Concussion Assessment, Recognition & Return to Play
advertisement

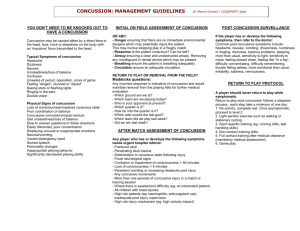
Concussion Assessment, Recognition, & Return to Play Leslie Duinink, MS, LAT Today We Will • • • • • • Review Definition & Symptoms Immediate Evaluation & Management SCAT3 and Child SCAT3 Return to Play New & Ongoing Research Questions Iowa’s Concussion Law – Senate File 367 • Iowa’s Law • Summary – Iowa High School Athletic Association (IHSAA) and the Iowa Girls High School Athletic Union (IGHSAU) must work to distribute guidelines – Provide parent/guardian information regarding concussion and obtain signature prior to participation – Immediate removal from participation if S&S observed by coach or official – If removed, must be cleared by licensed healthcare professional (physician, physician assistant, chiropractor, advanced registered nurse practitioner, nurse, physical therapist, licensed athletic trainer) General Definition “Concussion is a brain injury and is defined as a complex pathophysiological process affecting the brain, induced by biomechanical forces.” Zurich 2012 Definitions 1. Concussion may be caused either by a direct blow to the head, face, neck or elsewhere on the body with an ‘‘impulsive’’ force transmitted to the head. 2. Concussion typically results in the rapid onset of short- lived impairment of neurologic function that resolves spontaneously. However in some cases symptoms and signs may evolve over a number of minutes to hours. 3. Concussion may result in neuropathological changes but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury and as such, no abnormality is seen on standard structural neuroimaging studies. 4. Concussion results in a graded set of clinical symptoms that may or may not involve loss of consciousness. Resolution of the clinical and cognitive symptoms typically follows a sequential course. However it is important to note that in some cases, post-concussive symptoms may be prolonged. 2012 Zurich Consensus Statement Definitions • Sub-concussion or sub-concussive –a blow to the head that does not cause a concussion – Over time these are thought to accumulate, potentially adding up to problems in the future – Unsure of what this may look like moving forward Impact Data from a Helmet with an Accelerometer NatGeo Summary of a Season of Hits Four features of note • • • • Mechanism of Injury Presentation Functional disturbance Graded set of symptoms (w/wo loss of consciousness) resolution is typically sequential course • • • • • One or More Present Suspect a Concussion Symptoms – somatic, cognitive, and/or emotional Physical signs Behavior changes Cognitive impairment (slowed reaction time) Sleep disturbances (may not be immediate) Mechanism of Injury (MOI) • Direct blow to the head, face, neck or elsewhere on the body with “impulsive” force transmitted to the head. Examples can include • Struck with an object – hit with a ball to the head • Strike an object – head hits the floor or wall • Take a body blow from another person • Fall hard on their bottom or from a height • A sudden deceleration event • Others? http://journal.frontiersin.org/Journal/10.3389/fbioe.2013.00015/full Signs You May Observe • • • • • • • • Vacant stare – appears dazed, stunned Delayed verbal and motor response Inability to focus attention Disorientation Slurred or incoherent speech Gross incoordination – moves clumsily Heightened emotions, irritability Memory deficits (pre-event, post injury) Symptoms They May Tell You • • • • • • • • • Headache or “pressure” in the head Nausea or vomiting Balance problems or dizziness Double, fuzzy or blurry vision Sensitivity to light or noise Feeling sluggish, hazy, foggy or groggy Confusion Don’t “feel right” Concentration or memory problems http://www.sportsclinic.ca/ On-field or Sideline Evaluation • If ANY of the previous signs & symptoms are present: – Evaluation by licensed healthcare provider (LHCP); if none available, safely remove, urgent physician referral – Address first aid issues, use a sideline assessment tool (SCAT3 or other), neurological exam (motor & sensory), cranial nerve assessment & balance test – NO same day return to play (RTP) Immediate Management • • • • Unconscious patient Obviously concussed patient Concussion suspected patient Other – when in doubt… Why Monitor? • • • • Bleeding in the brain Serial monitoring for deterioration of symptoms Do not leave alone If not transporting, discuss home care with parent/guardian What to Monitor for Changes • • • • Consciousness Pupil reaction Reflexes Strength • Breathing patterns • Sensations • Movements Decision cannot be made in isolation with one “test” Borrowed from Michael McCrea, PhD, ABPP-CN Based on the Evidence • Imaging contributes little to the evaluation unless suspicion of an intracerebral or structural lesion (skull fracture) exists • 80-90% resolve