A PowerPoint presentation capturing some of the most
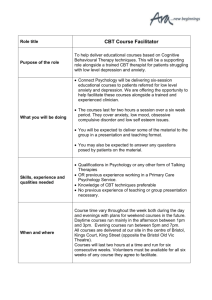
advertisement

Disorder specific models • • • • • • • Panic (Clark, 1986) Social Phobia (Clark & Wells, 1995) Health Anxiety (Salkovskis & Warwick, 1986) OCD (Salkovskis, 1994) GAD (Wells, 1997) PTSD (Ehlers & Clark, 2000) Depression (Beck, 1967) See also Core CBT Competencies list for recommended models: http://www.ucl.ac.uk/clinicalpsychology/CORE/CBT_Competences/CBT_Competences_Map.pdf © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com A vicious circle model of phobic anxiety Situational Trigger Physiological Behavioural Subjective Heart thumping Sweating Trembling etc. Running away “freezing” Shouting for help etc. “I might fall” “This is terrible” Fear, embarrassment etc. Symptoms Reactions Physiological Behavioural Subjective Heart thumping etc. Fatigue Avoidance, withdrawing from demanding or pleasurable activities “I can’t cope” “I must get out” Lowered confidence worry, frustration, fear © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com A cognitive-behavioural model for the maintenance of specific phobias Vomiting is unbearably awful and terrible for me Avoidance Encountering the phobic object / situation Catastrophic beliefs High degree of conviction Autonomic arousal Escape or safety behaviour The catastrophe does not occur and anxiety reactions dissipate Conclusion drawn: The escape / safety behaviour prevent the catastrophe The catastrophic belief is confirmed © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Pre-attentive activation The phobia remains unchanged Prevents disconfirmation A model of the development and maintenance of specific phobias Development Biological preparedness, disposition, developmental stage, culture, experience (classical conditioning, vicarious learning), memories/images, beliefs Assumptions With increased vulnerability to Trigger Frightening object or situation Anxious Cognitions (thoughts and images concerning stimulus) OVERESTIMATING THREAT AND CONSEQUENCES/ UNDERESTIMATING COPING AND RESCUE Anxious mood Physiological symptoms Increasingly anxious cognitions about external triggers Anxious cognitions about symptoms (fear of fear) Safety behaviours (related to anxious thoughts about external trigger) Safety behaviours (related to fear of fear) Secondary cognitions © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Depression, hopelessness, loss of confidence, low self-esteem Hyper vigilance about physical symptoms From Chapter 8 of Oxford Guide to Behavioural Experiments in Cognitive Behaviour Therapy (Kirk & Rouf) Cognitive model of social phobia [Clarks and Wells (1995) and Wells and Clark (1997)] Social Situation Activates assumptions a Perceived social danger (negative automatic thoughts) Processing of Self as a Social Object Safety behaviours © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Somatic & cognitive symptoms Wells, A., 1997. Cognitive Therapy of Anxiety Disorders: A Practice Manual and Conceptual Guide. Chichester: John Wiley & Sons Ltd. Cognitive cycle of fear for panic disorder Biological Vulnerability Stressful Events Alarm reaction Tachycardia, dyspnea, chest pain, depersonalisation etc. Increase in anxiety Increase in symptoms © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com F E A R Hyper surveillance Avoidance Anticipatory Anxiety Catastrophic thoughts “Oh, oh, oh..” “I’m gonna die, pass out” “Fall down, going crazy” Conduct Running away, escaping A cognitive model of OCD (Wells 1997, p.242) Trigger Activates Meta-Beliefs Appraisal of Intrusion Belief about rituals Behavioural Response © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Emotion Cognitive Model of OCD (Salkovskis) Neutralising actions (rituals, reassurances etc.) Intrusive thoughts, images, urges, doubts Attention and reasoning biases (looking for trouble) Misinterpretation of significance of intrusions – responsibility for actions Counterproductive “safety” strategies (though suppression, impossible criteria, avoidance etc.) © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Mood Changes (distress, anxiety, depression) 5 Part Cognitive Behavioural Therapy Model Environment Thoughts Emotions Behaviours Physical © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Cognitive Conceptualisation Diagram (Judith Beck, 1993) Relevant Childhood Data Core Belief(s) Conditional Assumptions/Beliefs/Rules Compensatory Strategies Situation 1 Situation 2 Situation 3 Automatic Thought Automatic Thought Automatic Thought Meaning of the A.T. Meaning of the A.T. Meaning of the A.T. Emotion Emotion Emotion Behaviour Behaviour Behaviour © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com A Cognitive Model of Hypochondriasis (Adapted from Salkovskis, 1989; Warwick and Salkovskis, 1990) Previous Experience Dysfunctional Schemas Formed Critical Incident Activates Schemas Negative Automatic Thoughts Cognitive Selective Attention Rumination Self-Focus Thinking Errors © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Anxiety