6/21/13 - The Pediatric Emergency Department @ Jackson
advertisement

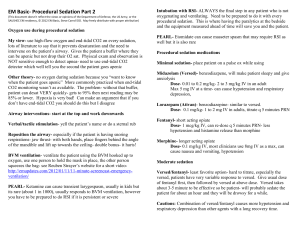
By Tiffany Tamse PGY 1 Indications for Pediatric Procedural Sedation LP Arthrocentesis Suturing Wound care Abscess I&D Fracture reduction Dislocation Foreign body removal Burn debridement Question 1 A 12 yo boy presents to the ED with an uncomplicated forearm fracture. VS: T 37.2, HR 90, BP 116/72, RR 22, Ht 5’6”, Wt 220lbs. On physical exam he is holding his arm close to his chest in flexion and says it is very painful to move. Ortho decides to set the fracture and requests procedural sedation. The ED attending decides to use ketamine. . Which of the following is true for the use of ketamine in this patient? A. He has a lower likelihood of developing nausea given his age and BMI. B. He will need co-administration of an analgesic agent as ketamine does not have analgesic properties. C. BP should be monitored closely as hypotension often occur with ketamine administration. D. Ketamine is a non-progressive dissociative anesthetic and increasing the dose will increase time of sedation but not the depth of sedation. Correct Answer D. Ketamine is a non-progressive dissociative anesthetic and increasing the dose will increase time of sedation but not the depth of sedation. Ketamine is dosed 1-2 mg/kg IV or 4-5 mg/kg IM with a peak onset of 1-2 min IV and 2-5 min IM Infusion rate is over 1-2 minutes to reduce the risk for respiratory depression. An additional 0.5-1 mg/kg may be administered for continued sedation A. He has a lower likelihood of developing nausea given his age and BMI. Percentage of patients with N/V after ketamine range from about 3% to 20% Studies have shown that BMI > 25 (our patient has a BMI of 35) have an increased likelihood of nausea/vomiting after use of ketamine N/V with ketamine administration also peaks around the age of 12 IM administration and higher doses of ketamine have also been shown to have increased rated of N/V Prophylactic Zofran before, during or after the procedure for our patient would be beneficial. B. He will need co-administration of an analgesic agent as ketamine does not have analgesic properties. Ketamine dose have analgesic properties in addition to sedation, anesthesia, and amnesia Ketamine is a PCP derivative and can also cause hallucinations, particularly in older children and adults. Midazolam may be used in conjunction with ketamine to prevent hallucinations. Dose: 0.05 mg/kg (max 2 g) over 3 minutes C. BP should be monitored closely as hypotension often occur with ketamine administration. Ketamine is a sympathomimetic and inhibits catecholamine uptake: Increased HR, BP, CO and coronary perfusion May cause transient increase in ICP Good for use in patients in shock Alternatives should be considered in patients with cardiac disease, increased ICP, or increased IOP Ketamine is also contraindicated in procedures involving laryngeal stimulation as it exaggerates the protective air reflexes and can cause laryngospasm. Question 2 A 14 yo boy with PMH of Autism with aggressive behavior presents to the ED with 6 cm laceration extending from the bottom of the right eye brow to the hairline. Mom says that he was playing in the park and tripped and fell into a tree branch sustaining the laceration. Patient lost consciousness for 30 seconds during the event but is now back to his baseline up walking and trying to get out of the room. VS: T 37.6, HR 92, BP 120/76, RR 20. CT is needed to rule out any head trauma/bleed. And the patient will need sutures to close the laceration. Sedation will be needed and the ED attending decided to use propofol. Which of the following is false about the use of propofol? Which of the following is false about the use of propofol? A. Premedication with Lidocaine is injected into the vein prior to propofol administration as the injection of propofol can be painful B. Sedation with propofol is dose dependent and a larger dose produces deeper sedation which can progress to general anesthesia. C. Hypotension after initial bolus of propofol is expected