Hemodialysis and Hemofiltration - Pediatric Continuous Renal
advertisement

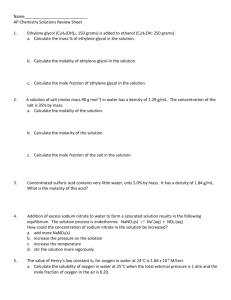
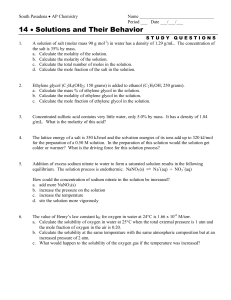
Hemodialysis and Hemofiltration in Pediatrics: An Approach to Intoxication Karen Papez MD University of Michigan Pediatric Nephrology, Dialysis & Transplantation 3rd annual PCRRT, Orlando, FL 2002 Annual Report of American Association of Poison Control Centers Nearly 2.4 million human exposures reported by 64 participating poison centers in 2002. 4.9% increase from 2001 Children <3 yrs: 39% of all human exposures Children <6 yrs: 51.6% of all exposures *Pediatricians and pediatric subspecialists need to be prepared to handle the majority of poison exposures. Watson WA et al. Am J Emerg Med 21: 2003 Litovitz TL et al. Am J Emerg Med 20: 2002 Enhanced Elimination Techniques for Poisonings Enhanced elimination techniques were used for 1457 cases (0.06%) in 2002. A near 8% increase over 2001 reports Hemodialysis: 1400 [up 9% from 2001] Hemoperfusion: 30 [down 33% from 2001] Other Extracorporeal Procedures: 27 *Pediatric nephrologists and intensivists need to be equipped with advanced techniques to handle such clinical situations. Treatment Measures Available for Poisonings Enhance Elimination (Cont.) Extracorporeal Methods Hemodialysis Standard High Efficiency/High Flux Hemofiltration Hemoperfusion Exchange Transfusion Plasma exchange Toxin Clearance What effects clearance? Volume of distribution Whether or not the drug is primarily renally excreted (competing pathways) Protein binding Molecular size of the drug Mode of therapy-HD, CVVH vs CVVHD vs CVVHDF Hemofilter membrane properties Pond, SM - Med J Australia 1991; 154: 617-622 HEMODIALYSIS Optimal drug characteristics for removal: Relative molecular mass < 500 Daltons Water soluble Small Vd (< 1 L/Kg) Minimal plasma protein binding Single compartment kinetics Low endogenous clearance (< 4ml/Kg/min) Pond, SM - Med J Australia 1991; 154: 617-622 HEMOFILTRATION Optimal drug characteristics for removal: Relative molecular mass less than the cut-off of the filter fibres (usually < 40,000 daltons) Small Vd (< 1 L/Kg) Single compartment kinetics Low endogenous clearance (< 4ml/Kg/min) Pond, SM - Med J Australia 1991; 154: 617-622 Additional Factors when Considering Enhanced Elimination Methods Drug kinetics should be reviewed Note: Kinetics may differ in an overdose situation Valproic acid: 90% protein bound with nl levels Valproic acid: 70% bound at levels of 135 mcg/ml : 35% bound at levels of 300 mcg/ml *The higher the levels and the more unbound drug that exists, the more effectively it may be removed. Case 1 14 year old female with history of depression, found slurring words, intermittently confused in her bedroom. During period of lucency, told mother she drank something a schoolmate gave her to “get high.” States this was 18 hours before presentation to local ER. Physical Exam at Admission to PICU T 38.8 P 125 RR 32 BP 158/75 Wt 75 Kg Generally: GCS variable, from verbal response to voice to mild response to pain. HEENT: Pupils equally round, sluggishly reactive to light, mucous membranes dry Resp: Deep, tachypneic, clear to auscultation CV: RRR, no murmur, peripheral pulses 2/4 Abd: Soft, nondistended, hypoactive bowel sounds Laboratory Analyses 148 5.4 121 13 7 2.1 9.4 4.8 11.7 4.0 16.8 50.4 98 38 59 0.3 143 163 7.24 / 18 / 113 / 8 UA SG 1.015, pH 5, normal for all substrates AG 20 Calc osm 306 Serum osm 311 CPK 388 NH3 38 Ethanol negative Urine drug screen negative βhCG negative Salicylate <1 Acetaminophen <10 Ethylene glycol 24.2 Osmolality (mosm/K) Calculated Osmolality with Dialysis in Ethylene Glycol Intoxication Calculated osmolality Serum osmolality HD Started 315 CVVHDF Started CT-190 295 Prisma dialyzer