of markers of nutritional rehabilitation, such as prealbumin. Until this stress response subsides, practitioners may not see improvement in prealbumin levels no matter how much nutrition is being provided)
Measures of success: serum markers (cont’d)
Transferrin: acute-phase reactant and a transport protein for iron
normal range: 200 to 360 mg/dL.
Medium half-life (8-10 days)
influenced by several factors, including liver disease, fluid status, stress, and illness.
Levels decrease in the setting of severe malnutrition, however unreliable in the assessment of mild malnutrition,
Cons: not studied extensively as albumin and prealbumin in relation to nutritional status, can be expensive.
Other measures of success
Nitrogen balance
Protein ~ 16% nitrogen
Protein intake (gm)/6.25 - (UUN +4)= balance in grams
Positive value: found during periods of growth, tissue repair or pregnancy. This means that the intake of nitrogen into the body is greater than the loss of nitrogen from the body, so there is an increase in the total body pool of protein.
Negative value: can be associated with burns, fevers, wasting diseases and other serious injuries and during periods of fasting. This means that the amount of nitrogen excreted from the body is greater than the amount of nitrogen ingested.
Healthy Humans= Nitrogen Equilibrium
Metabolic cart (indirect calorimetry)
ICU patient, measure of exchange of O2 and CO2
Respiratory quotient =1
Postoperative Nutritional Care
Traditional Method: Diet advancement
Introduction of solid food depends on the condition of the GI tract.
Oral feeding delayed for 24-48 hours after surgery
Wait for return of bowel sounds or passage of flatus.
Start clear liquids when signs of bowel function returns
Rationale
Clear liquid diets supply fluid and electrolytes that require minimal digestion and little stimulation of the
GI tract
Clear liquids are intended for short-term use due to inadequacy
Things to Consider…
For liquid diets, patients must have adequate swallowing functions
Even patients with mild dysphagia often require thickened liquids.
Must be specific in writing liquid diet orders for patients with dysphagia
There is no physiological reason for solid foods not to be introduced as soon as the GI tract is functioning and a few liquids are being tolerated. Multiple studies show patients can be fed a regular solid-food diet after surgery without initiation of liquid diets.
Diet Advancement
Advance diet to full liquids followed by solid foods, depending on patient’s tolerance.
Consider the patient’s disease state and any complications that may have come about since surgery.
Ex: steroid-induced diabetes in a post-kidney transplant patient.
Patients who cannot eat . . . ?
Consider Nutrition Support!
Nutrition Support
Length of time a patient can remain NPO after surgery without complications is uknown, however depends on:
Severity of operative stress
Patient’s preexisting nutritional status
Nature and severity of illness
Two types of nutritional support
Enteral
Parenteral
What is enteral nutrition?
Enteral Nutrition
Also called "tube feeding," enteral nutrition is a liquid mixture of all the needed nutrients.
Consistency is sometimes similar to a milkshake.
It is given through a tube in the stomach or small intestine.
If oral feeding is not possible, or an extended
NPO period is anticipated, an access devise for enteral feeding should be inserted at the time of surgery.
Indications for Enteral
Nutrition
Malnourished patient expected to be unable to eat adequately for > 5-7 days
Adequately nourished patient expected to be unable to eat > 7-9 days
Adaptive phase of short bowel syndrome
Following severe trauma or burns
Contraindications to Enteral
Nutrition Support
Malnourished patient expected to eat within 5-7 days
Severe acute pancreatitis
High output enteric fistula distal to feeding tube
Inability to gain access
Intractable vomiting or diarrhea
Aggressive therapy not warranted
Expected need less than 5-7 days if malnourished or 7-9 days if normally nourished
Enteral Access Devices
Nasogastric
Nasoenteric
Gastrostomy
PEG (percutaneous endoscopic gastrostomy)
Surgical or open gastrostomy
Jejunostomy
PEJ (percutaneous endoscopic jejunostomy)
Surgical or open jejunostomy
Transgastric Jejunostomy
PEG-J (percutaneous endoscopic gastro-jejunostomy)
Surgical or open gastro-jejunostomy
Feeding Tube Selection
Can the patient be fed into the stomach, or is small bowel access required?
How long will the patient need tube feedings?
Gastric vs. Small Bowel
Access
“If the stomach empties, use it.”
