ACA – IRS Reporting – Strategic Moves for School Districts
advertisement

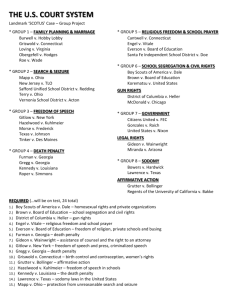
1 I have been practicing since last year’s FERMA Family Feud contest! 2 FERMA “1st and 10” – 2015 Conference Lido Beach John M. Drye, Esq. What We Will Accomplish Today: General Counsel & Chief Risk Strategist – Campus Benefits 1. Goal #1 – Figure out what QUESTIONS to be asking Home Office – Atlanta, GA PPACA , Healthcare Reform & Public School Employee Benefits In 2013 - 2015, completed training sessions to 315 + Public School Systems in GA, AL, TN and FL. Contact: 2. Current issues stemming from the Supreme Court, IRS, DOL and lower courts 3. Cyber issues for school districts 4. All you need to know about (and the solution to) 1094/1095 reporting in 1 minute (maybe) Jdrye@CampusBenefits.com Presentation Disclaimer: www.CampusBenefits.com This presentation is not intended to be exhaustive nor should any discussion or opinions be construed as legal advice. Listeners should contact school legal counsel for legal advice. 3 REVIEW REVIEW REVIEW REVIEW REVIEW REVIEW P.P.A.C.A. Patient Protection and Affordable Care Act 1. Passed by 111th Congress in March 2010. 2. Framework of directives & yet to be finalized set (1) Taxes, (2) Regulations. 3. Designed to be implemented during 2010 – 2018 with the majority of provisions to execute 2014 - 2016. 4. Significant new set of (1) compliance requirements for the employer marketplace and (2) responsibility for the Individual. 4 FERMA RISK – Not knowing all the answers to the topics below Management – Knowing the questions to ask trusted advisors Sample 2015 Checklist 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. FL Health Insurance Exchange (Marketplace) How Marketplace Subsidies work Exchange Plans: Bronze, Silver, Gold, Platinum Individual Mandate Pre-Existing Exclusions Wellness Program – Health Plan Discounts Annual or Lifetime Limits “Employer Shared Responsibility Provisions” Automatic Enrollment Medicaid Expansion Employer Reporting Requirements MEC – Minimum Essential Coverage EHB – Essential Health Benefits SBC – new SBC requirements under PPACA W-2 Reporting Requirements What Fees apply to our district? 1. 2. 3. 4. PCORI (IRC 720) fees and applicability Transitional Reinsurance Fee Health Insurance Provider Fee High Value Plan Tax (Cadillac Tax in 1018) 17. Required Notices (ie: Exchange Coverage options) 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. Review Plan Design Budget for Required Fees/Payments Prepare for Required Admin Tasks Review FSA Design Determine ALE and process Review Employer Mandate Penalties Review Affordability/Minimum Values Determine Measurement periods Begin Tracking Employees Prepare Required Reporting What Needs Documentation Future Requirements 1. What to Do 2. What to Wait on Question What makes a teacher effective? 6 Lets Focus on some of the Challenges facing school districts in 2015 - 2016 FMLA FLSA 7 Challenge #1 - Busy Supreme Court 8 Significant Ruling #1 from SCOTUS on the PPACA National Federation of Independent Business (NFIB) vs. Sebelius SCOTUS Case No. 11-393 (2012) Issue: Is the requirement that most Americans obtain insurance or pay a penalty was authorized by Congress’s power to levy taxes. Decision: The vote was 5 to 4, with Chief Justice John G. Roberts Jr. joining the court’s four more liberal members. Majority: Chief Justice Roberts wrote in the majority opinion. “The Affordable Care Act’s requirement that certain individuals pay a financial penalty for not obtaining health insurance may reasonably be characterized as a tax” “Because the Constitution permits such a tax, it is not our role to forbid it, or to pass upon its wisdom or fairness.” Majority The Governments claim requiring the purchase of insurance was constitutional under the interstate commerce clause failed. 9 Significant Ruling #1 from SCOTUS on the PPACA National Federation of Independent Business (NFIB) vs. Sebelius SCOTUS Case No. 11-393 (2012) What is the impact? (7/15/15 IRS report) • About 6.6 million U.S. taxpayers paid a penalty for 2014 for not having insurance • Roughly 10% more than the Obama administration had estimated • The average penalty was $190 according to the National Taxpayer Advocate, the in-house ombudsman of the IRS. • 300,000 taxpayers overpaid the penalty by a total of $35 million. • The average overpayment was a little more than $110. The IRS hasn’t decided yet whether to issue a refund for the overpayments. • About 10.7 million taxpayers filed for an exemption from the penalty. • 2.6 million filed for premium tax credits to help them afford insurance, adding up to $7.7 billion in subsidies. • The average tax credit was $3,000 10 Significant Ruling #1 from SCOTUS on the PPACA National Federation of Independent Business (NFIB) vs. Sebelius SCOTUS Case No. 11-393 (2012) Why does it matter for school districts? First: Understand the context of “THE MATH” and why employer penalties are so important to pay for PPACA. 