Acquired Brain Injury Unit - Brain Injury Association of Kentucky
advertisement
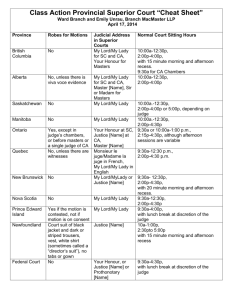
TREATING AT-RISK BEHAVIORS AT THE ACQUIRED BRAIN INJURY (ABI) UNIT AT EASTERN STATE HOSPITAL LINDSEY JASINSKI, PH.D. ABI PROGRAM DIRECTOR OBJECTIVES • Provide an overview of the new ABI unit at ESH • Discuss approaches to management of at-risk behaviors at ESH • • • • Staff Training Unit Structure Environmental Management Medical Interventions • Future Goals and Directions of ABI Unit MISSION AND VISION • Promote the highest level of functioning and quality of life through a systematically applied and comprehensive set of empirically supported medical and therapeutic rehabilitative interventions • Provide individualized, holistic, and compassionate post-acute brain injury rehabilitation in a safe environment • Focus on learning or re-learning new skills to improve functional independence, and transition to a lower level of care, including the community OVERVIEW • 17 beds • Locked, secure unit • Private & Semi-private rooms • 24-hour nursing care • Licensed as a Long-Term Care Facility • Anti-ligature hardware, focus on resident safety • Opened in late Fall 2014 ADMISSION CRITERIA INCLUSION CRITERIA • • • • Age 18+ History of Acquired Brain Injury Current Axis I diagnosis Meets nursing level of care, unsuccessful in less restrictive care • PASSR Level II • Rancho V or higher • Able to participate in at least 3 hours of therapy/day EXCLUSION CRITERIA • • • • • • Active felony for violent offense Primary substance abuse dx Any injury without known ABI (e.g. spinal cord) Dx of progressive dementia Psychiatric dx with no known ABI Intellectual disability or developmental disorder w/o etiology to ABI ADMISSIONS PROCESS • Referral • Review by the Admissions Committee Team • In Person visit • PASRR Level 1 and 2 • Scheduled admission date OUR TEAM ABI SPECIFIC TEAM • Medical Director, Board Certified in Neurology/Psychiatry • Physical Medicine/Rehabilitation Specialist ESH SERVICES • Music Therapist • Art Therapist • Registered Dietician • Chaplain • Quality Control • Infection Control • Neurologist • Neuropsychologist • Business Services • Clinical Psychologist • Utilization Review • Clinical Social Worker • Medical Supply • Safety/Environmental Services • Security • Laboratory • Health Information Management • Behavior Analyst • Physical Therapist • Speech/Language Pathologist • Occupational Therapist • Information Systems • Recreation Therapist • Pharmacy • Registered Nurses • Radiology • • Risk Management State Registered Nurse Aids TREATMENT TEAM APPROACH Multidisciplinary Interdisciplinary Transdisciplinary EXPECTED LOS 3-12 MONTHS Admission/Transition (goal development, motivation/engagement) Intensive Rehabilitation (PT, OT, SLP, Psy) Increased Community Integration Focus (Outings, expanded therapy) Transition to Community with Supportive Services AT RISK BEHAVIORS • Aggression/Violence • • • • • • • • Toward self: self-harm, suicidal ideation, suicide attempts Toward others: residents and staff Sexual Acting Out Personality Change/Irritability Emotional Lability Therapy Refusal Elopement attempts Other behaviors that interfere with progress in therapy or functional independence ESH PHILOSOPHY/MODEL Risk Need Responsivity TARGET AREAS FACTORS OFTEN CONTRIBUTING TO AGGRESSION & AT RISK BEHAVIORS • • • Decreased structure • • • Environmental triggers Staff attention less available Difficulty with communication and/or coping Poor task persistence/motivation Staff inexperience/ineffective ESH RESPONSE • • • • • Highly structured daily schedule Low staff to resident ratios Intensive Group and Individual Therapy Behavioral Support/Level System Errorless Learning, Goal Attainment Feedback Loop • Calming Rooms, Outdoor Space • P.E.A.R.L, CPI, GIV program DAILY SCHEDULE 7:25a 8:00a 8:30a 8:45a 9:00a 9:30a 10:00a 10:30a 10:45a 11:00a 11:25a 12:00p 12:30p 1:00p 1:30p 2:00p 2:30p 3:00p 3:30p 4:00p 4:30p 5:00p 5:30p 6:00p 6:30p 7:00p 7:30p 8:00p 8:30p 9:00p 9:30p 10:00p 10:30p Monday Breakfast Tuesday Breakfast Wednesday Breakfast ADLs ADLs ADLs Yoga/Stretch Yoga/Stretch Yoga/Stretch Goals Group Goals Group Goals Group Chaplain Group Chapel Lunch Lunch Lunch Mobile Library Mindfulness Gift Shop Thursday Breakfast ADLs Library Yoga/Stretch & Goals Saturday Breakfast Sunday Breakfast ADLs Relax/ADLs Relax/ADLs ADLs ADLs Yoga/Stretch Yoga/Stretch Goals Group Goals Group Lunch Lunch Mindfulness Mindfulness Gym and