Indications to consider small bowel access:
Gastroparesis / gastric ileus
Recent abdominal surgery
Sepsis
Significant gastroesophageal reflux
Pancreatitis
Aspiration
Ileus
Proximal enteric fistula or obstruction
Short-Term vs. Long-Term
Tube Feeding Access
No standard of care for cut-off time between short-term and long-term access
However, if patient is expected to require nutrition support longer than 6-8 weeks, longterm access should be considered
Choosing Appropriate
Formulas
Categories of enteral formulas:
Polymeric
Whole protein nitrogen source, for use in patients with normal or near normal GI function
Monomeric or elemental
Predigested nutrients; most have a low fat content or high % of
MCT; for use in patients with severely impaired GI function
Disease specific
Formulas designed for feeding patients with specific disease states
Formulas are available for respiratory disease, diabetes, renal failure, hepatic failure, and immune compromise
* well-designed clinical trials may or may not be available
Tulane Enteral Nutrition
Product Formulary
Enteral Nutrition Prescription
Guidelines
Gastric feeding
Continuous feeding:
Start at rate 30 mL/hour
Advance in increments of 20 mL q 8 hours to goal
Check gastric residuals q 4 hours
Bolus feeding:
Start with 120 mL bolus
Increase by 60 mL q bolus to goal volume
Typical bolus frequency every 3-8 hours
Small bowel feeding
Continuous feeding only; do not bolus due to risk of dumping syndrome
Start at rate 20 mL/hour
Advance in increments of 20 mL q 8 hours to goal
Do not check gastric residuals
Aspiration Precautions
To prevent aspiration of tube feeding, keep
HOB > 30 ° at all times
Use of blue dye to test for aspiration is controversial and has been discontinued in practice.
Discoloration
Falslely positive reading on guaiac tests
Reported deaths
Complications of Enteral
Nutrition Support
Issues with access, administration, GI complications, metabolic complications.
These include:
Nausea, vomitting, diarrhea, delayed gastric emptying, malabsorption, refeeding syndrome, hyponatremia, microbial contamination, tube obstruction, leakage from ostomy/stoma site, micronutrient deficiencies.
Enteral Nutrition Case Study
78-year-old woman admitted with new CVA
Significant aspiration detected on bedside swallow evaluation and confirmed with modified barium swallow study; speech language pathologist recommended strict NPO with alternate means of nutrition
PEG placed for long-term feeding access
Plan of care is to stabilize the patient and transfer her to a long-term care facility for rehabilitation
Enteral Nutrition Case Study
(continued)
Height: 5’4” IBW: 120# +/- 10%
Weight: 130# / 59kg 100% IBW
BMI: 22
Usual weight: ~130# no weight change
Estimated needs:
1475-1770 kcal (25-30 kcal/kg)
59-71g protein (1-1.2 g/kg)
1770 mL fluid (30 mL/kg)
Steps to determine the
Enteral Nutrition Prescription
3.
4.
1.
2.
5.
Estimate energy, protein, and fluid needs
Select most appropriate enteral formula
Determine continuous vs. bolus feeding
Determine goal rate to meet estimated needs
Write/recommend the enteral nutrition prescription
Enteral Nutrition Prescription
Tube feeding via PEG with full strength
Jevity 1.2
Initiate at 30 mL/hour, advance by 20 mL q 8 hours to goal
Goal rate = 55 mL/hour continuous infusion
Above goal will provide 1584 kcal, 73g protein, 1069 mL free H
2
O
Give additional free H
2
O 175 mL QID to meet hydration needs and keep tube patent
Check gastric residuals q 4 hours; hold feeds for residual > 200 mL
Keep HOB > 30 ° at all times
What is parenteral nutrition?
Parenteral Nutrition
also called "total parenteral nutrition," "TPN," or
"hyperalimentation."
It is a special liquid mixture given into the blood via a catheter in a vein.
The mixture contains all the protein, carbohydrates, fat, vitamins, minerals, and other nutrients needed.
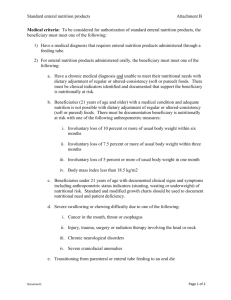
Indications for Parenteral
Nutrition Support
Malnourished patient expected to be unable to eat > 5-7 days AND enteral nutrition is contraindicated
Patient failed enteral nutrition trial with appropriate tube placement (post-pyloric)
Enteral nutrition is contraindicated or severe
GI dysfunction is present
Paralytic ileus, mesenteric ischemia, small bowel obstruction, enteric fistula distal to enteral access sites
PPN vs. TPN
TPN (total parenteral nutrition)
High glucose concentration (15%-25% final dextrose concentration)
Provides a hyperosmolar formulation (1300-1800 mOsm/L)
Must be delivered into a large-diameter vein
PPN (peripheral parenteral nutrition)
Similar nutrient components as TPN, but lower concentration (5%-10% final dextrose concentration)
Osmolarity < 900 mOsm/L (maximum tolerated by a peripheral vein)
May be delivered into a peripheral vein
Because of lower concentration, large fluid volumes are needed to provide a comparable calorie and protein dose as TPN
Parenteral Access Devices
Peripheral venous access
Catheter placed percutaneously into a peripheral vessel
Central venous access (catheter tip in SVC)
Percutaneous jugular, femoral, or subclavian catheter
Implanted ports (surgically placed)
PICC (peripherally inserted central catheter)
Writing TPN prescriptions
5.