Depression Anger Physiological Changes e.g Increased Arousal Bodily Sensations Sleep Disturbance Behaviour Reassurance Seeking Avoidance Bodily checking safety / prevention How did “the problem” develop? What made me vulnerable in the first place? Triggers for the most recent episode “The problem” Things that keep “the problem” going (These might include things that I do to control the problem) Positive things that I’ve got going for me © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com “The Vicious Flower” Cognitive Model of OCD (Salkovskis, Forrester & Richards, 1998) Early Experiences Making you vulnerable to OCD Critical Incidents What started the OCD off Activates Assumptions, General Beliefs E.G Not preventing disaster is as bad as making it happen Better safe than sorry Intrusive Thoughts, Images, Urges, Doubts Attention and Reasoning Biases Looking for trouble Neutralising Actions Rituals, reassurance, mental argument Misinterpretations of significance of intrusions – responsibility for action Counterproductive “Safety” Strategies Thought suppression, impossible criteria © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Mood Changes Distress, anxiety, depression Depression Model (Beck 1967, 1976) Early Experiences Core Beliefs and Assumptions Critical Incident Assumptions Activated Negative Automatic Thoughts Symptoms of Depression Behavioural Motivational © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Affective Cognitive Somatic Depression Increased hopelessness Loss of pleasure & achievement (Westbrook, Kennerley & Kirk, 2007) Depressed Mood More Negative view of self Reduced Activity Nothing Changes © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Reduced coping & problemsolving Negative thinking & Physical symptoms such as fatigue, poor concentration etc. Anxiety Maintenance (Westbrook, Kennerley & Kirk, 2007) Internal or external event 1. Perceived threat: Exaggerated and/or inappropriate 4. Fear remains intact: the alarming belief is unchanged 2. Client’s best attempt to protect him/herself from threat 3. Strategy gives shortterm relief, but fails to challenge the anxietyrelated belief © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Morrey, 2010 1. Automatic Negative thinking 3. Motivation and Physical symptoms Depression Mode Negative view of self, world and future 4. Unhelpful behaviours 5. Mood / emotion 6. Withdrawal and avoidance © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com 2. Ruminations and selfattacking DEPRESSION Cognitive-Behavioural Model of Body Dysmorphic Disorder (Veale, 2001) Trigger (e.g. reflection) Mirror-checking and selective attention Mirror checking Avoidance and safety behaviours to change or camouflage appearance Negative appraisal of internal body image Processing of self as an aesthetic object Mood (depression & disgust) Rumination on ugliness or “defectiveness” and comparison to ideal © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com What made me vulnerable in the first place Core Beliefs – about myself, others and the world Rules I live by… Helpful Unhelpful Current Problem What triggered the problem What helps me cope Helpful Unhelpful What maintains the problem now Thoughts Physical sensations Emotions Behaviours © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Cognitive Model of Postnatal Depression [Milgrom A., Martin P.R., Negri L.M (1999) Treating Postnatal Depression: A psychological Approach for Health Care Professionals. Wiley. Chichester. Adapted from Beck’s Cognitive Model of Depression (1979)] Vulnerability Factors Precipitating Factors, including Biological Factors Cultural Factors Post Natal Depression Exacerbating & maintaining factors Depression and other emotions Anxiety, Anger, Sadness Mediational Cognitive Factors Negative Automatic Thoughts Poor parenting self-efficacy (mediational = appraisal process) © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Behaviour / Coping Strategies Lethargy, Indecision, Social Withdrawal, Martial Conflict, Difficulty dealing with infant Diagnosis / symptoms Formative influences Situation / interpersonal issues Biological, genetic and medical factors Strengths / assets Typical automatic thoughts, emotions and behaviours Underlying schemas © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Working hypothesis Treatment Plan “Vicious Flower” Generic conceptualisation (Salkovskis, Warwick and Deal 2003) Anxiety Worry Processes Physical Sensations Images Threat Appraisal Meaning Selective Attention Safety Behaviours © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Memories Events, Stimuli, Situations Clark’s cognitive model of panic with maintenance cycles added (adapted from Clark, 1986) INTERNAL / EXTERAL TRIGGER PERCIEVED THREAT ANXIETY (Emotions) MISINTERPREATION © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com PHYSICAL / COGNITIVE SYMPTOMS AVOIDANCE AND SAFETY BEHAVIOURS (Including Selective Attention) A cognitive Model of GAD (Wells, 1995) Trigger Positive meta-beliefs activated (Strategy