After-care, Rehabilitation and Follow-up
advertisement

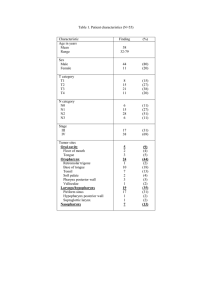
After-care, Rehabilitation and Follow-up Professor Magdy Amin RIAD Professor of Otolaryngology. Ain shames University Senior Lecturer in Otolaryngology University of Dundee cancers of the upper aerodigestive tract • Post treatment major dysfunction with airway, eating and drinking. • Patients with tracheostomy. • Patients with surgical voice restoration prosthesis. • Dental problems, dry mouth, and oral postradiotherapy dysfunction. • Neck and shoulder problems. • Return to work The main aims of follow-up include: 1. Identification of recurrent tumour or new primary disease. 2. Provision of help for patients suffering from side-effects of treatment (particularly delayed effects of radiotherapy). 3. Identification of patients who need additional help with functional or psychosocial problems. Structure of services • The structure of support and rehabilitation services for patients who have been treated for head and neck cancers should be reviewed at Specialised Cancer clinic level. • written rehabilitation plan. • Specialised Support Team should ensure that the long-term needs of patients and carers are met. Local Support Team Members • ENT/maxillofacial surgeon. • Regular examination of the neck is particularly important during the first two years after treatment, when 90% of recurrences develop. Local Support Team Members • Nurse practitioner, who can provide advanced skills for the management of stomas (tracheostomies and gastrostomies), nasogastric tubes and tracheoesophegal valves. Local Support Team Members • Speech and language therapist (SALT): Voice Swallowing • Dietician • Dental hygienist Local Support Team Members • Psycho-oncology, liaison psychiatry or clinical psychology services • Local patients who are willing to provide ‘buddy’ support. • Physiotherapist • Occupational therapist • Social worker Follow-up • patients who continue to smoke or drink alcohol should be encouraged to take up interventions to help them quit. • Follow-up after radiotherapy should include assessment of dental health, the lining of the mouth and salivation, since adverse effects in these areas are common and usually treatable. Oral and dental care • Specialist restorative dentistry and prosthodontic expertise should be available. • A trial of pilocarpine should be offered to patients with persistent xerostomia (dry mouth) after radiotherapy who had normal salivary function before treatment. Swallowing rehabilitation • Swallowing rehabilitation for patients dependent on tube feeding after treatment for head and neck cancer usually takes about three months, according to a Dutch study. • although about 20% need help for six months or more and some patients (9 of a group of 82) did not respond to therapy. • Patients with transport problems fared better than those with aspiration. OTHER CONDITIONS • 11% no definite diagnosis. • Globus and GERD not included. POST OP MYOPATHIES CRANIAL NV POUCHES MECHANISM OF SWALLOWING several closely coordinated actions are involved: (1) elevation and retraction of the soft palate with closure of the nasopharynx, (2) UES opening, (3) laryngeal closure at the level of the laryngeal vestibule, (4) tongue loading (5) tongue pulsion (6) pharyngeal clearance. These events occur in close synchrony, and last only one second. Normal oropharyngeal swallowing The sensory cues that elicit pharyngeal swallowing are not precisely known. sensory receptive field of the superior laryngeal nerve seems to be the crucial stimulus. swallowing can also be initiated solely by volitional effort if there is food or fluid within the oral cavity. Deglutitive pharyngeal reconfiguration: Laryngeal vestibule closure • A fundamental aspect is transforming the oropharynx from a respiratory to a swallowing pathway . • By opening the inlet to the esophagus and sealing the inlet to the larynx. • Laryngeal vestibule closure, is achieved by laryngeal elevation and anterior tilting of the arytenoid cartilages against the base of the epiglottis. • Laryngeal elevation is quantifiable fluoroscopically Deglutitive pharyngeal reconfiguration: UES relaxation • Videofluoroscopic studies done concurrently with manometry have shown that UES relaxation occurs during laryngeal elevation . • Relaxation of the sphincter precedes opening by approximately 0.1 seconds. • UES opening results from anterior traction caused by contraction of the suprahyoid and infrahyoid musculature. Deglutitive pharyngeal reconfiguration : UES opening Clinically, this is a significant point in that : impaired UES opening can result from either impaired traction on the sphincter or impaired sphincter relaxation. • Impaired traction should be evident fluoroscopically by diminished anterior hyoid displacement. • impaired relaxation is only detectable manometrically pharyngeal swallowing: propulsive phase of tongue • The functional elements of pharyngeal swallowing are the propulsive phase of tongue action and of propagated contraction of the pharyngeal constrictors. • Bolus propulsion relies heavily on deglutitive tongue action, transpiring between times 0.00 and 0.13 pharyngeal swallowing: pharyngeal contraction • the propagated pharyngeal contraction progresses from the superior to middle to inferior pharyngeal constrictors at approximately 15 cm/s. • Stripping almost all residue from the pharynx and hypopharynx except for trace amounts that may be left in the valleculae or pyriform sinuses. • Thereby minimizing the chance that aspiration will occur with resumed respiration. Resumption of respiration • After bolus clearance, the