File
advertisement
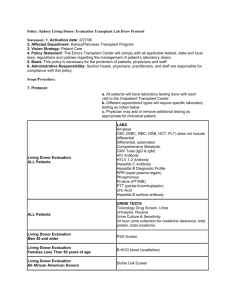
Immunohematology (Blood Bank) CLS 245 What is Immunohematology? • It is the study of Antigen-Antibody reaction as they relate to blood disorder. How can one donation help multiple people? • -In modern medical treatments, patients may receive a pint of whole blood or just specific components of the blood needed to treat their particular condition. • Up to four components can be derived from donated blood. This approach to treatment, referred to as blood component therapy, allows several patients to benefit from one pint of donated whole blood. Cont The main transfusable blood components are: 1. Whole blood. 2. Red cells. 3. Platelets. 4. Fresh frozen plasma 5. Cryoprecipitate AHF (Antihemophilic factors). Blood components Fig2: The whole blood is centrifuged to separate the blood into red cell, plasma and Buffy coat. Fig1: A blood sample after separation shows the main components of a blood. 1-Whole blood: • Whole blood contains red cells, white cells, and platelets (~45% of volume) suspended in plasma (~55% of volume). 2-Red cells, or erythrocytes: • Carry oxygen from the lungs to your body’s tissue and take carbon dioxide back to your lungs to be exhaled. -Note: Buffy coat has leukocytes. Thus, they have to be eliminated to avoid complication of a blood transfusion. 3-Platelets, or thrombocytes: • They are small, colorless cell fragments in the blood whose main function is to interact with clotting proteins to stop or prevent bleeding. • They are prepared by 2 ways: 1- using a centrifuge to separate the platelet-rich plasma from the donated unit of whole blood. 2-Platelets may also be obtained from a donor by a process known as apheresis. What is Apheresis? • Apheresis is a medical technology in which the blood of a donor or patient is passed through an instrument that separates out one particular component and returns the remainder to the human blood circulation. Fig3: Diagram illustrating the process of apheresis. 4-Plasma: • It is a fluid, composed of about 92% water, 7% vital proteins such as albumin, gamma globulin, anti- hemophilic factor, and other clotting factors, and 1% mineral salts, sugars, fats, hormones and vitamins. 5-Cryoprecipitated Antihemophilic Factor: • (Cryo) is a portion of plasma rich in clotting factors,including Factor VIII and fibrinogen. It is prepared by freezing and then slowly thawing the frozen plasma. What is self-antigens? • These are antigens that are found on human cells, and the Immune system doesn’t normally attack these. Fig4: Normal or self-antigens are not attacked by the immune system. ABO system • A system for classifying human blood on the b asis of the presence or absence of two antige ns on the red cell membrane. there are four blood types (A, B, AB, and O). Which Antigen or Antibody is present in each group? Rh system • Rh blood group system, system for classifying blood groups according to the presence (+) or absence (-) of the Rh antigen. • This system has 5 different antigens but antigen D is the most immunogenic. • RH antibodies are NOT naturally occurring. They are formed by immune stimulus due to transfusion or baby red cell during pregnancy. Q) What will happen if the mother is Rh negative and the fetus is Rh positive? To detect a blood group: • 1-Add anti A, anti B and anti D antibody separately to the blood sample • 2-If there is agglutination then the test is positive. This patient blood group is …? -Determine the blood group of each patient Patient1 Patient 2 Pateint3 Patient 4 Patient 5 Patient 6 Patient 7 Patient 8 Patient 9 ABO and Rh blood type donation showing matches between donor and recipient types Nucleic acid Testing (NAT) • Nucleic acid test, often called a "NAT is a molecular technique used to detect a virus or a bacterium in the donor blood. • Examples of pathogen detected by NAT: HIV, HCV and HBV. Antibody screening (Indirect coombs test) • The purpose of the antibody screen is to detect red blood cell antibodies other than anti-A or anti-B. • These antibodies are called “unexpected” because only 0.3 to 2 % of the general population have positive antibody screen. • Antibody screening test involve testing patient’s serum against two or three reagent red blood cell samples called screening cells Cross match • Cross-match test, consisting of mixing the patient’s serum with donor RBCs. • The two main functions of the cross-match test can be cited as: 1- It is a final check of ABO compatibility between donor and patient. 2- It may detect the presence of an Ab in the patient’s serum that will react with Ags on the donor RBCs but that was not detected in the Ab screening because the corresponding Ag was lacking from the screening cell. Summary of blood bank work flow 1. Accurate ABO and Rh typing of the patient. 2. Accurate ABO and Rh typing of the donor. 3. Screening tests for antibodies in the donors and patients serum. 4. In the presence of patient antibodies, selection of appropriate units for each patient. 5. Cross matching. 6. Accurate completion of paperwork and labels