Chapter 5 Gases
advertisement

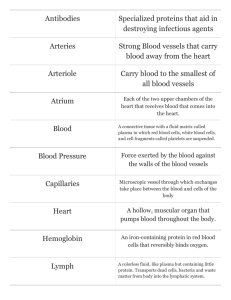
Chapter 36 Circulation Sections 8-13 Albia Dugger • Miami Dade College 36.8 Blood Vessel Structure and Function • Contracting ventricles put pressure on the blood, forcing it through a series of vessels that vary in their structure. • Arteries have thick walls containing smooth muscle reinforced with elastic connective tissue • When a ventricle contracts, artery walls to bulge and spring back, creating a pulse Blood Vessel Structure and Function • Blood flows from arteries into arterioles • In the systemic circuit, the distribution of blood to particular body parts is adjusted by altering the diameter of arterioles • Smooth muscle that rings each arteriole responds to signals from the autonomic nervous system, and to chemical signals • Sympathetic stimulation causes vasodilation of arterioles in the extremities and vasoconstriction of arterioles of the gut Blood Vessel Structure and Function • A capillary is a cylinder of endothelial cells, one cell thick, wrapped in basement membrane – its narrow diameter facilitate exchanges between blood and interstitial fluid • Blood flows from capillaries into venules, which empty Into veins • Veins are large-diameter, low-resistance vessels that convey blood to the heart – many veins have flaplike valves that help prevent backflow from the heart to the heart valve endothelium smooth muscle connective tissue capillary network B Arteriole D Venule endothelium A Artery C Capillary E Vein Figure 36-14 p638 Take-Home Message: How do blood vessels differ in structure and function? • Arteries are thick-walled, large-diameter vessels. Stretching and recoil of arteries helps keep blood moving. • Smooth muscle in the wall of arterioles allows adjustments to blood flow in the systemic circuit. • Capillaries are narrow tubes of epithelial cells. They are the site of exchanges with interstitial fluid. • Veins have valves that prevent backflow. 36.9 Blood Pressure • Blood pressure is the pressure exerted by blood on the walls of blood vessels • Blood pressure is highest in arteries, then declines throughout a cardiovascular circuit Change in Blood Pressure through the Systemic Circuit. Systolic and Diastolic Pressure • Systolic pressure, the highest pressure of a cardiac cycle, occurs as contracting ventricles force blood into arteries • Diastolic pressure, the lowest blood pressure of a cardiac cycle, occurs when ventricles are relaxed • Blood pressure is measured in millimeters of mercury (mm Hg), and is written as systolic /diastolic • Normal blood pressure is about 120/80 mm Hg Measuring Blood Pressure Controlling Blood Pressure • Blood pressure depends on total blood volume, how much blood the ventricles pump (cardiac output), and whether arterioles are constricted or dilated • Receptors in the aorta and carotid arteries monitor blood pressure and send signals to the medulla, which regulates cardiac output and arteriole diameter • Inability to regulate blood pressure can result in hypertension, in which resting blood pressure remains above 140/90 Take-Home Message: How is blood pressure recorded and regulated? • Blood pressure is the fluid pressure exerted against a vessel wall. It is recorded as systolic/diastolic pressure. • Adjustments to arteriole diameter, cardiac output, and blood volume regulate blood pressure. 36.10 Mechanisms of Capillary Exchange • Capillary beds are diffusion zones, where blood exchanges substances with interstitial fluid • As blood flows through a circuit, it moves fastest through arteries, and slowest in capillaries • Slow flow through capillaries enhances the rate of exchanges between the blood and interstitial fluid Substance Exchange • To move between the blood and interstitial fluid, a substance must cross a capillary wall • Oxygen, CO2 , and small lipid-soluble molecules diffuse across endothelial cells of a capillary • Some larger molecules enter endothelial cells by endocytosis, diffuse through, then enter interstitial fluid by exocytosis Fluid Exchange • Higher blood pressure at the arterial end of a capillary bed forces fluid out between cells • At the venous end of the capillary, interstitial fluid enters the capillaries by osmotic pressure • Normally, there is a small net outward flow of fluid • The lymphatic system returns fluid to the blood Fluid Movement at a Capillary Bed blood to venule high pressure causes outward flow blood from arteriole inward-directed osmotic movement cells of tissue Take-Home Message: How do blood and interstitial fluid exchange materials? • Small molecules cross cells of a capillary by diffusion and larger ones move across by exocytosis. • Fluid rich in oxygen and nutrients also leaks out between cells of the capillary wall. 36.11 Venous Function • Veins are the body’s largest blood reservoir • Skeletal muscle activity helps move blood at low pressure through veins and back to the heart • Valves in veins help prevent backflow • Contractions of smooth muscle inside vein walls helps force blood toward the heart venous valve Figure 36-18 p641 blood flow to heart valve open valve closed valve closed valve closed Figure 36-19a p641 Take-Home Message: What are the functions of veins? • Veins are the body’s main blood reservoir. The amount of blood in the veins changes depending on activity level. • Blood pressure in veins is low. One-way valves, activity of skeletal muscle, and respiratory muscle action all help move the blood toward the heart. 