Multiflo-100 BFR -HD 250 ml/min -CVVHDF 180 ml/min PO4 based dialysate 275 24 27 34 36 Hours After Ingestion 40 53 - 4L/1.73m2/hr Case 2 12 year old female with history of bipolar disorder had started an increased dose of lithium 6 weeks prior to admission. Was slurring her speech on morning of admission, and had irregular constant movements of her arms and legs. Physical Exam at Admission to PICU T afebrile P 82 RR 23 BP 104/46 Wt 33 Kg Generally: Confused, slurring speech HEENT: NC, AT, Mucous membranes moist Resp: Clear to auscultation CV: Regular rate and rhythm, no murmur Abdomen: Soft, normoactive bowel sounds Skin: Erythematous rash over abdomen Neuro: Athetoid movements as noted in HPI Laboratory Analyses 133 107 31 4.3 22 1.2 6.8 10.5 12.1 34.4 73 7.0 35 4.1 25 0.6 215 176 7.36 / 50 / 28 / 28 UA SG 1.010, pH 6.5, pro 1+, ket 2+, LE 1+, otherwise normal AG 4 CPK 939 NH3 38 Ethanol and volatile acids negative Urine drug screen negative βhCG negative Salicylate <1 Acetaminophen <10 Lithium 7.34 EKG First degree heart block, PR 188 ms, prolonged QTc 520 ms Lithium Concentration (mEq/L) Lithium Clearance on Dialysis Lithium 8 7 HD Started 6 5 4 3 CVVHD Started CVVHD Stopped 2 1 0 0 3 4 5 6 11 15 20 23 25 30 33 36 Time After Presentation (Hours) CT-190 Prisma dialyzer Multiflo-100 BFR -HD 250 ml/min -CVVHDF 180 ml/min PO4 based dialysate - 4L/1.73m2/hr Lithium Redistributes from Intracellular Compartment: Arrows indicate beginning and end of HD. A significant rebound in serum concentration occurred after a 5-hr HD treatment with recurrence of neurologic impairment. An additional 4-hour hemodialysis treatment was then begun. From Goldfarb DS in Goldfrank’s Toxologic Emergencies, 7th Ed. 2002 Hemofiltration May Attenuate Rebound Phenomenon! Pt #1 Pt #2 Pt #3 Li Therapeutic range 0.5-1.5 mEq/L HD started 10 CVVHD started 8 6 4 2 0 Hours After Presentation 24 12 6 5 0 Lithium concentration (mEq/L) CVVHD Following HD for Lithium Poisoning CT-190 (HD) Prisma dialyzer -Multiflo-60 (#1,2) -Multiflo-100 (#3) BFR- HD -pt # 1 200 ml/min -pt # 2 325 ml/min -pt # 3 250 ml/min BFR- CVVHD 200 ml/min - All 3 pts. PO4 Based dialysate at 2L/1.73m2/hr (#1,2) 4L/1.73m2/hr (#3) Drug MW [Daltons] H2O Sol % Prot Bound Vol of Distrib [L/kg] Endogenous Clearance Lithium 7 Yes 0 0.6-1.0 0.4 ml/min/kg Methanol 32 Yes 0 0.7 0.7 ml/min/kg Ethylene Glycol 62 Yes 0 0.6 2.0 ml/min/kg Salicylates 138 Yes 90%* 0.15-0.2 0.88 ml/min/kg Valproic acid 144 No 90%* 0.19-0.23 Tot 1.3 Free 0.13 ml/min/kg 1.1 ml/min/kg Theophylline 180 Yes 55% 0.4-0.7 0.65 ml/min/kg Phenobarb 232 No 24-60% 0.5 0.1 ml/min/kg Carbamazepine 236 No 75% 0.8-1.6 1.3 ml/min/kg Vancomycin 1486 Yes 10-50% 0.47-1.1 Conclusions High efficiency hemodialysis and hemofiltration may alter the current “treatment of choice”. Pediatric nephrologists need to be aware that more than one treatment option exists for many toxicology situations, and the modality selected should be that tailored to their patient’s needs. ACKNOWLEDGEMENTS THERESA MOTTES TIM KUDELKA BETSY ADAMS TAMMY KELLY ROBIN NIEVAARD DAVID KERSHAW PATRICK BROPHY OTHER ISSUES Optimal prescription Biocompatible filters - may increase protein adsorption Maximal blood flow rates (i.e. good access) Physiological solution (ARF vs non ARF) Potential removal of antidote Counter-current dialysate maximal removal of toxins Specific Antidotes Should be used adjunctively with supportive therapy. Examples: N-acetyl cysteine [for Acetaminophen] Benzodiazepines [for Flumazenil] Flumazenil [for Benzodiazepines] Naloxone [for Opiates] Calcium [for Calcium channel blockers] Atropine [for Acetylcholinesterase inhibitors] Fomepizole [for Ethylene glycol, Methanol, & Diethylene Glycol] Ethanol [for Ethylene glycol, Methanol, & Diethylene Glycol]