Selection) Type 1 Worry Negative meta- beliefs activated Behaviour © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Type 2 Worry (Meta-worry) Thought control Emotion Cognitive-behavioural model of generalized anxiety disorder [From Dugas, M.J., Gagnon, F., Ladoucer, R. & Freeston, M.H. (1998) Generalized Anxiety Disorder: A preliminary test of a conceptual model. Behaviour Research and Therapy, 36, 215-226] Situation What if..? Positive beliefs about worry Mood State Life Events Worry Negative problem orientation © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Anxiety Demoralization Exhaustion Cognitive avoidance The Bottom Line Assessment of worth/ value as a person Conclusions about the self, based on experience: this is the kind of person I am Rules for living Guidelines, policies or strategies for getting by, given the truth of the Bottom Line Standards against which self-worth can be measured Trigger Situations Situations in which the Rules for Living are, or may be, broken Activation of the Bottom Line Depression Negative Predictions Anxiety Self-critical thoughts © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Unhelpful behaviour Confirmation of the Bottom Line What keeps Low Selfesteem Going (Early) Experience Events, relationships, living conditions which have implications for ideas about the self How Low Self-esteem Develops Low Self-Esteem: A Map of the territory (Fennell, 1999) Based on Wells 1997, adapted by Stopa Social Situation 1. What went through your mind at that time? What was the worst you thought could happen? What did you think people would notice / think about you? What would that mean/ what would be so bad about that? Thoughts 3. As you became anxious, and thought that (feared event) might happen, did you do anything to try to prevent it from happening? Did you do anything to try to prevent people from noticing? Safety Behaviours 4. When you are afraid (feared event) will happened what happens to your attention? Do you become more self-conscious? As you focus on yourself, what do you notice? Do you have an image of how you feel you are coming across? What does that look like? Self-focus 5. As you did (safety behaviours) did that make you focus more or less attention on yourself? © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com 6. As you noticed yourself becoming more anxious, what effect did that have on your attention? 7. When you did (safety behaviours) what effect did that have on your anxiety? 2. When you thought (feared event) might happen, what did you notice happening in your body? (Suggest symptoms of anxiety) Anxiety Symptoms A. Ehlers., D.M Clarke. (2000) A Cognitive Model of posttraumatic stress disorder. Behaviour Research and Therapy 38, p. 319-345 Characteristics of trauma / Sequelae Prior Experiences/ Beliefs/ Coping State of individual Cognitive Processing during Trauma Influences Nature of Trauma Memory Negative Appraisal of Trauma and / or its Sequleae P E R S I S T E N T Matching Triggers Current Threat Intrusions Arousal Symptoms Strong Emotions Strategies Intended to Control Threat / Symptoms Arrows indicate the following relationships: Influences = Leads to = © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Prevents change in = P T S D A cognitive-behavioural model for the maintenance of specific phobias Various objects / situations are perceived as potentially harmful Avoidance Encountering the phobic object / situation Catastrophic beliefs High degree of conviction Autonomic arousal Escape or safety behaviour The catastrophe does not occur and anxiety reactions dissipate Conclusion drawn: The escape / safety behaviour prevent the catastrophe The catastrophic belief is confirmed © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Pre-attentive activation The phobia remains unchanged Prevents disconfirmation Maintaining Cycles • Safety Behaviours (e.g. OCD client) Fear/threat e.g. house burning down Failure to disconfirm threat (attributed to safety behaviour) © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Safety Behaviour e.g. repeated checking of appliances Maintaining Cycles • Reduced activity (depressed client) Depressed mood Negative Thoughts (What’s the point?’, ‘I can’t be bothered with anything’) Loss of Positive Rewards Reduced activity (Loss of sense of pleasure/social contacts) General reduction in achievement, activity levels, social withdrawal © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Maintaining Cycles • Perfectionism (e.g. depressed client) Negative self beliefs (e.g. I am worthless) Unable to achieve standards/derive satisfaction from achievement (‘Nothing I do is good enough’) © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Has high standards (‘If I don’t get 100% success in everything I do I’ve failed’) Maintaining Cycles • Catastrophic Misinterpretation (e.g. panic client) Symptoms e.g. heart racing, chest tight, breathless Increased anxiety Anxiety symptoms increased © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Misinterpretation ‘I’m