Text File: The Role of Technology in the Medication
advertisement

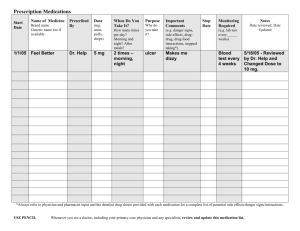
The Role of Technology in the Medication-Use Process Introduction Due to the numerous steps required in the care of patients, the healthcare industry is an inherently error-prone process that is fraught with opportunities for mistakes to occur. The healthcare industry must place safety as the national priority and work diligently toward this goal. Technology and Healthcare The majority of technology acquisitions have consisted of basic stand-alone computer systems, which were primarily used for data input to increase each department’s efficiency with financial accountability measures. But even as improving technology have emerged allowing for seamless integration of information to occur, most organizations have shown little interest or incentive to incur the huge costs associated with replacing their present nonintegrated computer systems. Influences on the Adoption of Technology Consumers have become increasingly concerned that hospitals are less than safe following the numerous mass media reporting of medical mistakes, which have resulted in patient harm and deaths. 1995 There were television and newspaper accounts that reported that tragic death of a patient from a preventable adverse drug event (ADE) due to an inadvertent administration of a massive overdose of a chemotherapy agent over 4 days. 1997 According to a 1994 American Medical Association report, medication errors related to the misinterpretation of physician’s prescriptions were the second most prevalent expensive claim listed on malpractice cases filed over a 7-year period on 90,000 malpractice claims between 1985 and 1992 (Cabral JDT, 1997). February 25, 2004 While CPOE technology purchases seemed to have plateaued, interest in the bar coding technology has dramatically increased due to the Federal Drug Agency’s (FDA) ruling, which requires medications to have machine-readable bar coding. Computerized Prescriber Order Entry (CPOE) Health Care practitioners still communicate information in the “old fashioned way”. There are many factors that demonstrate the need for a shift from a traditional paper-based system that relies on the unaided mind to automated order entry, record keeping, and clinical care. These factors include accessing patient information spread across multiple organizations that may be unavailable, especially in large organizations and, therefore, medical care would be provided without pertinent patient information. There are also many barriers that lead to ineffective communication to medication orders that include issues with illegible handwriting, use of dangerous abbreviations and dose designations, and verbal and faxed orders. Illegible hand-writing on medication orders has been shown to be a common cause of prescribing errors and patient injury and death have actually resulted from such errors (Brodell, 1993; Cabral, 1997; ASHP, 1993). Illegible orders may also lead to delays in the administration of medications. The use of CPOE system has the potential to alleviate many of these problems. CPOE can be defined as a system used for direct entry of one or more types of medical orders by a prescriber into a system that transmit those orders electronically to the appropriate department (AHA, 2000). CPOE systems offer many other advantages over the traditional paper-based system: They can improve quality, patient outcomes, and safety by a variety of factors Identifying patients needing updated immunizations or vaccinations, and suggesting cancer screening and diagnosis reminders and prompts. Reduction in the variation in care to improve disease management by improving follow-up of newly diagnosed condition. Reminder systems to improve patient management Automating evidence-based protocol Adhering to clinical guidelines, or providing screening instrument to help diagnosis disorder. Currently, the cost of providing health care is rising while reimbursement of services is declining. CPOE systems offer a variety of solutions to help reduce the cost of providing health care and making more appropriate utilization of services: 1. 2. 3. 4. 5. 6. 7. Reduction of hospitalization and decreased length of stay can be obtained from automated scheduling of follow-up appointments to reducing unnecessary diagnostic test. Better use of formulary and generis drugs by providing feedback of prescribing charges and patterns to encourage prescribers to substitute generics medications for more expensive branded medications. Properly designed systems can show improvement in work flow and time saving measures for prescribers Savings related to the storage of paper medical records could be substantial, compared to the costs of storing computerized backup storage devices. Entering medication and diagnostic orders into a computer system would allow for instantaneous capturing of charges and therefore enhancing revenue. Cost associated with the used of transcription notes would be eliminated as well by using electronic patient record system There is a patient and user satisfaction. CPOE systems have demonstrated a reduction in ADEs. Unfortunately, unsafe prescribing practices and medication errors are still possible with these systems. Errors in monitoring patient’s response to therapy can occur if the laboratory system is not interfaced with medication order entry system. It is important to have the ability to access past patient history, particularly previous AEDs and co-morbid conditions, yet some systems are unable to access prior patient care encounters. Problems may arise if drug information updates are not reformed on a timely basis or if this