36.12 Blood and Cardiovascular Disorders • Red blood cell disorders • Anemias are caused by low red blood cell counts • Thalassemias disrupt hemoglobin synthesis • Polycythemia is an excess of red blood cells • White blood cell disorders • Infectious mononucleosis increases monocyte production • Leukemias are cancers originating from stem cells in bone • Lymphomas are cancers that originate from B or T lymphocytes Blood and Cardiovascular Disorders • Atherosclerosis is a buildup of lipids such as cholesterol in the arterial wall that narrows the lumen • Cholesterol may be bound into low-density lipoproteins (LDLs) which are deposited in blood vessels; or into highdensity lipoproteins (HDLs) and taken up by the liver An Atherosclerotic Plaque Stroke and Heart Attack • Atherosclerosis increases the risk of stroke and heart attack • Clogged coronary arteries can be treated with a bypass or angioplasty • Angioplasty is also used to open partially blocked carotid arteries in the neck that supply blood to the brain Coronary Bypass Surgery A Coronary bypass surgery. Veins from another part of the body are used to divert blood past the blockages. This illustration shows a “double bypass,” in which veins are placed to divert blood around two blocked coronary arteries. vein from leg; used to bypass blockage blocked coronary artery Balloon Angioplasty and Stent plaque flattened by balloon angioplasty stent (metal mesh) placed to keep artery open B Balloon angioplasty and the placement of a stent. After a balloonlike device is inflated in an artery to open it and flatten the plaque, a tube of metal (the stent) is inserted and left in place to keep the artery open. Hypertension • Hypertension is chronically high blood pressure above 140/90 • Hypertension makes the heart work harder than normal, which can cause it to enlarge and to function less efficiently • High blood pressure also increases risk of atherosclerosis Rhythms and Arrhythmias • Electrocardiograms (ECGs) record the electrical activity of a beating heart • They can also reveal arrhythmias, which are abnormal heart rhythms caused by malfunction of the SA node • Bradycardia is a below-average resting cardiac rate • Tachycardia is a faster than normal heart rate • Palpitations are occasional episodes of tachycardia • Atrial fibrillation disrupts atrial contractions • Ventricular fibrillation causes death Electrocardiograms Take-Home Message: What factors impair circulatory function? • Altered blood cell number or quality can alter blood’s ability to carry out its functions. • Atherosclerosis and hypertension raise the risk of heart attack and stroke. • Problems with the cardiac pacemaker cause arrhythmias. Video: Repairing Damaged Hearts with Patients’ Own Stem Cells 36.13 Interactions With the Lymphatic System • Vessels and organs of the lymphatic system interact closely with the circulatory system • The lymph vascular system consists of lymph capillaries and vessels that collect water and solutes from interstitial fluid and deliver them to the circulatory system • Fluid that moves through these vessels is called lymph Three Functions of the Lymph Vascular System • Returns fluids and plasma proteins that leak out of capillaries to the circulatory system • Delivers fats absorbed from the small intestine to the blood • Transports cellular debris, pathogens, and foreign cells to lymph nodes Lymphoid Organs and Tissues • Lymph nodes filter lymph before it enters blood and identify pathogens • Tonsils in throat and adenoids in nasal cavity respond to inhaled pathogens • The spleen filters pathogens, worn out blood cells, and platelets from blood • The thymus gland matures T lymphocytes essential to the immune system Tonsils Defense against bacteria and other foreign agents Right lymphatic duct Drains right upper portion of the body Thymus gland Site where certain white blood cells acquire means to chemically recognize specific foreign invaders Thoracic duct Drains most of the body Spleen Major site of antibody production; disposal site for old red blood cells and foreign debris; site of red blood cell formation in the embryo Some of the lymph nodes Filter bacteria and many other agents of disease from lymph Some of the lymph vessels Return excess interstitial fluid and reclaimable solutes to the blood Bone marrow Marrow in some bones is production site for infectionfighting blood cells (as well as red blood cells and platelets) Figure 36-23a p644 lymph capillary interstitial fluid flaplike “valve” made of overlapping cells at tip of lymph capillary B capillary bed Figure 36-23b p644 lymph trickles past organized arrays of lymphocytes valve (prevents backflow) C Lymph node Figure 36-23c p644 Take-Home Message: What are the functions of the lymphatic system? • The lymph vascular system consists of tubes that collect and deliver excess water and solutes from interstitial fluid to blood. It also carries absorbed fats to the blood, and delivers disease agents to lymph nodes. • The system’s lymphoid organs, including lymph nodes, have specific roles in body defenses.