having a heart attack’ Maintaining Cycles • Scanning/hypervigilence (e.g. health anxiety client) Worry about illness e.g. fear of cancer Sensations noticed or produced Interpreted as confirmation of illness ‘I might have a brain tumour’ © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Scanning/checking e.g. headaches Maintaining Cycles • Escape/avoidance (e.g. social anxiety) Feared situation e.g. parties, social gatherings Escape/avoidance Failure to change belief (Client continues to believe boring) © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com e.g. turn down invites, others see them as dull, where possible, avoid eye contact/talking to others if have to go Maintaining Cycles • Fear of fear (e.g. GAD client) Anxiety (any cause) Anticipatory fear of becoming anxious Aversive anxiety symptoms ‘I can’t cope with anything’ Heart racing, tense, nausea © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Maintaining Cycles • Performance Anxiety Worry about performance e.g. public speaking Apparent confirmation ‘I was right, I’m terrible at public speaking’ © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Anxiety symptoms affect performance e.g. hands shaking, speech hesitant, dry throat Maintaining Cycles • Self-fulfilling prophecies Negative beliefs about others Behaviour changes towards others (e.g. ‘Other people dislike me’) (e.g. appear tense/hostile, withdrawn) Apparent confirmation of negative beliefs/predictions © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Behaviour elicits negative response from others e.g. others appear uncomfortable, stop social approaches ‘Vicious Flower’ model (Salkovskis, Warwick & Deale, 2003) Images Emotion Worry Processes Memories Threat Appraisal/ Meaning Physical Sensations Safety Seeking Behaviours Events, stimuli, situations © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Selective Attention ‘Vicious Flower’ model (Salkovskis, Warwick & Deale) Anxiety; panic Rumination; thinking over past events (what went wrong) and rehearsing future ones (what to say, etc) Standing in the corner at party, looking odd, wild staring eyes, drenched in sweat. People laughing and pointing People think I am weird; I will end up rejected and alone Sweating, restlessness, shaky hands © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Parties, social occasions, memories of social events School – called ‘weirdo’. Ignored. Told I had staring eyes. Mocked Focus on self & how I appear. Ignore any friendly remarks from others (‘just being kind’) Hold arms down to hide sweat; avoid eye contact. Avoid parties or stay in kitchen out of the way & leave early. Cross road to avoid people. Look at road. Keep eyes semi-closed 6 Cycles Maintenance Model – A ‘Vicious Flower’ for Depression (Moorey, 2010) 1. Automatic negative thinking 6. Motivation and physical symptoms 2. Ruminations & self attacking Depression Mode 5. Unhelpful behaviours © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Negative view of self, world & future 4. Withdrawal and avoidance 3. Mood/emotion Longitudinal Formulation Depression: Early experience Core beliefs/assumptions Critical Incident(s) Activation of beliefs/ assumptions Negative Automatic Thoughts (NATs) Feelings © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Physical Behaviour Longitudinal Formulation Depression: Deprived of affection; Lack of attention vs. siblings There’s something wrong with me; I’m unlovable Break up of relationship Activation of beliefs/ assumptions I’m unlovable, If I get into relationship it goes wrong Upset © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Lethargic, heavy Withdraw Longitudinal Formulation Anxiety: Learning Experience Danger Schemas Formed Critical Incident Schema Activated Negative Automatic Thoughts Anxiety Symptoms Behavioural Responses Cognitive Biases © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com Generic cognitive theory of anxiety disorder Ref: Wells, A. (2007) Cognitive Therapy of Anxiety Disorders. Chichester: John Wiley & Sons Longitudinal Formulation Anxiety: Learning Experience Generic cognitive theory of anxiety disorder, Wells, A. (2007) Cognitive Therapy of Anxiety Disorders. Chichester: John Wiley & Sons Danger Schemas Formed The world is dangerous; people will harm me; I am vulnerable; worrying keeps me safe Critical Incident Neighbour’s house burgled Schema Activated I will be next; I need to get more locks; I need to have the police’s number handy; what if it happens when I’m alone at night? Heart pounding; rapid breathing; sweating; restless; racing thoughts; rumination Behavioural Responses Cognitive Biases © Think CBT Ltd. info@thinkcbt.com 01732 808 626 www.thinkcbt.com The world is dangerous (& I am vulnerable) Negative Automatic Thoughts Anxiety Symptoms Plan escape routes & location of weapons; check locks frequently; have mobile by bed; buy alarm system Highly anxious mother: not allowed out alone until age 16; fear of abduction, etc) Selective abstraction (neighbour’s house less secure) Catastrophising