Psychological disorders
advertisement

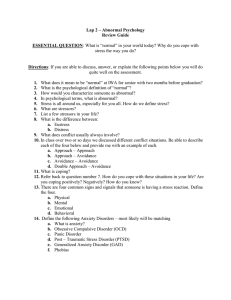
Psychological disorders • Abnormal vs. normal – The 4 D’s – The 3 C’s plus norms, zeitgeist • Explanations – various psychological and personality theories • Classifying psychological disorders – History – Diagnostic and statistical Manual • Major psychological disorders – – – – – Anxiety Somatoform & dissociative Mood Psychotic Personality disorders Abnormal vs. normal • Dialectic thinking – Opposite concepts define each other (thesis – antithesis) • The 4 D’s – Deviance (statistical, not judgmental) – Distress – Danger – Dysfunction Abnormal vs. normal • The 3 C’s – Contents (what a person does, maladaptive, irrational, unpredictable) – Context (When and where a BX occurs ) – Consequences (Distress or suffering) – Norms (Age gender culture historical period) Theoretical explanations for psychological disorders • • • • • • • Biological Psychodynamic Behavioral Cognitive Humanistic – existential Social cultural Bio-psycho-social Theories, continued • Diathesis- stress model – Also known as the vulnerability – stress model – Assumes a predisposition that will only present with sufficient and disorder specific stress – Classic example in biology is heart disease – Psychology examples include cognitive models of depression • For example relationship oriented vs. achievement oriented Cultural issues • Constructivist vs Objectivist definitions – Definitions of normality to a large degree are based on cultural traditions. Epidemiology • Study of prevalence and cause of disease – Etiology : study of cause – Prevalence • Point • Lifetime Point Lifetime Source Schizophrenia 0.3–0.7% Wikipedia 2012 Bipolar 1.0% Wikipedia 2012 17% Wikipedia 2012 • Depression 3-6% ♂ 8-10% ♀ DSM History • DSM stands for The Diagnostic & Statistical Manual of mental disorders • DSM I 1952 • DSM II • Homosexuality removed as a disorder, 1973 • DSM III 1980 – Descriptive vs theoretical (atheoretical) • DSM III-R 1989 • DSM-IV 1994 • DSM- V 2013 – Major overhaul Classification DSM IV • 5 Axes – Axis I Major Mental disorders – Axis II notes personality disorders and mental retardation – Axis III reflect any relevant physical conditions – Axis IV records any psychosocial or environmental problems – Axis V has a rating of one's current level of psychological social functioning DSM • Benefits – Increased interrelater reliability • Criticisms – – – – Reliability improved for some, not all Validity improved for some, not many Qualitative differences between health/non-health Discrete categories • vs dimension (or 3rd variable, eg, “negative emotionality”) – Same sx in different categories – Subjectivity inherent DSM-V • are they more like theoretical constructs or more like diseases; • how to reach an agreed definition; • whether the DSM-V should take a cautious/conservative approach; • the role of practical rather than scientific considerations; • the issue of use by clinicians or researchers; • and whether an entirely different diagnostic system is required Anxiety Disorders • Biological factors – Some people appear to have inherited predispositions – norepinephrine, serotonin may be factors • Psychological factors – People with anxiety disorders may exaggerate dangers of some stimuli while underestimating their own ability to deal with them Anxiety Disorders • Key commonality is physiological: heart rate, breathing, sweating, dry mouth, sense of dread • Fear/anxiety – phobia – generalized anxiety disorder – Panic disorder – obsessive compulsive disorder – PTSD Phobia • Often phobias are experienced as irrational • Simple or specific – Classic, typically afraid of a specific object or situation: • Spiders, Heights, Etc. • Social – Major fear his of humiliation and/embarrassment • Avoids opportunities that could put them into a position of ridicule: – Eating in public, public restrooms, public speaking • Agora – Fear of being separated from a safe place or person Generalized Anxiety Disorder • A nonspecific experience of anxiety, worry – This excessive worry often interferes with daily functioning, as individuals suffering GAD typically anticipate disaster, and are overly concerned about everyday matters such as health issues, money, death, family problems, friend problems, relationship problems or work difficulties. – Often comorbid with dysthymia Panic Disorder • Attack vs Disorder • Terror and fear of death, going crazy • Often experienced as coming from out of the blue • Hyper sensitivity to physiological changes • Cognitive tendency to catastrophize those changes OCD • Obsessive compulsive disorder is characterized by obsessions and compulsions • Obsessions are thoughts the create anxiety – The thoughts made be about germs dirt or graphically violent thoughts • Compulsions temporarily reduce that anxiety PTSD • Trauma defined • Acute vs. post • Acute occurs within 30 days of trauma, post occurs after • Symptoms include avoidance of anything that could remind a person of trauma • Flashbacks and nightmares Somatoform Disorders • Physical ailments without physical cause • Earliest forms were targeted by Freud – (Anna O) • • • • Conversion Hypochondriasis Somatization (Briquettes) Pain Disorder Somatoform • Over the course of the 20th century numerous studies convinced medical and clinical researchers that psychological factors, such as stress, worry, and perhaps even unconscious needs, can contribute to bodily illness Somatoform Sometimes when physicians cannot find a medical cause for a patient’s symptoms, he or she may suspect other factors are involved. Patients may malinger, intentionally fake illness to achieve external gain (e.g., financial compensation, military deferment) Patients may be manifesting a factitious disorder intentionally producing or faking symptoms simply out of a wish to be a patient Somatoform • Known popularly as Munchausen syndrome, people with a factitious disorder often go to extremes to create the appearance of illness – Many secretly give themselves medications to produce symptoms – Patients often research their supposed ailments and are impressively knowledgeable about medicine Somatoform Conversion disorder often is hard to distinguish from genuine medical problems It is always possible that a diagnosis of conversion disorder is a mistake and the patient’s problem has an undetected medical cause Physicians sometimes rely on oddities in the patient’s medical picture to help distinguish the two For example, conversion symptoms may be at odds with the known functioning of the nervous system, as in cases of glove anesthesia Somatoform People with a somatization pattern experience many long-lasting physical ailments that have little or no organic basis Also known as Briquet’s syndrome A sufferer’s ailments often include pain symptoms, gastrointestinal symptoms, sexual symptoms, and neurological symptoms Patients usually go from doctor to doctor in search of relief Somatoform Predominant pain pattern If the primary feature of somatic symptom disorder is pain, the individual is said to have a predominant pain pattern Although the precise prevalence has not been determined, this pattern appears to be fairly common The pattern often develops after an accident or illness that has caused genuine pain The pattern may begin at any age, and more women than men seem to experience it Somatoform Tx • Difficult to treat • Controversial: maybe not psychological but we don’t have the tech to dx • Hypochondriasis tx includes recommendation to Doctors to being open and setting the stage for the next doctor to do the same. Be honest, sincere, and supportive, but don’t feed the client’s anxieties or demands. Dissociative • Based on the Defense Mechanism – Think of your safe place rather than be present – Similar to hypnosis – Common in childhood (make believe friend) • Amnesia (not biological) • Fugue • Dissociative Identity Disorder – (DID, FKA Multiple Personality Disorder) Dissociative • The key to our identity – the sense of who we are and where we fit in our environment – is memory • In dissociative disorders, one part of the person’s memory typically seems to be dissociated, or separated, from the rest Dissociative • There are several kinds of dissociative disorders, including: – Dissociative amnesia – Dissociative identity disorder (multiple personality disorder) – Depersonalization-derealization disorder • These disorders are often memorably portrayed in books, movies, and television programs Dissociative • People with dissociative amnesia are unable to recall important information, usually of a stressful nature, about their lives – The loss of memory is much more extensive than normal forgetting and is not caused by physical factors – Often an episode of amnesia is directly triggered by a specific upsetting event Dissociative • Dissociative amnesia may be: – Localized – most common type; loss of all memory of events occurring within a limited period – Selective – loss of memory for some, but not all, events occurring within a period – Generalized – loss of memory beginning with an event, but extending back in time; may lose sense of identity; may fail to recognize family and friends – Continuous – forgetting continues into the future; quite rare in cases of dissociative amnesia Dissociative • All forms of the disorder are similar in that the amnesia interferes mostly with a person’s memory for personal material – Memory for abstract or encyclopedic information – usually remains intact • Clinicians do not known how common dissociative amnesia is, but many cases seem to begin serious threats to health and safety Dissociative • An extreme version of dissociative amnesia is called dissociative fugue – Here persons not only forget their personal identities and details of their past, but also flee to an entirely different location • For some, the fugue is brief – a matter of hours or days – and ends suddenly • For others, the fugue is more severe: people may travel far from home, take a new name and establish new relationships, and even a new line of work; some display new personality characteristics DISSOCIATIVE IDENTITY DISORDER • A person with dissociative identity disorder (DID, or multiple personality disorder) develops two or more distinct personalities, called “subpersonalities”, each with a unique set of memories, behaviors, thoughts, and emotions DISSOCIATIVE IDENTITY DISORDER • At any given time, one of the subpersonalities dominates the person’s functioning – Usually one of these subpersonalities – called the primary, or host, personality – appears more often than the others – The transition from one subpersonality to the next (“switching”) is usually sudden and may be dramatic DISSOCIATIVE IDENTITY DISORDER • Most cases are first diagnosed in late adolescence or early adulthood – Symptoms generally begin in childhood after episodes of abuse • Women receive the diagnosis three times as often as men DISSOCIATIVE IDENTITY DISORDER • How do subpersonalities interact? – The relationship between or among subpersonalities varies from case to case • Generally there are three kinds of relationships: – Mutually amnesic relationships – subpersonalities have no awareness of one another – Mutually cognizant patterns – each subpersonality is well aware of the rest – One-way amnesic relationships – most common pattern; some personalities are aware of others, but the awareness is not mutual » Those who are aware (“co-conscious subpersonalities”) are “quiet observers” DISSOCIATIVE IDENTITY DISORDER • How do subpersonalities interact? – Investigators used to believe that most cases of the disorder involved two or three subpersonalities • Studies now suggest that the average number is much higher – 15 for women, 8 for men – There have been cases of more than 100! DISSOCIATIVE IDENTITY DISORDER • How do subpersonalities differ? – Subpersonalities often display dramatically different characteristics, including: • Identifying features – Subpersonalities may differ in features as basic as age, sex, race, and family history • Abilities and preferences – Although encyclopedic information is not usually affected by dissociative amnesia, in DID it is often disturbed – It is not uncommon for different subpersonalities to have different abilities, including being able to drive, speak a foreign language, or play an instrument DISSOCIATIVE IDENTITY DISORDER • How do subpersonalities differ? – Subpersonalities often display dramatically different characteristics, including: • Physiological responses – Researchers have discovered that subpersonalities may have physiological differences, such as differences in autonomic nervous system activity, blood pressure levels, and allergies DISSOCIATIVE IDENTITY DISORDER • How common is DID? – Traditionally, DID was believed to be rare • Some researchers even argue that many or all cases are iatrogenic; that is, unintentionally produced by practitioners – These arguments are supported by the fact that many cases of DID first come to attention only after a person is already in treatment » Not true of all cases DISSOCIATIVE IDENTITY DISORDER • The psychodynamic view – Psychodynamic theorists believe that dissociative disorders are caused by repression, the most basic ego defense mechanism • People fight off anxiety by unconsciously preventing painful memories, thoughts, or impulses from reaching awareness DISSOCIATIVE IDENTITY DISORDER • The psychodynamic view – In this view, dissociative amnesia is a single episode of massive repression – DID is thought to result from a lifetime of excessive repression, motivated by very traumatic childhood events DISSOCIATIVE IDENTITY DISORDER • The behavioral view – Behaviorists believe that dissociation grows from normal memory processes and is a response learned through operant conditioning: • Momentary forgetting of trauma leads to a drop in anxiety, which increases the likelihood of future forgetting • Like psychodynamic theorists, behaviorists see dissociation as escape behavior – Also like psychodynamic theorists, behaviorists rely largely on case histories to support their view of dissociative disorders • Moreover, these explanations fail to explain all aspects of these disorders DISSOCIATIVE IDENTITY DISORDER • State-dependent learning – If people learn something when they are in a particular state of mind, they are likely to remember it best when they are in the same condition • This link between state and recall is called statedependent learning • This model has been demonstrated with substances and mood and may be linked to arousal levels DISSOCIATIVE IDENTITY DISORDER • Self-hypnosis – Although hypnosis can help people remember events that occurred and were forgotten years ago, it can also help people forget facts, events, and their personal identity • Called “hypnotic amnesia,” this phenomenon has been demonstrated in research studies with word lists • The parallels between hypnotic amnesia and dissociative disorders are striking and have led researchers to conclude that dissociative disorders may be a form of self-hypnosis DISSOCIATIVE IDENTITY DISORDER • People with dissociative amnesia often recover on their own – Only sometimes do their memory problems linger and require treatment • In contrast, people with DID usually require treatment to regain their lost memories and develop an integrated personality – Treatment for dissociative amnesia tends to be more successful than treatment for DID DISSOCIATIVE IDENTITY DISORDER • How do therapists help people with dissociative amnesia? – The leading treatments for these disorders are psychodynamic therapy, hypnotic therapy, and drug therapy • Psychodynamic therapists guide patients to search their unconscious and bring forgotten experiences into consciousness • In hypnotic therapy, patients are hypnotized and guided to recall forgotten events • Sometimes intravenous injections of barbiturates are used to help patients regain lost memories – Often called “truth serums,” the key to the drugs’ success is their ability to calm people and free their inhibitions DISSOCIATIVE IDENTITY DISORDER • How do therapists help individuals with DID? – Therapists usually try to help the client by: • Recognizing the disorder – Once a diagnosis of DID has been made, therapists try to bond with the primary personality and with each of the subpersonalities – As bonds are forged, therapists try to educate the patients and help them recognize the nature of the disorder » Some use hypnosis or video as a means of presenting other subpersonalities – Many therapists recommend group or family therapy DISSOCIATIVE IDENTITY DISORDER • How do therapists help individuals with DID? – Therapists usually try to help the client by: • Recovering memories – To help patients recover missing memories, therapists use many of the approaches applied in other dissociative disorders, including psychodynamic therapy, hypnotherapy, and drug treatment » These techniques tend to work slowly in cases of DID