6.
7.
1.
2.
3.
4.
Determine total volume of formulation based on individual patient fluid needs
Determine amino acid (protein) content
Adequate to meet patient’s estimated needs
Determine dextrose (carbohydrate) content
~70-80% of non-protein calories
Determine lipid (fat) content
~20-30% non-protein calories
Determine electrolyte needs
Determine acid/base status
Check to make sure desired formulation will fit in the total volume indicated
Tulane Daily Parenteral
Nutrition Order Form
Parenteral Nutrition
Monitoring
Check daily electrolytes and adjust TPN/PPN electrolyte additives accordingly
Check accu-check glucose q 6 hours
(regular insulin may be added to TPN/PPN bag for glucose control as needed)
Nondiabetics or NIDDM: start with half of the previous day’s sliding scale insulin requirement in TPN/PPN bag and increase daily in the same manner until target glucose is reached
IDDM: start with 0.1 units regular insulin per gram of dextrose in
TPN/PPN, then increase daily by half of the previous day’s sliding scale insulin requirement
Check triglyceride level within 24 hours of starting
TPN/PPN
If TG >250-400 mg/dL, lipid infusion should be significantly reduced or discontinued
Consider adding carnitine 1 gram daily to TPN/PPN to improve lipid metabolism
~100 grams fat per week is needed to prevent essential fatty acid deficiency
Parenteral Nutrition
Monitoring
(continued)
Check LFT’s weekly
If LFT’s significantly elevated as a result of TPN, then minimize lipids to < 1 g/kd/day and cycle TPN/PPN over 12 hours to rest the liver
If Bilirubin > 5-10 mg/dL due to hepatic dysfunction, then discontinue trace elements due to potential for toxicity of manganese and copper
Check pre-albumin weekly
Adjust amino acid content of TPN/PPN to reach normal pre-albumin 18-35 mg/dL
Adequate amino acids provided when there is an increase in pre-albumin of ~1 mg/dL per day
Parenteral Nutrition
Monitoring
(continued)
Acid/base balance
Adjust TPN/PPN anion concentration to maintain proper acid/base balance
Increase/decrease chloride content as needed
Since bicarbonate is unstable in TPN/PPN preparations, the precursor —acetate—is used; adjust acetate content as needed
Complications of Parenteral
Nutrition
Hepatic steatosis
May occur within 1-2 weeks after starting PN
May be associated with fatty liver infiltration
Usually is benign, transient, and reversible in patients on short-term PN and typically resolves in
10-15 days
Limiting fat content of PN and cycling PN over 12 hours is needed to control steatosis in long-term
PN patients
Complications of Parenteral
Nutrition Support
(continued)
Cholestasis
May occur 2-6 weeks after starting PN
Indicated by progressive increase in TBili and an elevated serum alkaline phosphatase
Occurs because there are no intestinal nutrients to stimulate hepatic bile flow
Trophic enteral feeding to stimulate the gallbladder can be helpful in reducing/preventing cholestasis
Gastrointestinal atrophy
Lack of enteral stimulation is associated with villus hypoplasia, colonic mucosal atrophy, decreased gastric function, impaired GI immunity, bacterial overgrowth, and bacterial translocation
Trophic enteral feeding to minimize/prevent GI atrophy
Parenteral Nutrition Case
Study
55-year-old male admitted with small bowel obstruction
History of complicated cholecystecomy 1 month ago. Since then patient has had poor appetite and 20-pound weight loss
Patient has been NPO for 3 days since admit
Right subclavian central line was placed and plan noted to start TPN since patient is expected to be NPO for at least 1-2 weeks
Parenteral Nutrition Case
Study
(continued)
Height: 6’0” IBW: 178# +/- 10%
Weight: 155# / 70kg 87% IBW
BMI: 21
Usual wt: 175# 11% wt loss x 1 mo.