Reel Life Gym and Reel Life Dinner Dinner HW/Relax/Visitation HW/Relax/Visitation Wrap up Group Wrap up Group ADLs/lights out ADLs/lights out Yoga/Stretch & Goals Music/Art Therapy Gift Shop Cooking Group Mindfulness Weekly Outing Shopping/Meal Plan Friday Breakfast Lunch Communication Station Retrain your Brain Healthy Living Group Check in Group Double Trouble/Drug Ed Family Ties Group Feelings Group I am a Survivor Group On unit exercise Mindfulness Recreation Therapy Gym/Exercise Recreation Therapy Gym/Exercise Dinner Dinner Dinner Dinner HW/Relax/Visitation HW/Relax/Visitation Gym/Exercise Gym/Exercise Wrap up Group Wrap up Group Wrap up Group Wrap up Group Wrap up Group ADLs/lights out ADLs/lights out ADLs/lights out ADLs/lights out ADLs/lights out Dinner HW/Relax/Visitation HW/Relax/Visitation AA Group Gym/Exercise GROUP & INDIVIDUAL THERAPY FOCUS • • • • • • • • • • • Distress Tolerance, including Anger Management and Safe Coping Social Skills Acquisition Emotion Regulation Mindfulness Communication Skills Family Support and Education Development of Specific Goals related to psychiatric symptoms and coping Promote insight into triggering events, emotions Process incidents and use modified behavior chain analysis to explore alternatives REPETITION!!! Role Plays, In Vivo Training, In the moment coaching to use skills LEVEL SYSTEM • Begin on Level 1/2 at admission Level Privileges 5 Able to have personal computer, cell phone, Ipad use for 90 mins, Home visits 4 All outings (therapy/activity), Ipad use for 60 mins, able to use Wii 3 Therapeutic outings, soda and all snacks 2 Able to go off unit in hospital (e.g. gift shop), Level 1 snacks, no outings • 100 points = move to next level • Must maintain 20 points per day to remain on level 5 • -10 points in a day = drop 1 level • Behaviors (e.g. aggression, elopement, threatening, SAO, etc) = automatic drop to level 0 for safety 1 0 Able to have soda & level 1 snacks, can have radio, restricted to unit No technology (computer, cell phone), No outings, restricted to unit, level 0 snacks • Points awarded for therapeutic and daily functional activities: • • • • • Meal behavior and clean up Therapy – groups and individual Homework completion, if applicable Housekeeping ADLs • 2 points for full participation and appropriate behavior, 1 for partial, 0 for excused absence, -4 for refusal P.E.A.R.L. (MCMORROW, 2005) Positive Early Reinforce All Look P.E.A.R.L. CONTINUED… • Purpose: “encourage a different approach to influencing the lives of persons who are considered disabled, one that emphasizes the interaction between people as the basis of all human existence.” • Proactive Treatment Interaction—every interaction is a “social exchange” intended to promote greater autonomy • • • • Teaching, ways to invite greater participation Can take place anywhere, anytime Can occur regardless of level of functioning Promotes an ongoing interaction POSITIVE • Interaction is: • • • • Inviting Physical characteristics: warm tone, expression, posture Looks interested Upbeat, makes request (not command) and encourages interaction • Not a new skill, but reinforce in our staff, becomes self-reinforcing • Expectation of 2 positive/neutral statements for every 1 request EARLY • Have a social exchange before emotional/behavioral upset • Not just a “good idea” but rather a job expectation • Providing support and problem-solving early, prior to a difficult situation develops • Paying specific attention to antecedents for each individual • No behavior occurs in a vacuum • Learning (i.e. coping skills) is most likely to occur at low levels of arousal ALL • Use all components of PEARL, with all people, in all settings, all the time • Comprehensive approach to interactions, idealistic, inclusive • “Consistent reminder that we are interested in developing more powerful, mutually reinforcing relationships in our lives” • Based on mutual reciprocity, helps refocus staff • Sounds easy but in fact most individuals in our setting are there because of behaviors that are unacceptable in the community/home setting making the likelihood that “attack-attack reciprocity” will develop much higher REINFORCE • “Interact in a way that acknowledges more independent or autonomous behavior and is intended to result in increased future use of this behavior.” • Focus on what reinforces more functional behavior: verbal praise, touch, eye contact, tangible rewards • Also focus on what the desired outcomes are do we want this