process of pharyngeal reconfiguration is reversed. • Allowing resumption of respiration. • The entire pharyngeal swallow occurs in approximately 1 second Oropharyngeal dysphagia Major categories of dysfunction are (1) Inability or excessive delay in initiation of pharyngeal swallowing. (2) Aspiration. (3) Nasopharyngeal regurgitation. (4) Residue within the pharyngeal cavity after swallowing. five fundamental questions • Does the patient describe dysphagia as opposed to globus sensation or Xerostomia? • Is the dysphagia oropharyngeal or esophageal in origin? • Is the dysphagia caused by a structural or functional disorder? • How severe is the dysphagia and are complications present? • Is there an underlying related or causative disease? Xerostomia common in the elderly, present in 16% of men and 25% of women. Dysphagia is attributed to loss of the moistening and lubricating qualities of saliva. Dry mouth may be accompanied by dry eyes, inflammatory arthropathy (Sjogren’s) History of head and neck radiotherapy, or concurrent medications with anticholinergic side effects. Detailed drug history is also important because a number of centrally acting drugs can impair oropharyngeal function Videofluoroscopic evaluation of oral and pharyngeal function (Gold standard) (1) inability or excessive delay in initiation of pharyngeal swallowing, (2) Aspiration (3) Nasopharyngeal regurgitation (4) Residue within the pharyngeal cavity after swallowing. Videofluoroscopy: Limitations videofluoroscopy does not allow: 1.Quantification of pharyngeal contractile forces. 2.Detection of incomplete UES relaxation (which can occur despite normal opening), 3.Quantification of the magnitude of intrabolus pressure during swallowing Nasoendoscopy: FEES • Optimal method for identification of intracavitary structural lesions . • identification and biopsy of mucosal abnormalities. • Liquids and foods colored with food dye are traced during swallowing inability or excessive delay in initiation of pharyngeal swallowing and Speech Rehabilitation • A recent US study indicated that 27% of patients used oesophageal speech, 21% used tracheosophageal speech, and 48% used an electrolarynx. • 89% of patients in the two former groups were satisfied with their means of communication, but satisfaction levels were lower (62%) among those who used the electrolarynx. Repositioning of VF • Secure airway. • Prevent aspiration. • Voice quality. Arytenoidectomyposterior cordotomy • 3 to 4 mm posterior glottic chink. • Mild to moderate exercise. • If in doubt keep the tracheotomy. VF Medialisation VF injection • • • • Timing. Material. Amount. Route. Thyroplasty • Reversible. • Local anaesthesia. • Avoid laryngeal scarring. • Posterior glottic competency. • Manipulation of acoustic properties. Laryngeal position alteration Alaryngeal voice Alaryngeal voice TE surgical set TE puncture TE tract TE Prosthesis Speech Rehabilitation • An older study, also from the US, reported that speech therapy after laryngectomy took an average of five months in patients assessed before surgery, and three months for those reviewed after surgery. • 26% of prospectively studied patients used oesophageal speech as the dominant mode of communication, 34% the electrolarynx and 34% communicated by writing. • 45% were considered not to be successfully rehabilitated. Speech Rehabilitation • Patients with problems that make rehabilitation more difficult such as : hearing impairment, previous neurological, pulmonary and gastroenterological disease • can be identified before treatment. • These patients require intensive help Restorative dentistry • Dental and facial bone restoration using osseointegrated implants are effective for many patients, despite radiation damage to the jawbone. • The proportion of implants reported lost over five years varies between 22% to 79% in patients who have been treated with radiotherapy. Restorative dentistry • One study suggests that hyperbaric oxygen may improve osseointegration in irradiated patients. • The probability of success appears to be higher when reconstruction is carried out more than four months after implantation. • Loss rates are below 20% in patients who have not been irradiated. Treatment for persistent xerostomia • pilocarpine can be effective for patients with xerostomia after radical radiotherapy to the head and neck. • Adverse events are dose-related; increased sweating, for example, occurs in about a quarter of those taking 5mg three times daily, and in twice as many taking twice this dose. • No severe or life-threatening events were reported in any study. Treatment for persistent xerostomia • One review concluded that the optimum dose is 5mg three times a day. • But it is not clear whether systemic or topical pilocarpine is more effective. incidence of recurrent disease and additional primary tumours • 30-50% of patients had local or regional recurrences within five years of initial treatment for head and neck cancer. • the risk of developing a second cancer (most often in the head and neck, oesophagus or lung) among these patients is 10 to 30 times that in the general population. • Continued smoking and drinking after initial treatment are both associated with significant increases in risk. Palliation • as many as half of all patients who develop head and neck cancers eventually die of the disease and will require palliative interventions. • Many experience moderate to severe pain, which should be regularly assessed and treated in accordance with the WHO analgesic ladder. • In most cases, the cause of death is tumour in the head and neck. • Choking or bleeding to death is particularly feared