Estimated needs:
2100-2450 kcal (30-35 kcal/kg)
84-98g protein (1.2-1.4 g/kg)
2100-2450 mL fluid (30-35 mL/kg)
Parenteral Nutrition
Prescription
TPN via right-SC line
2 L total volume x 24 hours
Amino acid 4.5% (or 45 g/liter)
Dextrose 17.5% (or 175 g/liter)
Lipid 20% 285 mL over 24 hours
Above will provide 2120 kcal, 90g protein, glucose infusion rate 3.5 mg/kg/minute, lipid
0.9 g/kg/day
Parenteral Nutrition
Prescription
Important items to consider:
Glucose infusion rate should be < 5 mg/kg/minute
(maximum tolerated by the liver) to prevent hepatic steatosis
Lipid infusion should be < 0.1 g/kg/hour (ideally <
0.4 g/kg/day to minimize/prevent TPN-induced liver dysfunction)
Initiate TPN at ~ ½ of goal rate/concentration and gradually increase to goal over 2-3 days to optimize serum glucose control
Benefits of Enteral Nutrition over parenteral nutrition
Cost
Tube feeding cost ~ $10-20 per day
TPN cost ~ $100 or more per day!
Maintains integrity of the gut
Tube feeding preserves intestinal function; it is more physiologic
TPN may be associated with gut atrophy
Less infection
Tube feeding —very small risk of infection and may prevent bacterial translocation across the gut wall
TPN —high risk/incidence of infection and sepsis
Transitional Feedings
Parenteral to enteral feedings
Introduce a minimal amount of enteral feeding at a low rate (30-40 ml/hr) to establish tolerance.
Decrease PN level slowly to keep nutrient levels at same prescribed amount
As enteral rate is increased by 25-30 ml/hr increments every 8-24 hrs, parenteral can be reduced
Discontinue PN solution if 75% of nutrient needs met by enteral route.
Parenteral/Enteral to oral feedings
Ideally accomplished by monitoring oral intake and concomitantly decreasing rate of nutrition support until
75% of needs are met.
Oral supplements are useful if needs not met 100% by diet. Ex (Nepro, Glucerna, Boost, Ensure).
Refeeding Syndrome
“the metabolic and physiologic consequences of depletion, repletion, compartmental shifts, and interrelationships of phosphorus, potassium, and magnesium…”
Severe drop in serum electrolyte levels resulting from intracellular electrolyte movement when energy is provided after a period of starvation (usually > 7-10 days)
Physiologic and metabolic sequelae may include:
EKG changes, hypotension, arrhythmia, cardiac arrest
Weakness, paralysis
Respiratory depression
Ketoacidosis / metabolic acidosis
Refeeding Syndrome
(continued)
Prevention and Therapy
Correct electrolyte abnormalities before starting nutrition support
Continue to monitor serum electrolytes after nutrition support begins and replete aggressively
Initiate nutrition support at low rate/concentration (~
50% of estimated needs) and advance to goal slowly in patients who are at high risk
Consequences of Overfeeding
Risks associated with over-feeding:
Hyperglycemia
Hepatic dysfunction from fatty infiltration
Respiratory acidosis from increased CO
2
Difficulty weaning from the ventilator production
Risks associated with under-feeding:
Depressed ventilatory drive
Decreased respiratory muscle function
Impaired immune function
Increased infection
Questions
Contact Information:
Carli Schwartz, RD/LDN
Dietitian, Tulane Abdominal Transplant Institute
(504) 988-1176
Carli.Schwartz@hcahealthcare.com
References
American Society for Parenteral and Enteral Nutrition. The Science and
Practice of Nutrition Support . 2001.
Han-Geurts, I.J, Jeekel,J.,Tilanus H.W, Brouwer,K.J., Randomized clinical trial of patient-controlled versus fixed regimen feeding after elective abdominal surgery. British Journal of Surgery.
2001,
Dec;88(12):1578-82
Jeffery K.M., Harkins B., Cresci, G.A., Marindale, R.G., The clear liquid diet is no longer a necessity in the routine postoperative management of surgical patients.
American Journal of Surgery.
1996 Mar; 62(3):167-70
Reissman.P., Teoh, T.A., Cohen S.M., Weiss, E.G., Nogueras, J.J.,
Wexner, S.D. Is early oral feeding safe after elective colorectal surgery?
A prospective randomized trial. Annals of Surgery . 1995 July;222(1):73-7.
Ross, R. Micronutrient recommendations for wound healing. Support
Line.
2004(4): 4.
Krause’s Food, Nutrition & Diet Therapy, 11 th Ed. Mahan, K., Stump, S.
Saunders, 2004.
American Society for Parenteral and Enteral Nutrition. The Science and
Practice of Nutrition Support . 2001.