Pathophysiology of
Concussions
November 9, 2013
Jon Schultz, MD
UMKC Sports Medicine
Kansas City, Missouri
Learning Objectives
• Appreciate the historical progression of
concussion research
• Recognize the impact of concussions on
today’s society
• Describe our current understanding of
concussive pathophysiology
So what’s the big deal???
•
“Compared to the complexity of a brain, a galaxy is just an inert lump” physicist Sir Roger Penrose
•
“Concussion is considered to be among the most complex injuries in sport medicine to diagnose,
assess, and manage” McCrory et al, Consensus Statement on Concussion in Sport, Clin J Sport
Med Volume 23, Number 2, March 2013
•
Limited research abilities
•
ED visits for sports-related TBI has risen over the past 10 years
•
Post-concussive syndrome, malignant cerebral edema, & second impact syndrome
•
Worries of chronic traumatic encephalopathy and dementia in retired NFL players
“DINGS” MATTER
AJSM, Lovell et al (2004)
43 HS athletes with “Grade 1” concussion
Neuropsych testing 36 hrs after concussion
Statistically significant differences in memory and symptoms
compared to baseline
Conclusion:
Old standard RTP guidelines may be too liberal
MECHANISM OF INJURY
Rotational (angular) acceleration: diffuse shearing forces deep in brain causing axonal
injury
Translational (linear) acceleration: tensile (pulling apart) and compressive forces
resulting in focal brain injury
Rotational
Linear
Pathophysiology of concussion
“neurometabolic cascade”
Nuerotramsmitter release with massive depolarization of
neurons along with axonal stretch inury
Energy supply and demand mismatch
Ionic
disruption
Decreased
cerebral blood
flow
Metabolic
disruption
Giza and DiFiori
Mitochondrial
dysfunction
Increased inflammation and
axonal swelling
Neurotransmission
disruption
Window of vulnerability
Pathophysiology of Sports-Related Concussion: An Update on
Basic Science and Translational Research Jan • Feb 2011SPORTS HEALTH
Lateral fluid percussion for inducing a
concussion in the lab
Ionic and metabolic dysfunction
Cerebral microdialysis measured elevated levels of glutamate and potassium in
head-injured patients in the ICU. J Neurosurg.1998;89:507-518, 971-982.
Components of clinical MD catheter. 1, pump connector; 2, inlet tube; 3, MD catheter; 4, MD
membrane; 5, outlet tube; 6, microvial holder; 7, microvial for collection of microdialysate.
Tisdall M M , and Smith M Br. J. Anaesth. 2006;97:18-25
© The Board of Management and Trustees of the British Journal of Anaesthesia 2006. All rights
reserved. For Permissions, please e-mail: journals.permissions@oxfordjournals.org
Chefer V, Thompson A, Zapata A a
Shippenberg T
Overview of Brain Microdialysis
Curr Protoc Neurosci. 2009 April
Schematic representation of MD catheter in brain tissue.
Tisdall M M , and Smith M Br. J. Anaesth. 2006;97:18-25
© The Board of Management and Trustees of the British Journal of Anaesthesia 2006. All rights
reserved. For Permissions, please e-mail: journals.permissions@oxfordjournals.org
Na+ influx
pH↑↓
Matthew F. Grady, MD, et al, Pediatric Annals, September 2012 - Volume 41 · Issue 9
Changes in LPR in ‘at-risk’ (a) and normal (b) brain during a period of low and normal CPP.
The normal range for LPR is shown by the shaded area.
Tisdall M M , and Smith M Br. J. Anaesth. 2006;97:18-25
© The Board of Management and Trustees of the British Journal of Anaesthesia 2006. All rights
reserved. For Permissions, please e-mail: journals.permissions@oxfordjournals.org
Human evidence
• After human TBI, positron emission tomography (PET)
scanning has shown a similar pattern of early
hyperglycolysis followed by glucose metabolic depression.
