the powerpoint presentation
advertisement

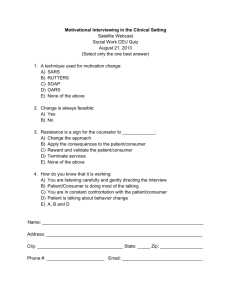
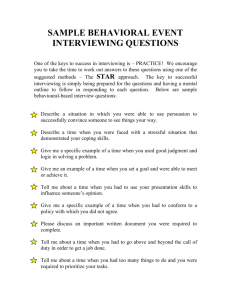
Maximizing the Patient Encounter STRATEGIES TO PROVIDE EXCELLENT PATIENT EDUCATION EMILY FENTON, PA-S, SATF ANTHONY BRENNEMAN MPAS, PA-C Disclosures Emily Fenton University of Iowa, student Student Advisory Task Force of the PAEA Anthony Brenneman, MPAS, PAC University of Iowa, Program Director Multiple positions within the PAEA Objectives For This Session Define the Physician Assistant (PA) role as a patient educator Apply communication strategies and skills that provide effective patient education Explore the integration of specific preventative medicine/health guidelines into patient education sessions Patient Education Why Is It Important?? Patient satisfaction Patient compliance Clinician satisfaction Patient Education Like all clinical skills, it takes time and practice to develop this skill! Be an effective communicator It can be difficult to find the right words You feel like you don’t have the “extra time” Use systematic communication strategies to maximize your interaction with the patient Overview: 2 Strategies For Today “SPIKES” protocol How to break bad news – a method for relaying the message of a negative diagnosis that will significantly alter a patient’s health, happiness, lifestyle, or even lead to their death Motivational Interviewing How to increase patient compliance – strengthen your patient’s commitment to change a behavior adversely affecting their physical or mental health “SPIKES” Protocol: How To Deliver Bad News Introduction SPIKES Setting Patient’s Perception Invitation for Information Knowledge Explore Emotions and Empathize Strategy and Summary “SPIKES” Protocol: How To Deliver Bad News Clinical Scenario Patient is 36 yo nulliparous female who is monogamous with her husband of 4 years. She initially went to her ob/gyn PA to discuss her desire to become pregnant. However, a routine Pap test report came back as abnormal and ultimately led to a diagnosis of cervical cancer. Over the following year, she has yet been unable to become pregnant due to the aggressive recurrence of her cancer. Her PA has scheduled an appointment for today to discuss her most recent workup, which indicates endocervical tissue margins are still positive for microinvasive carcinoma, and the best option is now radical hysterectomy. “SPIKES” Protocol: How To Deliver Bad News Cervical Cancer Screening Guidelines Bethesda system for Pap test screening: ASC-US, ASC-H, LSIL, HSIL Histologic evaluation of cervical biopsy obtained during colposcopy CIN I, II, III Age 21-29 Pap test only Age 30-65 Pap test every 3 years OR Pap test + HPV co-test every 5 years http://wcs-stl.com/wp-content/uploads/2011/09/cervix_exam.327131242_std.gif http://www.arhp.org/publications-and-resources/quick-reference-guide-for-clinicians/managing-hpv/Screening “SPIKES” Protocol: How To Deliver Bad News Clinical Scenario Patient is 36 yo nulliparous female who is monogamous with her husband of 4 years. She initially went to her ob/gyn PA to discuss her desire to become pregnant. However, a routine Pap test report came back as abnormal and ultimately led to a diagnosis of cervical cancer. Over the following year, she has yet been unable to become pregnant due to the aggressive nature of her cancer. Her PA has scheduled an appointment for today to discuss her most recent workup, which indicates endocervical tissue margins are still positive for microinvasive carcinoma, and the best option is now radical hysterectomy. “SPIKES” Protocol: How To Deliver Bad News S.P.I.K.E.S. Setting: Private location with adequate time to deliver news “Is there anyone else you would like to be here?” Patient’s Perception: Patient knowledge: “What do you know about your disease?” Invitation for Information “Would you like to know more about your illness/your treatment options right now?” “SPIKES” Protocol: How To Deliver Bad News K.E.S. S.P.I. Knowledge Warning shot: “Unfortunately, I do have bad news to discuss with you today.” Give information in small chunks and “signpost” when moving to new topics Explore Emotions and Empathize “How are you feeling?” Non-verbal cues Strategy and Summary “Can you tell me what I told you about your disease today?” Schedule follow-up visit “SPIKES” Protocol: How To Deliver Bad News Patient Response To Bad News “We came back and he told me it was cancerous. It was just like my whole body went dead. I went completely numb. The doctor sat and told us things. I never heard another word he said.” “Your mind is racing like, ‘How long am I going to be out of work?’ I am going to have to make lesson plans for 8 weeks. It also raced through my mind, ‘How did I get it? Was it because of stress or just luck?’ You want to know why you have it when there is no answer.” Slide courtesy of Marcy Rosenbaum Overview: 2 Strategies For Today “SPIKES” protocol How to break bad news – a method for relaying the message of a negative diagnosis Motivational Interviewing How to strengthen your patient’s commitment to change a behavior adversely affecting their physical or mental health Motivational Interviewing: Commit To Change A Provider’s “Typical Approach” How do we typically try to convince a patient to change problematic or unhealthy behaviors? Explain what he/she could do differently Warn them about what will happen if they don’t change Counsel them about how to change their behavior Refer them to a specialist Be frustrated by your non-compliant patient! Motivational Interviewing: Commit To Change A Patient’s “Typical Response” How do patients respond to being told what to do? “Paradoxical effect of coercion”: We tend to believe and act on what we hear ourselves say When a provider takes up the “good” side of an ambivalent behavior, the patient is more likely to argue the other side The more we hear ourselves defending our behavior, the more committed we become to it New approach: Actively try to guide the conversation so that it is the client rather than the clinician voicing the argument for change Motivational Interviewing: Commit To Change 4 Steps To Learning MI Understand the spirit of MI 2. Learn how to ask 3. Learn how to respond 4. Learn how to really listen 1. Motivational Interviewing: Commit To Change The Spirit Of MI Collaboration With Patient Compassion Acceptance And Honesty Of Stage Make A Commitment Motivational Interviewing: Commit To Change Your Patient’s Stage Of Change Pre-contemplation Contemplation Preparation Action Maintenance Relapse Motivational Interviewing: Commit To Change Mnemonic To Ask And Respond OARS Open questions Affirmation Reflection Summarize Motivational Interviewing: Commit To Change Learn How To Ask: Open Questions Closed questions invite brief answers, e.g. yes or no: OLDCARTS – “When did you start smoking?” or “How many ppd?” Open questions evoke more elaborate responses: “What, if anything, has been your experience with cigarette smoking?” Motivational Interviewing: Commit To Change Learn How To Respond: Affirmations An affirmation is a genuine statement that emphasizes a strength of the patient. Notice and appreciate a positive action Express positive regard and caring “I see you have tried to quit smoking before, which I think is a great starting point.” Motivational Interviewing: Commit To Change Learn How To Respond: Reflections A reflection is a statement of inference, or hypothesis, about what your patient has told you Attempt to extrapolate the essential meaning of what the patient has told you back to them The patient must respond by confirming, correcting, or elaborating on your comment “You say you don’t see yourself quitting. So you plan to smoke for all the rest of your days.” Motivational Interviewing: Commit To Change Learn How To Respond: Summarize A summary wraps up what the patient has told you Shows you have been listening carefully Allows you to end the conversation and make recommendations for follow-up “This is what I heard you say. Now let’s plan to address that again next time.” Motivational Interviewing: Commit To Change Learn How To Really Listen RULE Resist the righting reflex Understand their motivations Listen to your patient Empower your patient Motivational Interviewing: Commit To Change Video Scenario Motivational Interviewing: Commit To Change Mnemonic To Ask And Respond How did the clinician do? OARS Open questions Affirmation Reflection Summarize Motivational Interviewing: Commit To Change Clinical Scenario Patient is 55 yo with a history of poorly-controlled hypertension (170/90) who has an appointment with you, their family practice PA, for a discussion about lifestyle modification. The patient is obese (BMI = 35), eats a high-salt diet, does not exercise, and refuses to take medications regularly. Use the OARS approach to begin a conversation with your patient about making healthy changes. Motivational Interviewing: Commit To Change 2013 ACC/AHA Blood Cholesterol Guidelines Atherosclerosis is a primary risk factor for cardiovascular disease, including MI or stroke Preventative statin therapy should be initiated in most patients with the following risk factors for atherosclerotic Cardiovascular Disease: Clinical atherosclerotic CV disease LDL ≥ 190 mg/dL Type 1 or 2 diabetes + 10-year ACVD risk ≥ 7.5% 10-year ACVD risk ≥ 7.5% http://jama.jamanetwork.com/article.aspx?articleid=1791497#Results(Recommendations) Motivational Interviewing: Commit To Change Clinical Scenario Patient is 55 yo with a history of poorly-controlled hypertension (170/90) who has an appointment with you, their family practice PA, for a discussion about lifestyle modification. The patient is obese (BMI = 35), eats a high-salt diet, does not exercise, and refuses to take medications regularly. Use the OARS approach to begin a conversation with your patient about making healthy changes. Motivational Interviewing: Commit To Change Discussion OARS Open-ended Affirmations: questions: not yes/no positive attributes Reflections: infer patient’s ultimate view Summarize: show you’re listening Conclusion: Your Role As A Patient Educator Soon you will be a practicing PA Patient education is a part of your job Understand the impact good communication skills can have on the well-being of your patients Use SPIKES and OARS to address difficult but common! clinical scenarios with your patients Be confident in your ability to meet the healthcare needs of your patients Additional Resources And Information Next session: more on your role as an educator in your profession! Future opportunities to learn about PA education: SPIKES information Future Educator Fellowship - November 2015: small number of students + scholarship to attend Education Forum in Washington DC http://www.each.eu/teaching/resources/breaking-bad-news-experientialmodule-curriculum-iowa-120613/ Motivational Interviewing information Miller, W.R.; Rollnick, S. (2002). "Motivational Interviewing: Preparing People to Change'". Guilford press. A special thanks to Marcy Rosenbaum, PhD and Dr. Michael Flaum, MD for their contributions of time and materials in the making of this presentation.