1. As the Individual Mandate penalty escalates for taxpayers, and the “claw back” increases from the IRS, more individuals will look to join (not covered now) or remain on your health plan. 2. 1094/1095 - “Notice for Penalty” letters (love notes) could become a more time consuming task than districts are currently planning for. 11 Significant Ruling #2 from SCOTUS on the PPACA King v. Burell SCOTUS Case No. 14-114 (June 25, 2015) Issue: Can individuals be eligible for Health Insurance Subsidies in states (ie: FL) that did not form a “state-based” Health exchange/marketplace. Decision: The vote was 6 - 3 and upheld the acts section 36B tax credits available to individuals who qualify regardless of state or FFE(34), with Chief Justice Roberts again joining the court’s more liberal members. Majority: Chief Justice Roberts wrote in the majority opinion. "Congress passed the Affordable Care Act to improve health insurance markets, not to destroy them," Roberts wrote in his opinion. "The combination of no tax credits and an ineffective coverage requirement could well push a State's individual insurance market into a death spiral," Roberts wrote, aligning with the argument of Solicitor General Donald Verrilli. Majority The key question in the case centered on whether the federal government (not states) had the ability to provide subsidies to help low-income Americans buy health insurance 12 Significant Ruling #2 from SCOTUS on the PPACA King v. Burell SCOTUS Case No. 14-114 (June 25, 2015) Why does it matter for school districts? (1) Solidifies the “Pay or Play” mandate. Because the employee going to an exchange has to receive a subsidy to trigger an employer penalty, a decision the other way would have rendered the mandate ineffective in 34 states (2) Employers adopting a “wait and see” approach – Time is up… in fact at this point you are behind the curve if you have not adopted a strategy for implementation, reporting and penalty review. (3) Reinforces the need for HR personnel to understand the state exchange. (4) Have you put into place a plan for “waiver of coverage” during open enrollment? 13 Significant Ruling #3 from SCOTUS on the PPACA Obergefell v. Hodges SCOTUS Case No. 14-556 (June 26, 2015) Note: 2nd Anniversary of the Windsor decision (DOMA) Issue: Recognizing same-sex marriage in all states Decision: In a 5-4 decision. The Fourteenth Amendment requires a State to license a marriage between two people of the same sex and to recognize a marriage between two people of the same sex when their marriage was lawfully licensed and performed out-of-State. Majority: Justice Kennedy wrote the majority opinion. 14 Significant Ruling #3 from SCOTUS on the PPACA Obergefell v. Hodges SCOTUS Case No. 14-556 (June 26, 2015) Note: 2nd Anniversary of the Windsor decision (DOMA) Why does it matter for school districts? (1) The ruling has effectively created the issue of marriage equality vs. domestic partners. • Many employers in states that did not recognize same-sex marriage, did recognize benefit eligibility for unwed domestic partners. • Not all states have clearly defined registration requirements or rules so employers were left to set standards for what constituted enough of a commitment for a domestic partner to warrant coverage. (2) Review your benefit eligibility rules as it relates to domestic partnerships. Does it need to be updated (Board decision?) (3) What is your policy on “Dependent audits”? (4) When was the last time you updated your Employee handbook? (5) Do you understand how this applies to FMLA issues? 15 Court Case I am watching : Southern District of New York Marin v. Dave & Busters, Inc. S.D.N.Y, No. 1: 15-cv-03608 (Filed May 2015) Issue: Approximately a class of 10,000 workers filed suit alleging that their employer reduced the worker’s hours to keep them from attaining full-time status for the purpose of avoiding mandated coverage offer under the ACA. Theory: ERISA Section 105 Violation which prohibits employers and plan sponsors from interfering with an employee’s attainment of benefits, effectively prohibiting employers from reducing work hours for the purpose of avoiding the requirement to offer health coverage under the ACA. My Opinion: 1. 