and transient . D. The patient may be cleared for discharge as early as 30 minutes after drip ends. E. Zofran should be administered before propofol as it causes a high rate of nausea/vomiting. Correct Answer E. Zofran should be administered before propofol as it causes a high rate of nausea/vomiting. Propofol has antiemetic activity and therefore zofran is not needed as often as for ketamine· Other advantages are the fast onset and short halflife. A. Propofol can be very painful upon injection and therefore premedication with lidocaine is very common· dose: 0.5mg/kg injected into the vein with a tourniquet applied for 1 minute Ketamine or opioids may also be used prior to propofol for analgesic effects as propofol does not have any analgesic effects Pain is also less if an antecubital injection site is used compared to a hand vein B. Sedation with propofol is dose dependent and a larger dose produces deeper sedation which can progress to general anesthesia Propofol dosing 0.5-1 mg/kg for the bolus (1-2 mg/kg for 6mo-12 yr of age) with repeated doses of 0.5-1 mg/kg boluses every 3-5 min (max 3mg/kg) Continuous infusion of 25mcg/min titrated up to a max of 200mcg/min to achieve adequate sedation Bolus dosing increased the risk of exceeding desired level of sedation and has been associated with higher risk of respiratory depression, bradycardia, hypotension, or debilitation C. Hypotension after initial bolus of propofol is expected and transient . Should be used with caution in hemodynamically unstable patients (depleted intravascular volume) and consider using an alternate sedation agent Other relative contraindications may be patients with allergy to egg or soybeans, although there is not sufficient evidence to support this statement Other advers effects include respiratory depression and apnea (total adverse effects with propofol use is 2-5%) Prolonged infusions in critically ill patients may cause an acute bradycardia -> asystole + metabolic acidosis, rhabdomyolysis, hyperlipidemia or fatty liver. D. The patient may be cleared for discharge as early as 30 minutes after drip ends. Propofol is an ultra short acting soy-based hypnotic that has lipophillic properties and deposits in the tissues of neuro lipid membranes to potentiate effects of GABA and cause rapid sedation Effective 10-50 seconds after administration T ½ is 9min, making recovery time faster than with most other anesthetics Good for short procedures like CT or other imaging as random movements under sedation do not occur as they do with ketamine Ketofol = Ketamine + Propofol Advantages Propofol decreases the hallucinations and nausea/vomiting from ketamine as well as the emergence phenomenon and helps to produce more stable hemodynamics Ketamine decreases the hypotension from propofol administration as well as the pain, episodes of hypoxia (more stable airway) and requires less boluses to maintain sedation but with similar recovery time Dosing: 1:1 mixed and administered together or ketamine administered first to decrease pain from propofol administration NPO Status Guidelines Clears > 2 hours Solids < 6 months: 4-6 hours 6-36 months: 6 hourso > 36 months: 6-8 hours *Studies have shown that failure of NPO guidelines may not increase risk of complications with procedural sedation . References Up to Date: Selection of medications for pediatric procedural sedation outside of the operating room· Up to Date: Pharmacologic agents for pediatric procedural sedation outside of the operating room· Kinder KL, Lehman-Huskamp KL, Gerard JM. Do children with high body mass indicies have a higher incidence of emesis when undergoing procedural sedation? Pediatr Emerg Care. 2012 Nov;28(11):1203-5. doi: 10.1097/PEC.0b013e318271be65. · Alletag MJ, Aurebach MA, Baum CR. Ketamine, propofol, and ketofol use for pediatric sedation. Pediatr Emerg Care. 2012 Dec;28(12):1391-5; quiz 1396-8. doi: 10.1097/PEC.0b013e318276fde2 · Doctor K, Roback MG, Teach SJ. An update on pediatric hospitalbased sedation. Curr Opin Pediatr. 2013 Jun;25(3):310-6. doi: 10.1097/MOP.0b013e328360bb92