J Head Trauma Rehabil. 2001;16:135-148, J Neurosurg.
1997;86:241-251.
• Profound glucose metabolic depression was seen after mild
TBI, to the same degree as severe TBI. J Neurotrauma.
2000;17:389-401.
• Metabolic recovery generally takes weeks to months after
moderate to severe TBI. J Head Trauma Rehabil.
2001;16:135-148.
Pathophysiology of concussion
“neurometabolic cascade”
Neurotramsmitter release due to massive depolarization
of neurons and axonal stretch inury
Energy supply and demand mismatch
Ionic
disruption
Decreased
cerebral blood
flow
Metabolic
disruption
Giza and DiFiori
Mitochondrial
dysfunction
Increased inflammation and
axonal swelling
Neurotransmission
disruption
Window of vulnerability
Pathophysiology of Sports-Related Concussion: An Update on
Basic Science and Translational Research Jan • Feb 2011SPORTS HEALTH
So now what do we do???
Motor
cortex
Forced overuse within the first week of
experimental injury actually worsened the
animal’s recovery, causing greater cell death in
the brain and hampering neurologic recovery.
Exp Neurol.1999;157:349-358. Brain Res.
1998;783:286-292. J Neurosci. 1996;16:47764786.
Good legs
Delay forced overuse
Delay overuse by 1 week, and neurologic
recovery was more complete. But the amount
of cell death was not affected. Brain Res.
1991;561:106-119.
Voluntary exercise
If the animal runs within 1 week of a mild
injury, BDNF levels do not increase and
cognitive performance suffers. Neuroscience.
2004;125:129-139.
BDNF = brain-derived neurotrophic factor
What we know in the rat post-injury
• Period of vulnerability to premature activation
= known abnormal metabolic state after
experimental TBI = 7 to 10 days. Brain Res.
1991;561:106-119.
• A 2nd TBI within 3 to 5 days after the first =
impaired cognitive function but not when the
second injury was applied at 7 days.
Neurosurgery. 2005;56:364-374.
Does this apply to humans?
It appears so…
95 student-athletes (80 males, 15 females: age = 15.88 +/- 1.35 years) with
“moderate” postconcussive activity fared the best on neurocognitive testing. The
higher and the lower activity levels were associated with the worst scores. J Athl
Train.2008;43:265-274.
College football players
• With a history of concussion were 3.4 times more likely
to suffer a concussion that season.
• 6.5% of football players had a repeat injury in the same
season
• 75% (9 of 12) had a recurrent injury within 7 days of
the first injury, and 11 of 12 recurred within 10 days.
• The risk for repeat injury appears to be greatest within
10 days following the initial concussion.
Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated
with recurrent concussion in collegiate football players: the NCAA
concussion study. JAMA. 2003;290:2549-2555
Rats and CTE
• Molecular markers associated with dementing
processes
• Alzheimer disease is characterized by
accumulation of tau and amyloid β (Aβ)
protein
• Rodents do not readily develop Aβ plaques
• Apolipoprotein (Apo) E4 allele may be a
genetic marker making certain individuals
more susceptible to dementia
Tau
protein
Apo E4
Amyloid β
SYMPTOMS OF CONCUSSIONS
Headache
Nausea
Balance problems/dizziness
Fatigue
Drowsiness
Feeling “in a fog”
Difficulty concentrating
Difficulty remembering
Sensitivity to light
Sensitivity to noise
Blurred vision
Feeling slowed down
Randolph, et.al. Arch. Clin. Neuropsychol. 2009
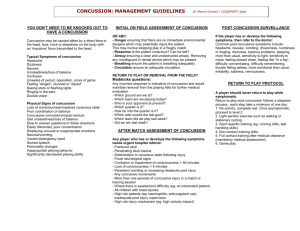
RETURN TO PLAY ISSUES
A player with diagnosed concussion should not be allowed
to return to play on the day of injury.
Occasionally, in adult athletes,
return to play on the same day as the injury may be allowed.