2. Significant case to watch as it could open the proverbial flood gates. I would argue that a strategy, structured properly, does not interfere with the employees attainment of benefits under ERISA Section 510 16 Court Case I am watching : Southern District of New York Marin v. Dave & Busters, Inc. S.D.N.Y, No. 1: 15-cv-03608 (Filed May 2015) Why does it matter for school districts? 1. As we all know the ACA Employer Mandate generally requires employers to offer coverage to all “FTE” (avg. of 30+ hours) 2. How a school district complies with ACA requirements not only affects potential penalties but law suits as well. 3. Have you set a solid plan into action for classifying certain types of employees. 4. Question: What kind of paper trail are you creating with your compliance requirements? 5. Have you budges for professional advice? accountants, legal, insurance brokers 17 Challenge #2 – Keeping up with the DOL 1. June 12, 2015 Final Regulations updated on SBC and Uniform Glossary 2. June 30th Proposed Amendments to increase threshold of FLSA White Collar Exemption – Expanding the number of employees eligible for overtime. 18 FLSA – Fair Labor Standards Act The Basics • • • • FLSA was enacted in 1938 to establish minimum living standards for workers Found in 29 U.S.C. 201 et seq. & 29 C.F.R. Part 541 Florida Code 448.01 Initial Minimum Wage was 25 cents an hour • Employers determine Exempt and Non-exempt employees • Appropriate record keeping must be maintained by the employer on non-exempt employees •Current salary threshold to be exempt from FLSA is $445 a week / $23,660 a year •General Rule: • Executives, Administrators, Teachers are Exempt Employees • Service Employees such as school secretaries, bus drivers, lunch room workers, and maintenance personnel may be non-exempt 19 FLSA – Fair Labor Standards Act The Proposed Rule Change • June 30 – 295 page report issued to amend FLSA (29 CFR Part 541) • Proposed salary threshold to be exempt from FLSA: • Moving from $445 a week to $970 a week • Moving from $23,660 / year to $50,440 / year • Did not address duties test but did amend salary basis and salary level test. • If adopted will eliminate an estimated 21.4 million exempt employee status. 20 FLSA – Fair Labor Standards Act Why does it matter for school districts? 1. Employee tracking and analysis (ie: 1094/1095 reporting) is becoming more important. How are you devoting resources? 2. Are you data collection practices and software ready to meet new challenges? 3. All employers should start planning for an increase in overtime eligible employees 4. All employers should review the job duties and salary levels of employees currently classified as exempt and determine which employees will likely be deemed nonexempt under the new (proposed) regulations. 21 FLSA – Fair Labor Standards Act 22 Challenge #3 - Healthcare “Data” Protection Cyber Attacks on Districts Data Security BBA Agreements Notification Requirements Communication Strategies IT Due Diligence 23 What happened? Why it affects all SHBP members… January 29, 2015 • Anthem victim of a cyber attack (BREACH) • 80 Million current and former customers (dating back to 2004) data stolen • Names, birthdays, medical IDs/social security numbers, street addresses, email addresses and employment information, including income data. • No evidence that credit card or medical information, such as claims, test results or diagnostic codes were targeted or compromised. • Impacted individuals offered (by Anthem) credit monitoring/identity protection California, Colorado, Connecticut, Georgia, Indiana, Kentucky, Maine, Missouri, Nevada, New Hampshire, New York, Virginia, and Wisconsin. 24 Why did it happened? • Hospitals, clinics, Insurance carriers and affiliated entities traditionally do not meet the high standards required to protect data including “PHI” Personal Health Information. • The main reason these institutions fail is due to consolidation and mergers where smaller entities computer systems don’t always connect or data management becomes challenging. • Dell Security works reports that a “complete set of health insurance credentials” sold for $20 on underground markets in 2013. • That is 10-20 times the price for a US credit card number with a security code • This is not the first time Anthem (formerly WellPoint) has been breached. In 2013, Anthem agreed to pay $1.7 million to resolve allegations it left information for 612,000+ members available online because the insurer failed to execute adequate safeguards People’s Liberation Army’s Unit 61398 1. 2. 