in 7-10 days • Role of balance testing (BESS test) is valid & reliable • No same day RTP for anyone, at any level Management: Zurich 2012 Recommendations • Cornerstone – physical and cognitive rest • Initial 24-48 hours of rest in acute symptomatic phase • Gradual school and social activities should precede RTP (w/o significant exacerbation of symptoms) • Graduated RTP protocol • Role of low level exercise • Role of meds Return to Learn • Process of return students back to the classroom • Recommendation is that normal classroom activity MUST precede return to play decision • Requires teams working together • Individualized to the student Return to Play (RTP) • • • • • NO same day RTP Each step 24 hours Must be asymptomatic Approximately 1 week to complete What about the 10-20% that don’t recover in 7-10 days? Neuropsychological (NP) assessments • Cognitive function assessment is important PART of the overall assessment and RTP protocol • In absence of NP testing, a more conservative approach for RTP is needed • Perform when asymptomatic, but can also be done in early stages of injury • Baseline not required, but may provide useful information (for all tests) Mental Health Issues • Depression • Anxiety • May require short term medication Pre-participation Physical Exam & Concussion History • • • • Recognize known history Recognize likely UNKNOWN history Include all head, face and cervical spine injuries Knowledge and honesty of all parties, especially the student athlete Modifying Factors • Gender - not unanimous but may be risk factor • LOC >1 minute may modify management • Amnesia - duration of post-concussive symptoms more important than amnesia • Motor & Convulsive phenomena – no special treatment required, use standard protocols • Depression • Dizziness in initial symptom set Why Can’t They Participate with a Concussion? • Second Impact Syndrome Children • • • • • Under 13 Child SCAT3 – 5-12 Home & school management Must be clinically completely symptom free NO RTP same day PREVENTION Protective Equipment & Rules • “There is little evidence supporting the use of specific helmets or mouth guards to prevent concussions outside of specific sports such as cycling, skiing and snowboarding.” Daneshvar, et.al. Clin Sports Med 2011 • Risk compensation due to equipment • Proper technique & coaching – no substitute for this! • Rule changes • Violence in sport • Education NEW & ONGOING RESEARCH What is New? • • • • • • • • • How many is too many? Sub-concussive forces over time (HITS) Concussion Threshold? Future of computerized neurocognitive testing Blood tests Detection of Tau in living brain – PET scan Rest vs light activity during recovery King Devick Test Changing the Culture Sports Culture for Athletes http://www.cdc.gov/headsup/pdfs/resources/concussion_at_play_playbook-a.pdf Heads Up Concussion - CDC Program • Concussion at Play: Opportunities to Reshape the Culture Around Concussion – The way coaches talk about concussion influences young athletes’ decisions to report concussion symptoms – Young athletes feel pressure to hide their concussion symptoms – More likely to play with a concussion during a BIG game – Health care providers and school professionals can help young athletes successfully return to learn and play http://www.cdc.gov/headsup/pdfs/resources/concussion_at_play_playbook-a.pdf References • • • • • • • Courson R. Inter-Association Consensus Statement on Best Practices for Sports Medicine Management for Secondary Schools and Colleges. J Ath Train. 2014;49(1):128-137 http://www.nata.org/sites/default/files/SportsMedicineManagement.pdf (accessed 9/29/15) Daneshvar DH, Baugh CM, Nowinski CJ, McKee AC, Stern RA, Cantu RC. Helmets and Mouth Guards: The Role of Personal Equipment in Preventing Sport-Related Concussions. Clin Sports Med. 2011; 30(1): 145-163. Giza C, et al. Summary of evidence-based guideline update: Evaluation and management of concussion in sports: Report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology,2013;90:2250-2257. http://www.neurology.org/content/80/24/2250.full.pdf+html (accessed 9/29/15) McCrory P, et al. Consensus Statement on concussion in sport: the 4th International Conference on Concussion in Sport held in Zurich, November 2012. BrJSportsMed 2013;47:250–258. Rivara FP, Schiff MA, Chrisman SP, Chung SK, Ellenbogen RG, Herring SA. The Effect of Coach Education on Reporting of Concussions Among High School Athletes After Passage of a Concussion Law. Am J Sports Med 2014; 42(5): 1197-203. doi: 10.1177/0363546514521774 SCAT3, SCAT3 child and Pocket Concussion Recognition Tool available for reproduction on http://www.sportsconcussion.com/concussion-management ttp://www.nata.org/sites/default/files/SportsMedicineManagement.pdf (accessed 9/29/15) http://www.cdc.gov/headsup/pdfs/resources/concussion_at_play_playbook-a.pdf (accessed 9/29/15)