information is difficult to access. Medication errors such as wrong patient error, when the wrong patient is selected from a menu list of similar patient names; wrong drug errors, when the wrong medication is selected from a list due to look-alike similarity in either brand or generic name or orders intended for laboratory levels that are filled as medications can occur. CPOE systems will affect or even change the work of nurses in many ways, both negative and positive (AHA, 2000). First, like prescribers, these systems will require nurses to possess basic computer skills. Bar Code-Enabled Point-of-Care Technology Nurses play a vital role in the medication-use process, ranging from their involvement in the communication of medication orders to the administration of medications. One study showed that 38% of medication errors occur during the drug administration process (Leape et al, 1995). For more than 20 years bar code technology has clearly demonstrated its power to greatly improve productivity and accuracy in the identification of products in a variety of business settings, such as supermarkets and department stores proven to be an effective technology, it quickly spread to virtually all other industries. Additional levels of functionality can include some of the ff. features: Up-to-date drug reference information from online medication libraries Customizable comments or alerts Monitoring the pharmacy and the nurses’ response to predetermined rules Reconciliation for pending or STAT orders Capturing data for the purpose of retrospective analysis of aggregate data to monitor trends Verifying blood transfusion and laboratory specimen collection identification Negative effects include the following: Nurses are sometimes caught “off guard” by the programmed automated actions taken by the BPOC software The BPOC seem to inhibit the coordination of patient information between prescribers and nurses when compared to a traditional paperbased system Nurses found it more difficult to deviate from the routine medication administration sequence with the BPOC system Nurses felt that their main priority was the timeliness of the medication administration because BPOC required nurses to type in an explanation when medication even a few minutes late Nurses used strategies to increase efficiency that circumvented the intended use of the BPOC The use of BPOC systems can possibly introduce new types of medication errors such as the following: Omissions Extra dose Wrong drug Wrong dose Unauthorized drug Charting errors Wrong dosage form Automated Dispensing Cabinet Traditionally, hospital pharmacies provided medications for patients by filling patient-specific bins for unit dose medications, which were then delivered to the nursing unit and stored in medication carts. The ADC is a computerized point-of-use medication-management system that is designed to replace or support the traditional unit-dose drug delivery system. The devices require staff to enter a unique logon and password to access the system using a touch screen monitor or by using fingerprint identification. The rationales behind the wide acceptance of this technology are the following: Improving pharmacy productivity Improving nursing productivity Reducing costs Improving charge capture Enhancing patient quality and safety Some documented unsafe practices with the use of devices include: The lack of pharmacy screening of medication order prior to administration Choosing of the wrong medication from an alphabetic pick list High alert medications placed, stored, and returned to ADCs Storage of medications with look-alike names and/or packaging The development of “workarounds” Regardless of an organization’s steps to purchase or implement ADCs, the following issues should be considered to ensure safe medication practices: Consider purchasing a system that allow for patient profiling so pharmacists can enter and screen drug orders prior to their removal and administration Carefully select the drugs that will be stocked in the cabinets Place drugs that cannot be accessed without pharmacy order entry and screening individual matrix bins Use individual cabinets to separate pediatric and adult medications Periodically reassess the drugs stocked in each unit-based cabinet Remove only a single dose of the medication ordered Develop a check system to assure accurate stocking of the cabinets Place allergy reminders for specific drugs on the cabinets Routinely run and analyze override reports to help track and identify problems Implementation of Technology Implementing any form of technology into a healthcare organization can be an imposing task. The multidisciplinary team will need to address the following issues: Outlining goals for the type of automation to be implemented Developing a wish list of desired features and determining which one, given budgetary constraints, are practical Investigating systems that are presently available Analyzing the current workflow and determining what charges are needed Identify the required capabilities and configuration of the new system “Sell” the benefits and objectives of automation to staff Development of an implementation plan and set realistic timeframe expectations Conclusion As patient advocates, nurses have a responsibility to discuss their patient safety concern and speak up about the dangers associated with the current paper-based medication-used process. We also have the responsibility to become familiar with the availability of “safety” technology, the advantages and disadvantages, to work in collaboration with other healthcare stakeholders in the search for new and innovative technological solutions to improve patient safety.