3. Illegal & Bogus Treatment Buy Addictive drugs Obtain free treatment 25 July 9th announcement of OPM Hack Overview • 21.1 Million applicants had their personal data stolen • Two Breaches between 2013 – 2014 • April 4.2 Million people • July 21.5 million people • Total 22.1 (3.6 million overlap) •Among the data stolen (fingerprints , Social Security numbers, Health records) • Same week announced: United Airlines, Wallstreet Journal and NYSE all had their systems attacked and taken off-line. • Has the Cold war has turned into the Cyber war? • Credit Card Breach – Phone Call / Zero liability • Medical ID Breach – If used for treatments what happens if you show up to the hospital and your blood type or allergies list is different? 26 The Law -- Exposure School Districts Have… Federal Law – There are several areas pertinent to discussion (especially notification requirements) but an important law to understand as an employer or business partner is related to the U.S. Health and Human Services office for Civil Rights. As required by section 13402(e)(4) of the HITECH Act, the Secretary must post a list of breaches of unsecured protected health information affecting 500 or more individuals. Since 1997 HHS has logged over 1,200 breaches. This list includes hospitals, doctors, dentist, insurance brokers, universities, state and county governmental entities and many others. 27 The Law (Florida) -- Exposure School Districts Have… State of Florida Law - The Florida Information Protection Act of 2014 repeals section 817.5681 and replaces it with a new statute: section 501.171 Notification required upon breach of security regarding personal information: The new statute requires notice to be provided to affected individuals within 30 days. In addition, notice must now be provided to the Florida Department of Legal Affairs for any breach affecting 500 or more individuals within 30 days of the breach unless good cause is provided to the department in writing for an additional 15-day delay. The new statute authorizes the Florida Office of Attorney General to bring enforcement actions under FDUTPA for any statutory violations, but does not create private rights of action for affected individuals. The new statute expands the definition of “personal information” to include health insurance policy or subscriber numbers, information regarding an individual’s medical history, financial information, and online user names or email addresses in combination with their associated passwords or security questions and answers to permit account access. The civil penalties for FDUTPA violations could be up to $1,000 per day for the first2830 days and $50,000 for each subsequent 30-day period, not to exceed a total of $500,000. Lessons Learned & Tips for Superintendents Why does it matter for school districts? 1. Have you documented any training on cyber security in HR? 2. One “Hacktivist” can cause substantial damage and financial penalty. Do you have the right BBA agreements in place with your vendors. 3. Do you have a HIPAA compliance training course in place for your employees? Best Practices: Review your exposure and test the security of your Business Associates: 1. BBA Agreement Review 2. Mandatory “Site Visit” for Insurance and Retirement Brokers/Providers 29 The 1-minute solution to 1095 Filings Legal Notice: Do not try this at home or work. It is a very bad idea. 30 Informational Reporting 1094/1095 STOP attending seminars on the nitty gritty details of 1094/1095 until: – You read the instructions for the forms – Your print off and review the forms – You understand the top 12 Questions surrounding 1094 / 1095-C reporting I will release a client alert in the beginning of August if you are interested jdrye@CampusBenefits.com 31 jdrye@CampusBenefits.com 32 Bonus Material – What will cause the most “Reporting Stress” for your HR Departments? NEW PPACA Reporting Requirements – IRS Code Sections §6055 & §6056 That require IRS Reporting Forms 1094 / 1095 -----------------Health Waiver Documentation SBC Disclosures Marketplace Disclosures Timeline Penalties Administration 33 New Burdensome Reporting Requirements The Affordable Care Act (“ACA”) created new reporting requirements under Internal Revenue Code (“IRC”) §6055 and §6056. 1. Under these new reporting rules, certain employers must provide information to the IRS about the medical plan coverage they offer (or do not offer) to their employees. 2. Code §6055 requires insurers, self-insured health plan sponsors, government agencies that administer government-sponsored health insurance programs and any other entity that provides minimum essential coverage (“MEC”) to report information on that coverage to the IRS and covered individuals. 