behavior to continue? • Reinforce-reinforce exchange: what part of the person’s behavior can you acknowledge? LOOK • Identify opportunities to teach as they arise, encourage independence and increase participation in the social community • Goes against the idea that “teaching” is specific to a particular type of interaction (i.e. didactic), specific discipline (e.g. psychology, SLP, OT, PT) or in a certain setting (e.g. group therapy). • Engages all staff to focus on what each interaction can produce, rather than imposing an agenda on the resident • “developing good therapy habits” as important for future functioning as the content of the session or interaction ERRORLESS LEARNING • Teaching method minimizing errors • Contrasted to Trial and Error Learning • Longer learning acquisition time • Used for cognitive retraining, but also for learning coping skills, ADLs, engaging in rehabilitation, etc. doesn’t allow for guessing or mistakes • Empirically supported for moderate to severe cognitive deficits after TBI • Improves learning, reduces depression/frustration/lack of motivation/anxiety associated with error correction process • Increased opportunity for positive reinforcement • Enhances engagement in rehabilitation process, develop good therapy habits, and improves rapport in early stages of intervention ERRORLESS LEARNING, EXAMPLES • Cognitive retraining: • Learn phone number for therapist number is 8167 the number is 816_ the number is 81_ _ the number is 8_ _ _ the number is ______ • Refusing rehabilitation: • Comprehensive task breakdown, points awarded for increasingly completing the steps over a period of time GOAL ATTAINMENT FEEDBACK • Daily goals group to start the day—maintains focus • Written on footprint as visual cue • Feedback given at lunch and dinner on level system and goals • Wrap up group in evening—process goal attainment • Visual cues also in binder relevant to other goals (e.g. cognitive goals, ADLs, etc.) CPI (NONVIOLENT CRISIS INTERVENTION) • • Crisis Prevention and Intervention Focus on De-escalation, Process each incident to re-focus on future • • • • • • • • C: Recognize lack of control O: Orient to the facts P: Identify patterns I: Investigate alternatives N: Negotiate, give choices G: Give back empowerment Physical interventions are a LAST resort to managing a crisis situation Staff highly training on staying calm, de-escalating the situation CPI, CONTINUED Anxiety Supportive Defensive Directive Acting Out Nonviolent Physical Intervention Tension Reduction Therapeutic Rapport CALMING ROOMS • In development, hospital-wide • Transdisciplinary approach with Psychology and OT • Focus on sensory and distraction tools for calming GIV PROGRAM • Individualized plan for giving the right patient, the right medication, at the right time. • Verbal de-escalation always attempted first, prompt to use effective coping • Effective and efficient utilization of PRN medication • Initial evaluation includes: • • • • Safety Crisis Management Assessment (SCMA)-triggers and coping What medications work and what dose? What route works best? At what point should medication be administered? Behavioral symptoms documented. • Benefits: • • • • Safe environment for everyone Decreased symptom burden Decreased number of incidents, including staff, peer, and resident injuries Allows staff to humanely intervene and respond effectively to a behavioral emergency SAFETY CRISIS MANAGEMENT ASSESSMENT Restraint Hours 1.6 1.4 1.38 1.28 1.13 1.2 1 0.84 0.8 0.56 0.6 0.31 0.4 0.2 0 -0.2 -0.4 Actual 3PMA 3PWMA Exponential jul 1.16 1.11 1.38 1.23 Actual aug 1.02 1.36 1.28 1.28 3PMA sep 0.61 1.33 1.13 1.24 3PWMA oct 0.35 1.19 0.84 1.17 nov 0.17 0.93 0.56 1.01 Exponential dec 0.11 0.66 0.31 0.81 Linear (3PWMA) SUMMARY • New unit: environment, culture and milieu very flexible, with solid foundation • Approach to managing at-risk behaviors is multifaceted • • • • Staff training through P.E.A.R.L. and CPI Highly structured therapeutic environment Focus on behavioral and environmental supports Maximize psychotherapeutic and medical interventions LOOKING FORWARD… • Continue clarifying our mission and vision, while meeting the needs of the community • Meet unit capacity, while maintaining highest levels of care and staffing ratios • Integration of ESH services with other providers, continuum of care • Research: What interventions have the biggest impact for what individuals? • Opportunities for additional research & training QUESTIONS???