3. Code §6056 requires applicable large employers (“ALEs”) subject to the employer shared responsibility rules to report information on the health coverage offered to full-time employees to the IRS and covered individuals. 34 Why??? In order to enforce New Reporting Requirements and pay for PPACA: The Government needs data to administer significant parts of the PPACA mandates, such as: (1) Employer Shared Responsibility Penalty (ALE (Applicable Large Employer – 50+) ) (2) Individual Mandate (3) Each State “Exchange / Marketplace” Subsidy eligibility July 24, 2014 (draft forms) – February 4, 2015 final forms 35 What??? New Reporting Requirements Form 1095–C : Employer-Provided Health Insurance Offer & Coverage • • • • Offer of coverage “code” Employee Share of Lowest “MEC” offered plan (Affordable?) Must report every month List of covered individuals Similar in nature to a w-2 form, this informational notice is required for individuals to show proof of coverage to avoid “individual mandate penalties” and/or qualify for exchange subsidies 36 What??? New Reporting Requirements What information will school districts need to collect and merge into one file? 1. What employees were full-time during 2015 and when • Define and track full-time status 2. What months was coverage offered to each employee 3. Was the coverage offered minimum value The Not So “simple” Six 4. What affordable safe harbor was met and when 5. Which transitional rule was applied and when 6. Was coverage offered to spouse and dependents and when 37 When??? New Reporting Requirements Form 1095–C : Employer-Provided Health Insurance Offer & Coverage Deadlines in 2016 1. Statements must be furnished by mail, unless the recipient affirmatively consents (proof) to receive the statements electronically 2. First statements are due to individuals by February 1, 2016 3. Statements must be filed with the IRS (along with Form 1094): • February 28th (if by paper) • March 31st (if electronically) • (Employers with more than 250 must file electronically) 38 When??? New Reporting Requirements Form 1095–C : Employer-Provided Health Insurance Offer & Coverage Challenge #1: IRS is not ready to accept electronic feeds and may not be ready by the deadline: (Publication 5165 ACA Information Returns Guide for more details and file format) Challenge #2: SHBP and (ADP) have not fully determined the process of getting needed data to the school systems and it will likely not occur until January giving little time for districts without advance planning to file. Challenge #3: School District Data, Data, Data • • • • Aggregating data needed to complete the forms (Merge from SHBP) Classifying employees by the coding system Sending forms to both employees who elected and who did not “Look back” and tracking for eligibility 39 What??? Form 1094-C : New Reporting Requirements Transmittal Form summarizing all 1095-C forms issued Similar in nature to the w-3 Form that summarizes all w-2s issued to employees. Significant work is required to classify employee “codes” and Certifications of eligibility safe harbors 40 Penalties??? New Reporting Requirements Two different sections of the Internal Revenue Code discuss the penalties for not complying with Code §6055 and §6056 reporting: 1. Code §6721 discusses failing to send correct returns to the IRS. •The basic penalty is $100 for each incorrect return. •The total fine during any calendar year will not exceed $1,500,000. 2. Code §6722 discusses failing to provide employee statements. •The penalty is the same as above but applies for not providing individual statements. However, initially penalties may be waived if the failure is due to reasonable cause and not to willful neglect. §4980 (H) a & b – Codes section describing the “tracking” penalty traps 41 Penalties??? New Reporting Requirements Final regulations include short term relief from penalties to allow time to develop appropriate procedures for data collection and compliance with these new reporting requirements. For returns and statements filed and furnished in 2016 (reporting for 2015 calendar year), the IRS will not impose penalties on reporting entities that can show they make good faith efforts to comply with the information reporting requirements. • This relief is provided only for incorrect or incomplete information reported on the return or statement, including social security #’s, TINs or dates of birth. • No relief is provided for reporting entities that do not make a good faith effort to: • Comply with these regulations or • Fail to timely file an information return or statement. 42 Challenge #3 – “Under the Gold Dome” 43